Anatomy, Thorax, Intercostal Nerves
- Article Author:
- Niklas Glenesk
- Article Author:
- Sajedur Rahman
- Article Editor:
- Peter Lopez
- Updated:
- 7/27/2020 9:17:56 PM
- For CME on this topic:
- Anatomy, Thorax, Intercostal Nerves CME
- PubMed Link:
- Anatomy, Thorax, Intercostal Nerves
Introduction
The intercostal nerves emerge from the somatic nervous system and aid in the contraction of muscles as well as provide sensory information from the skin and parietal pleura. The intercostal nerves arise from the anterior rami of the thoracic spinal nerves from T1 to T11. The anterior division of the twelfth thoracic nerve is not technically grouped with the other intercostal nerves as it enters the abdominal wall; this nerve is instead referred to as the subcostal nerve. Some techniques utilize the blockage of these nerves for analgesia and also pathology of these nerves giving rise to neuralgia. It is crucial for providers to be comfortable with the anatomy and physiology of the intercostal nerves to accurately diagnose and treat intercostal nerve pain and pathology.
Structure and Function
Each of the intercostal nerves enters the correlated intercostal space in between the posterior intercostal membrane and the parietal pleura. The intercostal nerve at this point is directly outside of the parietal pleura and then dives forward to the subcostal groove of its associated rib, which lies directly inferior to the rib. The boundary of the nerve as it runs this course through the subcostal groove is the innermost intercostal muscle and the internal intercostal muscle. The first six intercostal nerves give branches, which will be explained in detail later, and then end within the intercostal space of their corresponding rib. The seventh through eleventh intercostal nerves exit the intercostal spaces and travel into the abdominal wall. These last five intercostal nerves are termed thoraco-abdominal nerves due to this pathway.[1][2]
Blood Supply and Lymphatics
The intercostal vessels travel along with the intercostal nerves in the intercostal space of each rib. There are the anterior and posterior intercostal arteries. The anterior intercostal arteries are branches of the internal thoracic artery and supply the upper six intercostal spaces. After this point, the internal thoracic artery divides into the superior epigastric artery and musculophrenic artery. The musculophrenic artery is then the tributary for the remaining anterior intercostal branches which then anastomose with the posterior intercostal arteries forming the thoracic aorta. The right posterior intercostal arteries are longer in length than the left due to the aorta's position to the left of the vertebral column.[3] Each posterior intercostal artery travels along the bottom of the rib with a corresponding posterior intercostal vein and intercostal nerve. The intercostal nerve lies inferior to the intercostal artery while the intercostal vein lies superior to it.[4]
Nerves
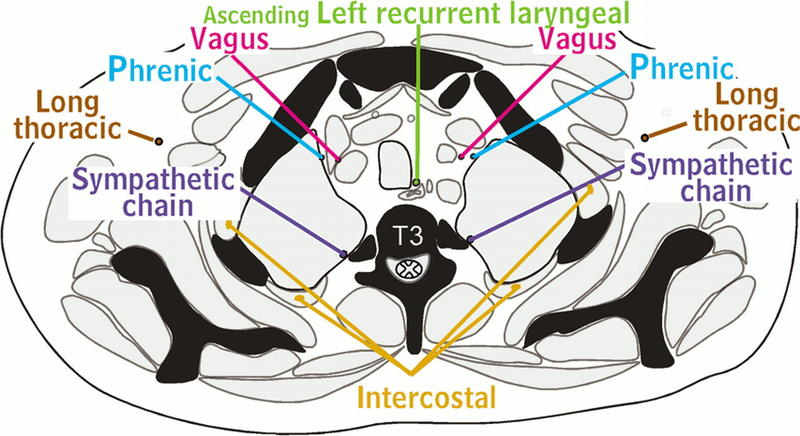
The intercostal nerves commonly group into two categories: typical intercostal nerves and atypical intercostal nerves. The typical intercostal nerves include T3 through T6, and the atypical intercostal nerves include T1 through T2 and T8 through T11. The main reason for the two separate groupings is that the typical intercostal nerves stay confined to their own intercostal spaces while the atypical spinal nerves go past the thoracic wall and partially or wholly supply other regions.[5]
The typical intercostal nerve runs laterally behind the sympathetic trunk and enters the intercostal space between the parietal pleura and the intercostal membrane as described above. While in the costal groove, it runs along the intercostal vessels and travels in front of the internal thoracic artery. The major branches of the typical intercostal nerves include the rami communicates, the muscular branches, the collateral branch, the lateral cutaneous branch, and the anterior cutaneous branch. The rami communicate branches innervate the corresponding thoracic ganglion by gray and white rami. The muscular branches supply the intercostal muscles as well as the serratus posterior and superior. The collateral branch innervates the intercostal muscles, parietal pleura, and the periosteum of the rib. The lateral cutaneous branch goes through the muscles of the lateral thoracic wall and then divides to anterior and posterior branches to give cutaneous information from the skin of the lateral thoracic wall. The anterior cutaneous branch is the terminal branch of the typical intercostal nerves and divides into medial and lateral branches to supply the skin of the anterior thoracic wall.[6]
The atypical intercostal nerves, T1 through T2 and T7 through T11, run a more complicated course and have their own routes to innervation in the human body. The first intercostal nerve does give some contribution to the lower trunk of the brachial plexus along with the ventral ramus of C8. The rest of the first intercostal nerve lacks both lateral and anterior cutaneous branches seen in typical intercostal nerves. The second intercostal nerve has a branch named the intercostobrachial nerve, and this branch gives cutaneous information from the floor of the axilla and superior region of the upper extremity. In cases of coronary artery disease, the cardiac pain patients describe on the medial side of the arm is due to this nerve. The seventh to eleventh intercostal nerves travel in the intercostal spaces but then travel into the abdominal wall where they supply muscles such as the external oblique, internal oblique, transverse abdominis, and rectus abdominis. They also innervate the skin and parietal peritoneum.[7]
Surgical Considerations
The intercostal nerves are at constant jeopardy of being damaged during thoracotomy procedures. The intercostal nerves are also in danger of damage or transection during placement of a chest tube. There have been case reports that describe techniques of chest tube placement that include careful dissection of the intercostal spaces and identification of the intercostal nerve as opposed to a stab insertion of a chest tube. There have also been reports that anesthetic blocks of the intercostal nerves before closure of a thoracotomy have resulted in hypotension both with and without a spinal block.[8][9]
Clinical Significance
Pain arising from the intercostal nerves has been termed intercostal neuralgia. Intercostal neuralgia is a common pathology that can occur due to nerve entrapment, traumatic causes, persistent nerve irritation, and herpes zoster. Patients describe the pain itself as a shooting, burning, or sharp pain. The location of the pain usually begins at the posterior axillary line and radiates anteriorly into the distribution of the intercostal nerve. The pain is reproducible during deep inspiration or other chest wall movements, which creates a complication for those who do not take adequate breaths. Upon diagnosing intercostal neuralgia, treatment can vary from pharmacological therapy with tricyclic antidepressants or anticonvulsants, non-somatic treatment, and also interventional pain treatment. It is important to note that intercostal nerve blocks are a viable option to provide analgesia, however, their proximity to the pleural space made careful attention to technique and anatomy mandatory.[10]
(Click Image to Enlarge)
(Click Image to Enlarge)