Hypopituitarism
- Article Author:
- Verena Gounden
- Article Editor:
- Ishwarlal Jialal
- Updated:
- 5/24/2020 11:19:57 PM
- For CME on this topic:
- Hypopituitarism CME
- PubMed Link:
- Hypopituitarism
Introduction
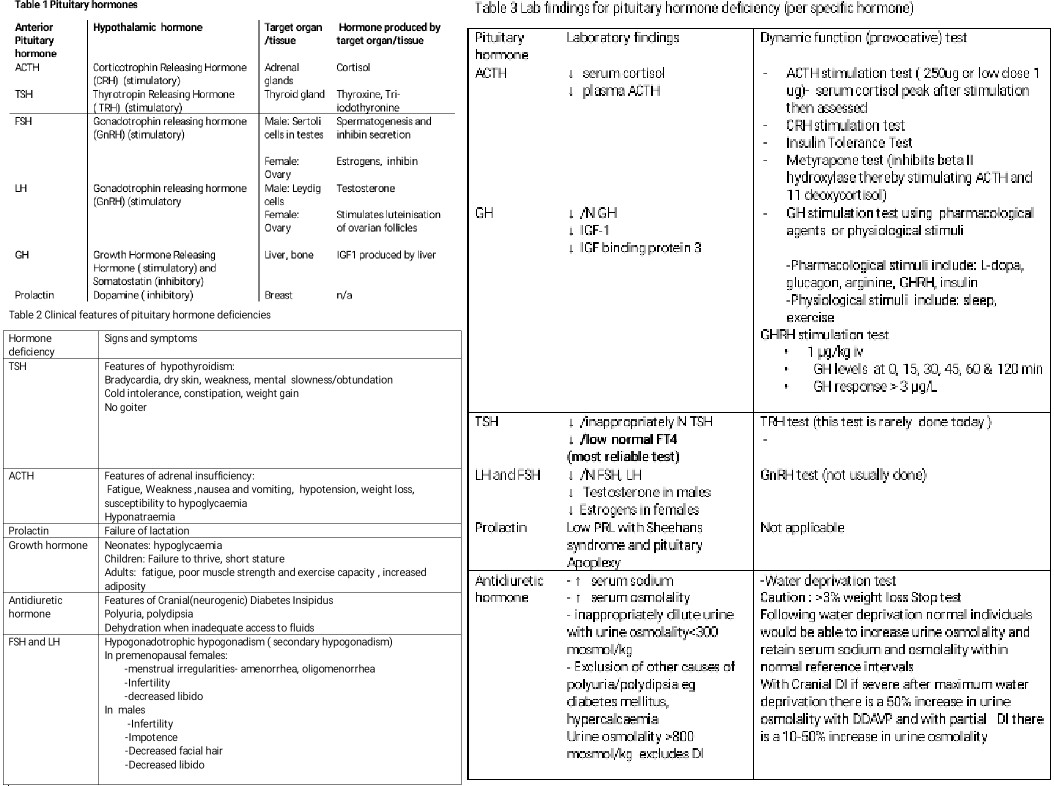
The pituitary gland is responsible for the production and secretion of various hormones that play a vital role in regulating endocrine function within the body. The pituitary gland consists of an anterior and a posterior lobe. Hormones produced by the anterior lobe of the pituitary gland include growth hormone (GH), thyroid-stimulating hormone (TSH), luteinizing hormone (LH), follicular-stimulating hormone (FSH), adrenocorticotropin hormone (ACTH), and prolactin (PRL). Hormones stored and released from the posterior pituitary are antidiuretic hormone (ADH)/vasopressin and oxytocin. ADH and oxytocin are produced by neurosecretory cells in the hypothalamus. Trophic hormones produced by the hypothalamus stimulate or inhibit the production of different anterior pituitary hormones which then affect target organs. See Table 1 (Anterior Pituitary Hormones).
