Isthmic Spondylolisthesis
- Article Author:
- Matthew Burton
- Article Author:
- Thomas Dowling
- Article Editor:
- Fassil Mesfin
- Updated:
- 8/11/2020 11:34:58 AM
- For CME on this topic:
- Isthmic Spondylolisthesis CME
- PubMed Link:
- Isthmic Spondylolisthesis
Introduction
The lumbar spine in the sagittal plane should maintain an alignment in which each vertebral body is aligned with the vertebral body above and below. In other words, the anterior inferior endplate of the vertebral body above should be aligned with the anterior superior endplate of the vertebral body below. Spondylolisthesis occurs when there is an anterior translation or “slippage” of one vertebral body relative to its caudal vertebral body. In most cases, symptoms associated with spondylolisthesis are chronic. The primary symptom of chronic spondylolisthesis is back pain, with or without leg pain. When spondylolisthesis occurs acutely in the setting of traumatic or metastatic tumors, patients can present with neurological examination deficits including a loss of bowel and bladder function. The classification system utilized to categorize the degree of subluxation of the vertebral bodies is the Meyerding Classification, which quantifies the percentage of subluxation of the vertebral body above on the vertebral body below. Classification of Spondylolisthesis is based on the degree of slippage in the lumbar spine. Grade 1 is less than 25%, Grade 2 is 25% to 50%, Grade 3 is 50% to 75%, Grade 4 is 75% to 100%, and Spondyloptosis is > 100% [1].
There are many causes of spondylolisthesis including congenital, degenerative, traumatic, pathologic, iatrogenic, and isthmic. Isthmic spondylolisthesis, which will be the topic of this discussion, refers to a defect in the pars interarticularis that then results in anterior subluxation over time, most commonly at L5-S1 followed by L4-5. The resulting anterior subluxation can produce back pain, central canal stenosis, and lateral recess or foraminal stenosis.
Etiology
The most common etiology for isthmic spondylolisthesis is instability of unilateral or bilateral pars interarticularis. The pars interarticularis, or pars, is the bony structure which connects the lamina, pedicle, and transverse processes of the vertebral bodies. Importantly, the facet joints of the superior and inferior vertebrae also are connected by the pars. Thus, a defect in this structure would effectively “disconnect” the vertebral body above from the vertebral body below. This disconnection allows the anterior subluxation seen in spondylolisthesis. Many biomechanical studies indicate that the pars is subjected to the greatest force of any structure in the lumbar spine; therefore, it is susceptible to stress fractures which may heal and fracture repeatedly over time. These injuries can induce non-healing fractures or an elongated pars without a defect which likely indicates repeated fracture healing. Pars fractures are believed to be the result of repetitive motion. Thus, risks associated with pars defects include activities associated with repetitive flexion/extension, axial loading, and rotational loading (i.e., golfers, weight lifers, baseball and football players, gymnasts).
Epidemiology
The incidence of isthmic spondylolisthesis is generally reported as between 4% to 8% of the general population. It is three times as common in males as it is in females. An interesting cross-sectional study utilizing the Framingham Heart Study participant of 3529 patients showed that 20% of patients with CT finding of bilateral pars defect showed no evidence of spondylolistheisis[2]. In addition, this cross-sectional study showed that the incidence of spondylolisthesis increases significantly from the fifth decade of life to the eighth decade of life .
Pathophysiology
Spondylolisthesis can result in accelerated degeneration of the intervertebral disc which can lead to diminished height of the neural foramen and increased stresses on the facet joints posteriorly. This increased stress can lead to hypertrophy of the facet and ligamentum flavum. These changes can result in back pain, neurogenic claudication and radiculopathy. The radicular symptoms of isthmic spondylolisthesis are typically caused by the foraminal stenosis. Since the level most commonly affected is L5-S1, the L5 exiting nerve root in the L5-S1 foramen can be compressed. Other causes of symptoms can include lateral recess stenosis which, for example, can be caused by facet arthrosis or hypertrophied ligamentum flavum. Even more rare would be symptoms caused by central stenosis, given that most of these spondylolistheses rarely progress beyond grade II, and as the vertebral body translates anteriorly, the posterior elements tend to remain with the caudal vertebra maintaining their normal anatomic alignment.[3]
History and Physical
Many cases of isthmic spondylolisthesis are asymptomatic. However, the most common symptom of presentation is low back pain, which may be mechanical in nature. Patients also can present with neurogenic claudication symptomatology such as back and leg pain and discomfort associated with walking. These symptoms need to be differentiated from vascular claudication, which is exacerbated by ambulation and gets better with rest. Other patients can present with symptoms of specific dermatome of lumbar radiculopathy depending on the compressed nerve root and the amount of subluxation or stenosis. Physical examination can show different degrees of findings ranging from normal to paraplegia. However, the most common findings are depressed deep tendon reflexes, positive straight leg signs, and diminished sensations. Some patients can have specific pain-related weakness of lower extremities. Usually, patients with chronic isthmic spondylolisthesis do not present with significant motor weakness; however, acute isthmic spondylolisthesis can present with paralysis and loss of bowel and bladder function. Since L5-S1 is the most commonly afflicted level, an L5-S1 isthmic spondylolisthesis will typically cause radicular symptoms that correlate with the L5 exiting nerve at that level such as weakness in ankle dorsiflexion and hallux extension.
