Anatomy, Head and Neck, Eye Inferior Rectus Muscle
- Article Author:
- Caleb Shumway
- Article Author:
- Mahsaw Motlagh
- Article Editor:
- Matthew Wade
- Updated:
- 7/27/2020 12:46:16 PM
- For CME on this topic:
- Anatomy, Head and Neck, Eye Inferior Rectus Muscle CME
- PubMed Link:
- Anatomy, Head and Neck, Eye Inferior Rectus Muscle
Introduction
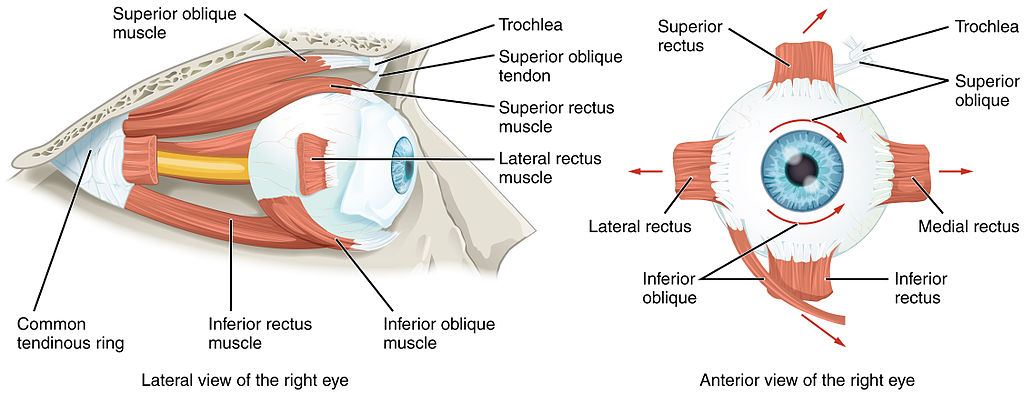
The inferior rectus is one of the seven extraocular muscles and is primarily responsible for depressing the eye (downgaze). The inferior rectus is one of the four rectus muscles, which also include the superior rectus, the medial rectus, and the lateral rectus. There are also two oblique muscles, the superior and inferior obliques. The seventh extraocular muscle is the levator palpebrae superioris.
Structure and Function
With head facing straight and the eyes facing straight ahead, the eyes are said to be in primary gaze. From this position, an action from an extraocular muscle produces a secondary or tertiary action. Although the globe can be moved about 50 degrees from primary position, usually during normal eye movement only 15 degrees of extraocular muscle movement occurs before the head movement begins.
The annulus of Zinn is the common site of origin of the rectus muscles and spans the superior orbital fissure. It consists of superior and inferior tendons. The superior tendon is involved with the entire superior rectus muscle as well as portions of the medial rectus and lateral rectus muscles. The inferior tendon is involved with the inferior rectus muscle and portions of the medial rectus and lateral rectus muscles.
The inferior rectus has a primary action of depressing the eye, causing the cornea and pupil to move inferiorly. The inferior rectus originates from the Annulus of Zinn and courses anteriorly and laterally along the orbital floor, making an angle of 23 degrees with the visual axis. This angle causes the secondary and tertiary actions of the inferior rectus muscle to be abduction and extorsion (excycloduction).
Each of the extraocular muscles has a functional insertion point, which is at the closest point where the muscle first contacts the globe. This point forms a tangential line from the globe to the muscle origin and is known as the arc of contact. The inferior rectus inserts in the vertical meridian, approximately 6.5 mm from the limbus. [1]
Embryology
The mesenchyme of the head, including the orbit and its structures, arise in mesoderm and neural crest cells primarily. The extraocular muscles originate from mesoderm, but the satellite and connective tissue of the muscle derive from neural crest cells. Most of the remaining connective tissue of the orbit also is derived from neural crest cells.
Blood Supply and Lymphatics
The inferior rectus receives blood primarily from the inferior muscular branch of the ophthalmic artery, with secondary contribution from the infraorbital artery. The primary blood supply for all of the extraocular muscles are the muscular branches of the ophthalmic artery, the lacrimal artery, and the infraorbital artery. The two muscular branches of the ophthalmic artery are the superior and inferior muscular branches.
Venous drainage is similar to the arterial system and empties into the superior and inferior orbital veins. Usually, there are a total of four vortex veins, and these are found at the lateral and medial sides of the superior and inferior rectus muscles. These vortex veins drain into to the orbital venous system.
Nerves
The inferior rectus is innervated by the lower division of cranial nerve III (oculomotor). Cranial nerve III is divided into upper and lower divisions, with the upper division innervating the superior rectus, and levator palpebrae superioris, and the lower division to the medial rectus, inferior rectus, and inferior oblique. The lateral rectus is innervated by cranial nerve VI (abducens), and the superior oblique is innervated by cranial nerve IV (trochlear).