Hypopituitarism is defined as a deficiency of one or more of the hormones produced by the pituitary gland. The presence of hypopituitarism is associated with increased mortality due to increased cardiovascular and respiratory diseases, and early diagnosis is important to prevent further morbidity due to the subtle presentation.[1][2][3]
Etiology
The causes of hypopituitarism can be attributed to either a pathology of the hypothalamus affecting the production of trophic hormones that act on the pituitary or direct pathology of the pituitary gland itself. The most common cause of hypopituitarism (61%) is the presence of pituitary tumors (both non-secretory and secretory). Pituitary tumors may cause the increased production of one hormone with resultant deficiency of the other pituitary hormones as in acromegaly (excess GH with hypopituitarism from the macroadenoma). Most pituitary tumors are benign and may be secretory or non-secretory. Secondary metastases originating from, for example, breast, colon, and prostate cancers do occur less commonly. Hypothalamic and para-pituitary tumors such as suprasellar meningiomas, gliomas, and craniopharyngiomas may also be associated with hypopituitarism. Other causes of hypopituitarism include injury to the pituitary gland following traumatic brain injury or iatrogenically during surgery or cranial irradiation.[4]
Inflammatory conditions of the pituitary may also be responsible for the occurrence of hypopituitarism. The infectious agents that can have been related to pituitary insufficiency include Mycobacterium tuberculosis and non-mycobacterial agents such as histoplasmosis, syphilis, viruses, and protozoa. Lymphocytic hypophysitis usually presents in the post-partum period as a mass lesion on magnetic resonance imaging (MRI) due to infiltration of the pituitary with lymphocytes and plasma cells and is responsive to steroid therapy.
Infiltrative diseases such as hemochromatosis, sarcoidosis, and histiocytosis may be associated with the development of hypopituitarism.
Pituitary apoplexy is a medical emergency and is due to acute ischaemic infarction or hemorrhage of the pituitary gland. Pituitary apoplexy may occur in the presence of a pituitary adenoma but may also occur in the normal pituitary gland. Sheehan syndrome refers to infarction of the hyperplastic pituitary gland during pregnancy due to severe blood loss (post-partum hemorrhage). Because of the rich and complex vascular supply, pituitary adenomas have an increased risk of bleeding when compared to other brain tumors.[5]
Congenital absence of the pituitary gland is related to the midline and craniofacial defects. Genetic mutations in transcription factors such as HESX1, PROP1, and Pit-1 can lead to congenital hypopituitarism. Empty Sella syndrome is a rare disorder which is characterized by enlargement or malformation of the sella turcica resulting in a herniation of the arachnoid membrane into the pituitary fossa dislodging the pituitary to the floor of the fossa. It is associated with a small or absent pituitary gland. Empty Sella syndrome may be idiopathic or occur secondarily to a treated pituitary tumor, head trauma, or a condition known as idiopathic intracranial hypertension (pseudotumor cerebri). Kallmann syndrome is a rare genetic condition associated with an inability to smell (hyposmia/anosmia) and hypogonadotropic hypogonadism (decreased FSH decreased LH, and reduced testosterone/estradiol) due to a mutation in the Kal1 gene as the commonest genetic abnormality in males.
Epidemiology
There is limited data available regarding the incidence and prevalence of hypopituitarism, and it is placed in the category of rare disorders by the National Institute of Health (NIH). One study from Northwestern Spain conducted by Regal et al. reported a prevalence of 45.5 cases per 100,000 population.[6][7]
History and Physical
It appears that 75% of the pituitary needs to be damaged to result in hypopituitarism. Clinical features of hypopituitarism may be subtle and ill-defined or severe with the acute presentation. Conditions such as Sheehan syndrome/pituitary apoplexy, pituitary infection, hypophysitis, and traumatic brain injury present with acute findings. [8][9][10]
Presenting signs and symptoms may be linked to that of a deficiency of the pituitary hormone, mass effects in the presence of pituitary tumors, and/or features of the causative disease.