Evaluation
Radiological evaluation is not indicated upon initial presentation of low back pain because of its self-limiting nature. However, serious conditions such as tumor or infection should be ruled out with a high-quality history and physical examination. Should the back pain not respond to conservative management then plain x-rays, including oblique views and lateral flexion-extension views, may be used to assess the bony quality and alignment of the lumbar spine as well as any dynamic instability. Should the initial presentation also consist of radicular symptoms or symptoms of neurogenic claudication, then the neural elements must be evaluated with an MRI or CT myelogram of the lumbar spine.
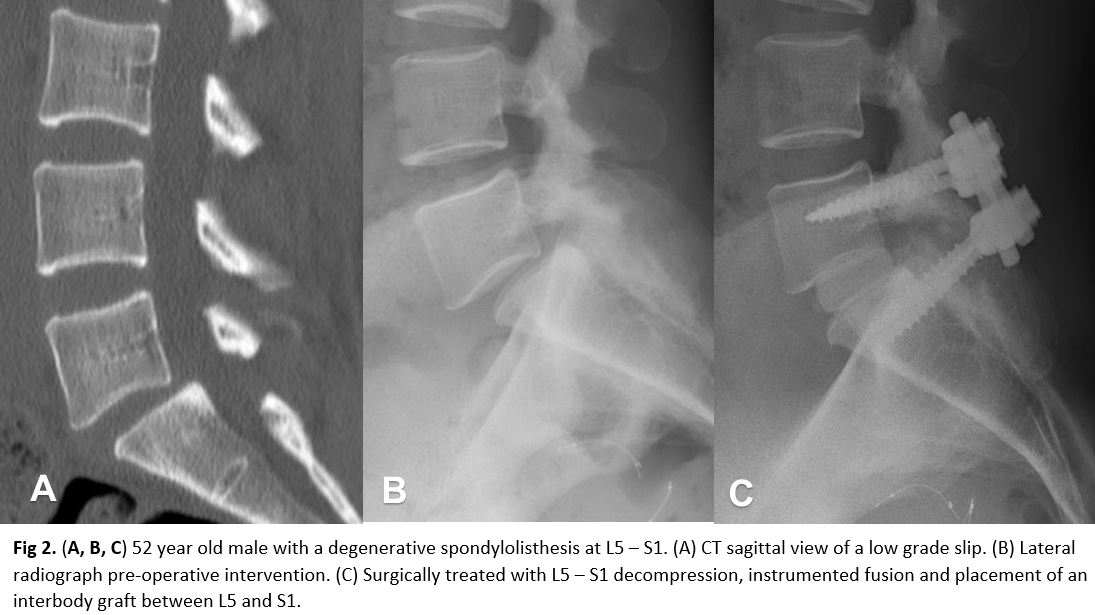
The degree of slippage is best characterized on the lateral x-ray. An oblique view x-ray of the lumbar spine is a good tool to assess the pars defect. CT Scan of the lumbar spine is the definitive study to assess the pars defect. MRI is the study of choice for evaluation of soft tissue structures including intervertebral discs, ligamentum flavum, the thecal sac, nerve roots, and the conus medullaris in the lumbar spine. MRI is needed for patients who fail conservative treatments and are planning a surgical intervention.
Treatment / Management
Isthmic spondylolisthesis with low back pain should initially be managed conservatively. Activity modification, NSAIDs, muscle relaxers, physical therapy, and epidural steroid injections are some of the conservative options. Should the back pain persist despite conservative management, or if the severity is such that quality of life is significantly affected, then referral to a specialist for evaluation is indicated. When the presentation consists of symptoms of neurogenic claudication or radiculopathy, then imaging of the neural elements of the lumbar spine is indicated along with referral to a specialist. Surgical treatment options consist of decompression of the neural elements alone versus decompression with internal fixation for bony fusion to prevent further subluxation [4]. In addition, for patients who present with acute symptoms due to trauma or malignancies, emergent surgical referrals are indicated [5].[6][7][8]
Differential Diagnosis
Differential Diagnosis:
- Degenerative spondylolisthesis
- Traumatic spondylolisthesis
- Dysplasatic spondylolisthesis
- Pathologic spondylolisthesis (i.e., neoplasm, infection, iatrogenic)
Enhancing Healthcare Team Outcomes
Low back pain is commonly encountered by the nurse practitioner, primary caregiver, emergency department physician, and internist. Isthmic spondylolisthesis is also a common cause of back pain and the diagnosis is confirmed by the radiologist. The initial management of the condition is with conservative measures but when patients fail to respond, a referral to an orthopedic surgeon is recommended. Surgical treatment options consist of decompression of the neural elements alone versus decompression with internal fixation for bony fusion to prevent further subluxation [4]. In addition, for patients who present with acute symptoms due to trauma or malignancies, emergent surgical referrals are indicated [5].
Unfortunately, many patients continue to have a recurrence of pain because no treatment works consistently or reliably. Surgery only benefits a few patients and is associated with serious complications. Thus the primary care provider should emphasize lifestyle changes, regular exercise, discontinuation of tobacco and a healthy body weight.[9][10]