Additionally, the parasympathetic innervation of the sphincter pupillae and ciliary muscle travels with the branch of the lower division of cranial nerve III that supplies the inferior oblique, and this passes near the inferior rectus. This has important surgical considerations that will be explained further. [2][1]
Muscles
The inferior rectus and the superior rectus are vertical rectus muscles. The medial and lateral rectus muscles are the horizontal rectus muscles. Each of the rectus muscles originates posteriorly at the Annulus of Zinn and courses anteriorly.
Each of the rectus muscles inserts on the globe at varying distances from the limbus, and the curved line drawn along the insertion points makes a spiral that is known as the Spiral of Tillaux. Starting at the medial aspect of the globe, the medial rectus inserts at 5.5 mm from the limbus, the inferior rectus inserts at 6.5 mm from the limbus, the lateral rectus inserts at 6.9 mm from the limbus, and the superior rectus at 7.7 mm from the limbus.
The inferior rectus is 9.8 mm wide at its insertion on the globe. The tendon is 7 mm, measured from the origin. The entire length of the muscle is 40 mm.
Extraocular muscles have a large ratio of nerve fibers to skeletal muscle fibers. The ratio is 1:3 to 1:5, compared to other skeletal muscles which is 1:50 to 1:125. Extraocular muscles are a specialized form of skeletal muscle with a variety of fiber types, including both slow tonic types which resist fatigue and also saccadic (rapid) type muscle fibers. [3]
Physiologic Variants
The size of the inferior rectus muscle, as well as its insertion point on the globe from the limbus and other anatomical measurements, may vary widely from one individual to the next. The numbers described in this article reflect average distances.
Congenital differences in extraocular muscles can cause ocular misalignment. See the Clinical Significance section for more details regarding strabismus.
Surgical Considerations
Because the parasympathetic fibers to the sphincter pupillae and ciliary muscle travel with the innervation to the inferior oblique, and the inferior oblique crosses the inferior rectus laterally, there are potential complications from surgery in this area. If the parasympathetic fibers are damaged during surgery in this area, pupillary abnormalities may result.
The inferior rectus also interacts with the lower eyelid via a fascial connection from its sheath. Weakening or recession of the inferior rectus may widen the palpebral fissure, and this can cause lower lid droop. Conversely, strengthening or resection of the inferior rectus may cause the fissure to narrow and elevate the lower lid.
The nerves to rectus muscles and superior oblique muscles insert into the muscles at a one third the distance from the origin to the insertion. This makes damage to these nerves during anterior segment surgery difficult, but not impossible. Additionally, instruments that are advanced 26 mm posterior to the rectus muscle insertions can cause injury to the nerve.
Blood vessels may be compromised during surgery of the inferior rectus muscle. The vessels which supply blood to the extraocular muscles also supply nearly all the temporal half of the anterior segment of the eye. Most of the nasal half of the anterior segment circulation also derives from blood vessels that supply the extraocular muscles. Therefore, care must be taken during surgery of the medial rectus or other extraocular muscles to avoid disrupting this blood supply.
There are other complications which may result from inferior rectus surgery, which also may result from other rectus muscle surgery. Unsatisfactory alignment is the most common complication and may require additional surgery to correct this. Refractive changes may occur when two rectus muscles of one eye are operated, and this may resolve over months. Other possible surgical complications include diplopia, perforation of the sclera and postoperative infections. Although uncommon, serious infections may result after strabismus surgery, including pre-septal or orbital cellulitis and endophthalmitis.[4][5][6][7][8][9]
Clinical Significance
The function of the inferior rectus muscle can be assessed along with the other extraocular muscles during the clinical exam. The movement of the extraocular muscles can be assessed by having the patient look in nine directions starting with a primary gaze, followed by the secondary positions (up, down, left and right) and the tertiary positions (up and right, up and left, down and right, down and left). The clinician can test these positions by having the patient follow the clinician's finger trace a wide letter "H" in the air.
Further tests of ocular alignment can be tested further by several methods, including cover tests, corneal light reflex, dissimilar image tests and dissimilar target tests. Since many patients with extraocular muscle abnormalities are young children, the clinician may need to employ various clever means such as using toys or other objects to elicit the cooperation of the child.
Strabismus, or ocular misalignment, can be caused by abnormalities in binocular vision or abnormalities of neuromuscular control. Weakness, injury or paralysis that involves the inferior rectus muscle can be involved in strabismus.
Because the inferior rectus is near the orbital floor, orbital floor fractures may involve this muscle. Inferior rectus muscle paresis can result from trauma to the inferior rectus muscle or nerve. This can occur either at the time of initial injury or during surgical repair of the orbital floor. If inferior rectus muscle paresis is present without entrapment, the patient may display hypertropia in the primary position. If paresis is present with entrapment, the patient may have a little deviation or even slight hypotropia which decreases with downgaze. The management of inferior rectus paresis is observation for six months. If there is no improvement during this time, muscle surgery may be recommended. [10] [9]
Other Issues
The inferior rectus has a muscle capsule that binds to the muscle capsule of the inferior oblique. This fibrous connection is known as Lockwood's ligament and connects the lower eyelid retractors.