Patients with hormonal deficiencies present with the following:
- ACTH deficiency - Adrenal insufficiency
- TSH deficiency - Hypothyroidism
- Gonadotropin deficiency - Hypogonadism
- GH deficiency - difficult to thrive and short stature in children. Adults are usually asymptomatic; however, they may feel fatigued and weak.
- ADH deficiency - Polydipsia and polyuria
Mass effects include visual field defects known as bitemporal hemianopsia. Visual field defects may also occur unilaterally. Patients may also present with headaches, secondary to the mass lesions. See table 2 below. It summarises the clinical features of pituitary hormone deficiencies.
Physical examination may not reveal any significant findings as the presentation is usually subtle. Variable features may be present owing to the involvement of different target hormones, such as:
- Hypothyroidism - small and soft thyroid gland, dry and coarse skin, thinning of hair and alopecia, delayed tendon reflexes, cold skin with loss of sweating, and non-pitting type edema
- Adrenal insufficiency - buccal hyperpigmentation and postural hypotension in cases of Addison disease
- Hypogonadism - small and atrophied testes in men. Loss of axillary and pubic hair in women.
- Neurological and ophthalmic involvement - loss of visual acuity, extraocular paresis, and bitemporal hemianopsia
- GH excess - in functioning adenomas may result in features consistent with acromegaly.
Evaluation
The presence of a secretory pituitary tumor may result in features of hormone excess for the particular hormone produced by a tumor while other pituitary hormones may be deficient.[11][12][13][14]
Investigations
Laboratory Investigations: Initial testing involves baseline levels of pituitary hormones and hormones produced by target glands. Due to the variation of hormone levels related to the time of day, season, and pulsatile secretion of certain pituitary hormones, baseline levels may not be helpful. In this instance, dynamic function testing may be performed to confirm biochemical deficiency or excess of a particular pituitary hormone. In dynamic function testing, for the investigation of a hormone deficiency, a stimulatory agent that would normally increase secretion of the hormone is given to the patient and blood levels are measured before and after the administration of the agent. After the administration of this stimulant, measurements are taken at defined intervals to determine if there has been an adequate response to stimulation. See Table 3. Lab findings for pituitary hormone deficiency (per specific hormone).
Insulin Tolerance Test: This is the best provocative test that is used to assess the presence of the deficiency of both GH and cortisol. Following an overnight fast, baseline samples are obtained for cortisol, GH, and glucose. An insulin dose of 0.1 U/kg or 0.05 U/kg is administered intravenously (IV). Further samples for analysis of the hormones measured in the baseline samples are then taken at several other time points after administration. It should not be performed in those with cardiac disease or epilepsy. The plasma glucose should fall to 40 mg/dl within 30 to 45 minutes or by 50% of baseline. The test is terminated by giving IV dextrose and assessing the patient's status for at least 90 minutes. A normal/adequate response is indicated by cortisol of more than 20 ug/dL and GH of more than 5 ng/mL to 10 ng/mL.
Modern Combined Test: The patient is given growth hormone-releasing hormone (GHRH), cortisol releasing hormone (CRH), gonadotropin-releasing hormone (GnRH), and thyroid releasing hormone (TRH) as the provocative stimuli and GH, TSH, ACTH, cortisol, LH, and FSH are measured at baseline and at specified time intervals after that. Doses of each stimulating hormone are as follows
- GHRH (1.0 ug/kg)
- CRH (1.0 ug/Kg)
- GnRH (100 ug)
- TRH (200 ug).
However, this testing is rarely required.
Radiological Investigations: Imaging studies of the pituitary using magnetic resonance imaging (MRI) with gadolinium enhancement are used to visualize the pituitary, in particular, to detect the presence of a mass lesion. Visual field defects need to be assessed if a pituitary mass is the cause of hypopituitarism.
Treatment / Management
Management is dependent on the cause of hypopituitarism. Initial treatment is to address the underlying cause of hypopituitarism. Mass lesions may be removed surgically, and other medical conditions treated accordingly. Many patients may require hormone replacement therapy.
