Hollenhorst Plaque
- Article Author:
- Evan Kaufman
- Article Author:
- Navid Mahabadi
- Article Editor:
- Bhupendra Patel
- Updated:
- 8/10/2020 4:42:06 PM
- For CME on this topic:
- Hollenhorst Plaque CME
- PubMed Link:
- Hollenhorst Plaque
Introduction
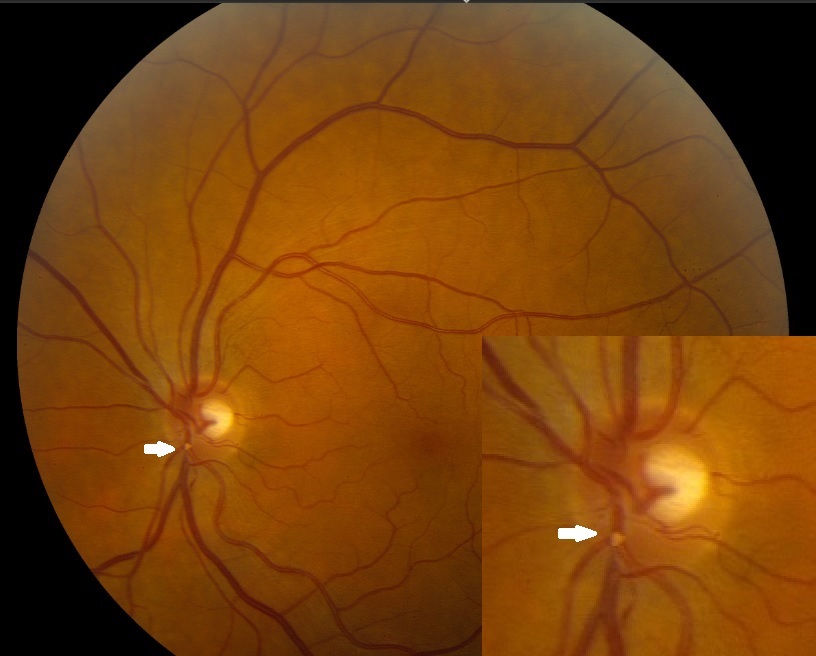
Stroke is the third most common cause of death in the United States. Eighty percent of all strokes are due to occlusion of a vessel secondary to atherothrombosis or embolus. Hollenhorst plaques were discovered in 1961 by Dr. Robert Hollenhorst. He defined them as emboli cause by plaques of cholesterol. The appearance of these emboli indicate that they are yellow, refractile, and typically located at an arterial bifurcation.[1][2]
Etiology
Hollenhorst plaques tend to originate from carotid arteries or the aorta. This finding is consistent with carotid disease originating from atherosclerotic lesions. The initial assumption, among eye care providers, upon discovering a Hollenhorst plaque is that it originated from the stenosed, ipsilateral internal carotid artery. The direct anatomical route between the internal carotid artery (ICA) and central retinal artery (CRA) supports this assumption. The ophthalmic artery is the first branch of the ICA, which then leads into the CRA.[3][4]
Epidemiology
The Blue Mountains Eye study stated the prevalence of retinal emboli is 1.4% in the general population older than 49 years old. The prevalence increases with age. Retinal emboli are significantly more prevalent in men than in women. Hollenhorst plaques make up the majority of the retinal emboli at 80%. An estimated 10% of carotid emboli reach the retinal arteries.[5]
Pathophysiology
Ulcerated plaques just distal to the bifurcation of the common carotid artery into its external and internal branches may be a source of retinal emboli that can be asymptomatic or produce transient monocular blindness.[6][7]
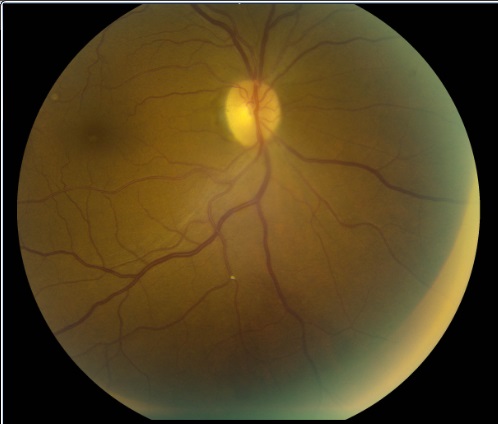
A Hollenhorst plaque is a clinical sign. It is commonly a contributing factor in the diagnosis of retinal artery occlusion (RAO). In order for a Hollenhorst plaque to cause an RAO, the plaque must completely obstruct the vessel. RAOs can occur in the central retinal artery (CRAO) or one of its branches (BRAO). Hollenhorst plaques are only one possible cause of a CRAO/BRAO and should not be thought of as synonymous. As discussed in the differential diagnoses, other types of emboli exist with the ability to occlude. There are also non-embolic causes of retinal artery occlusion including nocturnal arterial hypotension and transient vasospasm. Hollenhorst plaques, like other types of retinal emboli, may not stay in one place. The plaque may dislodge and move to a smaller diameter vessel before it gets lodged again, or the plaque may dissolve completely. The presence of a Hollenhorst plaque is a confirming diagnosis; however, the absence of a plaque does not rule out the possibility of embolic occlusion.