ACTH Deficit: Corticosteroid replacement should be initiated before the replacement of the thyroid hormone to avoid precipitating an adrenal crisis. Hydrocortisone at a dose of 10 mg to 20 mg in the morning and 5 mg to 10 mg in the evening. Prednisone may also be used.
Increased dosages of corticosteroids are given during periods of stress, surgery, and pregnancy.
TSH Deficit: Thyroid hormone (L-thyroxine) replacement, in particular for the elderly and those with cardiac disease. It is important to start with a low dose of 25 ug/daily and then up-titrate as required according to biochemical findings, and clinical signs and symptoms.
FSH/LH Deficit: In secondary hypogonadism, testosterone can be delivered by gel, patch, or intramuscular (IM) injections every two weeks with careful monitoring of prostate-specific antigen (PSA) and testosterone levels.
In women: estrogen/progesterone hormone replacement therapy via oral, intramuscular, or transdermal routes can be given.
If fertility is desired, then one starts with human chorionic gonadotropin (HCG) to augment testosterone levels and improve semen quality. If this is not successful after one year, consider human menopausal gonadotropin (HMG)/recombinant FSH concomitant therapy to further enhance fertility.
Growth hormone deficit: Unlike in children with short stature due to GH deficiency, the role of GH replacement in the treatment of adult GH deficiency has not been well established. In children, synthetic growth hormone replacement is used for this purpose such as somatotrophin. Replacement therapy is titrated against IGF1 levels. The goal of treatment is to ensure that adult height is obtained. Further evaluation is made post-puberty to determine whether GH replacement should continue into adulthood.
ADH deficit: Replacement of ADH with intranasal desmopressin (synthetic vasopressin) helps stabilize water balance and polyuria.
Differential Diagnosis
A diagnosis of hypopituitarism may be missed or delayed in complex situations where apparently normal pituitary hormone levels are misinterpreted in the context of suboptimal target organ hormone levels. However, adrenal insufficiency should be treated on the basis of clinical suspicion without waiting for the biochemical evidence.
Following are some differential diagnoses that may be considered while making a diagnosis of hypopituitarism:
- Primary hypothyroidism
- Kallman syndrome
- Pituitary macroadenomas
- Hyponatremia
- Polyglandular autoimmune syndrome type-1
- Polyglandular autoimmune syndrome type-2
- Polyglandular autoimmune syndrome type-3
Prognosis
Patients who are stable on hormone replacement, usually have a good prognosis. Mortality increases in patients with acute decompensation who are in a critical state.
Morbidity is variable and depends on the type of hormone deficiency. The systemic effects of hypopituitarism are also variable depending on the extent of pituitary involvement.
Some clinical states that result from the acute decline in pituitary production may lead to increased mortality risk, such as deficiency of ACTH leading to adrenal crisis or TSH deficiency causing myxedema coma and death.[15]
Deterrence and Patient Education
Patient education should mainly focus on the need for lifelong hormone replacement therapy, increased glucocorticoid dose during times of stress, and rapid medical access as appropriate. Regular monitoring to prevent inadequate or excessive replacement is crucial.
Patients with hypopituitarism should carry some form of identification with them. This can be in the form of a bracelet to be worn on the wrist or neck.
For emergency purposes, patients may also need to carry a vial of hydrocortisone 100 mg and a syringe at home and while traveling.
Enhancing Healthcare Team Outcomes
The diagnosis and management of hypopituitarism are done with an interprofessional team that consists of a neurosurgeon, endocrinologist, pathologist, radiologist, primary care provider, nurse practitioner, and an ophthalmologist. Management is dependent on the cause of hypopituitarism. Initial treatment is to address the underlying cause of hypopituitarism. Mass lesions may be removed surgically, and other medical conditions treated accordingly. Many patients may require hormone replacement therapy. The outcome in most patients with hypopituitarism is good, but those who have a neurological deficit may continue to have partial deficits even after treatment. [1][16][17](Level V)