If an RAO takes place, the most common symptom is sudden, painless vision loss. The fundus will display typical ischemic signs such as retinal whitening around the occluded vessel. The macular area will remain “cherry-red” due to its secondary outer retinal blood supply.If the plaque is only partially occluding the vessel, blood can still flow through the lumen, and no damage is currently occurring. This partial occlusion is what was taking place with our patient. This does not mean an RAO cannot occur in the future. A single eye can undergo more than one transient RAO as documented by Hayreh et al. in their clinical study of over 250 patients. Unfortunately, what the literature shows is that asymptomatic Hollenhorst plaques are a poor predictor of future embolic events.
History and Physical
Hollenhorst plaques serve as markers of past emboli events but are poor predictors of future events. These plaques may or may not cause an RAO. The discovery of asymptomatic emboli has a greater concern for a patient’s systemic health than visual health.
Statistics
The prevalence increased with age: 0.8% visible in participants ages 49 to 60, 1.4% in ages 60 to 69, 2.1% in ages 70 to 79. This prevalence then dropped to 1.5% in the population over 80 years old.
Retinal emboli were significantly more prevalent in men compared to women: 67%. The presentation of a single embolism (88%) was more prevalent than a presentation of multiple emboli (12%). Lastly, the majority of the emboli were cholesterol (80%), followed by platelet-fibrin (14%) and calcific (6%).[8]
Evaluation
Ocular testing may involve fluorescein angiography (FA) as a supplemental test. Expected results for an occlusion include: delay in the retinal arterial filling, delayed arteriovenous transit time, and variable amounts of residual retinal circulation. It is very rare to see a complete lack of retinal filling even though the vessel is completely occluded. The choroidal filling should be normal since the occlusion has occurred anterior to the ophthalmic artery. There is also a restoration of retinal circulation within days/weeks after an RAO via anastomoses with the central retinal artery; therefore, an FA is of little benefit if delayed.[4][9]
Treatment / Management
Unless a Hollenhorst plaque completely obstructs a vessel causing an RAO, no ocular treatment is necessary. All patients with retinal emboli should be referred to the patient’s primary care provider for bilateral carotid duplex. Ocular testing may involve fluorescein angiography (FA) as a supplemental test.[10][11]
Differential Diagnosis
Calcific emboli: White, dull (non-refractile), due to their larger size typically found in the central retinal artery close to the optic disc. This finding is consistent with cardiac disease originating from heart valve calcifications.
Platelet-fibrin emboli: White/gray, dull (non-refractile), elongated. This can be a finding for both cardiac and carotid disease; however, cholesterol emboli are more common in carotid disease.
Talc emboli: Small, white/yellow, highly refractile, typically located in the macular region. This finding is associated with intravenous drug abuse.
Lipid/fat emboli: Usually cannot visualize the emboli, cotton wool spots are often seen. This finding is associated with long bone fractures and chest trauma, i.e., Purtscher retinopathy.
Tumor cells: These proliferative neoplastic cells which can fall off the main the main lesion and lodge in the retinal arterioles.
Septic emboli: These deposits are associated with bacterial endocarditis
Prognosis
Atheromatous disease of the internal carotid artery can be associated with these Hollenhorst plaques and is usually an indicator of potential stroke. Carotid stenosis increase in stroke risk as 1.18 times for every 10% increase in stenosis. This risk of stroke rises less than 1% per year for a vessel that is less than 80% stenosed. Whereas a vessel that is greater than 90% stenosed rises at 4.8% per year.
Complications
The most common complication is a stroke.
Pearls and Other Issues
Cholesterol emboli aka Hollenhorst plaque: Yellow, refractile, typically located at the carotid artery bifurcation. They tend to originate from carotid arteries or the aorta. This finding is consistent with carotid disease originating from atherosclerotic lesions.
- Hollenhorst plaques are considered to be the most common form of emboli
- Hollenhorst plaques are a common finding in the aging population
- Approximately 75% of Hollenhorst plaques seen in ophthalmic practice are asymptomatic
Enhancing Healthcare Team Outcomes
Even though there are several other causes of hollenhorst bodies, the most worrisome diagnosis is that of atherosclerosis of the internal carotid artery. Often the presence of a hollenhorst body is indicative of an impending stroke, especially in older individuals. Once a hollenhorst body has been diagnosed the management generally involves a neurologist, ophthalmologist, cardiologist, vascular surgeon, interventional radiologist, nurse, and a pharmacist, functioning as a cohesive interprofessional team. The patient should undergo a duplex ultrasound of the neck to determine the presence of atherosclerotic disease at the carotid bifurcation. If the lesion is ulcerated and more than 70% stenosis, the patient should be referred to the vascular surgeon or an interventional radiologist for stenting. The patient should be encouraged to lower his blood pressure and cholesterol, discontinue smoking and take aspirin while awaiting surgery. The nurse should educate the patient on the possible symptoms of a stroke and when to return to the emergency room. When patients with carotid artery atherosclerosis are managed with elective surgery or stenting, the morbidity and mortality rates are less than 3%. [4][9] THis type of interprofessional activity will drive improved results [Level 5]
(Click Image to Enlarge)