
Anterior Cruciate Ligament Knee Injuries
- Article Author:
- Jennifer Evans
- Article Editor:
- Jeffery Nielson
- Updated:
- 8/10/2020 9:06:45 PM
- For CME on this topic:
- Anterior Cruciate Ligament Knee Injuries CME
- PubMed Link:
- Anterior Cruciate Ligament Knee Injuries
Introduction
The anterior cruciate ligament (ACL) is one of 2 cruciate ligaments which aids in stabilization of the knee joint. It is a strong band made of connective tissue and collagenous fibers that originate from the anteromedial aspect of the intercondylar region of the tibial plateau and extends posteromedially to attach to the lateral femoral condyle. The anteromedial bundle and posterolateral bundle form the 2 components of the ACL. [1][2][3] The ACL and the posterior cruciate ligament (PCL) together form a cross (or an “x”) within the knee and prevents excessive forward or backward motion of the tibia in relation to the femur during flexion and extension. The ACL additionally provides rotational stability to the knee with varus or valgus stress. ACL sprains and tears are common knee injuries with a reported incidence of 100,000 to 200,000 in the United States every year.
Etiology
The ACL is the most commonly injured ligament in the knee. The annual reported incidence in the United States alone is approximately 1 in 3500 people. However, data may not be accurate as there is no standard surveillance. Most ACL tears occur in athletes by noncontact mechanisms versus contact mechanisms, such as rotational forces versus a direct hit to the knee. The most at risk athletes for noncontact injury include skiers, soccer players, and basketball players, while the most at risk athletes for contact injury are football players.
Epidemiology
There is no age or gender bias; however, it has been suggested that women are at increased risk of ACL injury secondary to a multitude of factors. Some studies suggest that females may have weaker hamstrings and preferential utilize the quadriceps muscle group while decelerating. When engaging the quadriceps musculature while slowing down, this places abnormally increased stress on the ACL, as the quadriceps muscles are less effective at preventing anterior tibial translation versus the hamstring muscles. A second factor that may increase the risk of ACL injury is the increased valgus angulation of the knee. [4] [5]One study utilizing video analysis demonstrated that female athletes are more likely to place their knees in increased valgus angulations when changing directions suddenly, which increased the stress on the ACL ligament. Lastly, it has been suggested that estrogenic effects on the strength and flexibility of tissues such as ligaments may play a role and predispose females to injury; however, this remains controversial and has yet to be proven.
History and Physical
One of the most common knee injuries is an ACL sprain or tear. Typically, injury occurs during activity/sports play that includes sudden changes in the direction of movement, rapid stopping, jumping and landing abnormally, a direct blow to the lateral aspect of the knee, or slowing down while running.
Most patients complain of hearing and feeling a sudden “pop” and feel that their knee “gives out” from under them at the time of injury. Other symptoms include tenderness along the joint line, pain, and swelling, decreased or loss of range of motion, and difficulty ambulating.
The physical exam should include timing of the injury, mechanism of injury, ambulatory status, joint stability, mobility, strength, palpation, and evaluation of possible associated injuries.
Multiple maneuvers are employed to test the ACL and include the anterior drawer, the pivot shift, and the Lachman tests.[6][7] These tests should be performed whenever there is suspicion for injury to the anterior cruciate ligament.
-
The anterior drawer test is performed with the patient lying supine with their affected knee flexed to 90 degrees and the foot in a planted position (Sometimes it is easiest for the clinician to stabilize the patient’s foot by sitting on it). The clinician will grip the proximal tibia with both hands and pull with an anterior motion. If there is excessive anterior motion and instability, then the test is positive. It may also be useful to compare to the unaffected knee as patients may have increased laxity of the ACL that is not pathologic. This test has a sensitivity of 92% and specificity of 91% in chronic injuries, but not acute injuries.
-
The pivot shift test is performed with the patient in the supine position. The clinician should hold the patient’s lower leg and begin with the knee in extension and flexion of the hip to 20 to 30 degrees. Next, the clinician will bring the tibia into the internal rotation with one hand and begin placing valgus stress on the knee using the other hand. While holding this position, the knee should now be flexed. This causes stress, instability, and ultimately subluxation of the ACL of the affected knee. With flexion of the knee, if the tibia subluxes posteriorly and one may feel a “clunk”; this would indicate a positive test. This test can be difficult to perform in patients who are guarding, and some may not allow the clinician to perform the test. This is a highly specific test (98%) when positive, but is insensitive (24%) due to the difficulty in evaluation secondary to patient pain and cooperation.
-
The Lachman test is performed with the patient in the supine position with the knee flexed to about 30 degrees. The clinician should stabilize the distal femur with one hand and with the other hand pull the tibia toward themselves. If there is increased anterior translation, then this is a positive test. Again, comparing to the unaffected side may be helpful. This test has a sensitivity of 95% and specificity of 94% for ACL rupture.
It is important to evaluate for associated injuries such as medial or lateral collateral ligamentous injury, injury to the posterior collateral ligament, or meniscal injuries.
Evaluation
Although ACL injury can be diagnosed clinically, imaging with magnetic resonance (MRI) is often utilized to confirm the diagnosis. MRI is the primary modality to diagnose ACL pathology with a sensitivity of 86% and specificity of 95%. Diagnosis may also be made with knee arthroscopy to differentiate complete from partial tears, as well as chronic tears. Arthrography is considered the gold standard as it is 92% to 100% sensitive and 95% to 100% specific; however, it is rarely used as the initial step in diagnosis as it is invasive and requires anesthesia.
On MR, ACL tears have primary and secondary signs. Primary signs will indicate changes associated directly with the ligamentous injury while secondary signs are changes that are closely related to the ACL injury. Primary signs include edema, an increased signal of the anterior cruciate ligament on T2 weighted or proton density images, discontinuity of the fibers, and a change in the expected course of the ACL (alteration of Blumensaat’s line). Tears usually occur within the midportion of the ligament, and signal changes are most often seen here and appear hyperintense. Secondary signs include bone marrow edema (secondary to bone contusion), Second fracture (as discussed below), associated medial collateral ligament injury, or anterior tibial translation of greater than 7 mm of the tibia relative to the femur (best seen on lateral view).
Radiographs are generally non-contributory for ACL injuries but are helpful to rule out fractures or other associated osseous injuries. In younger patients, avulsion of the tibial attachment may be seen. Other non-specific features that can be seen on radiographs include:
-
Second fracture: An avulsion fracture at the site of the lateral capsular ligaments/IT band insertion on the tibia
-
Arcuate fracture. An avulsion fracture at the proximal fibula at the site of the lateral collateral ligament and/or biceps femoris tendon
-
Joint effusion
-
Deep lateral sulcus sign: A notch on the lateral femoral condyle with a depth of 1.5 mm or more, best seen on the lateral view
Computed tomography (CT) is not generally utilized in evaluating the ACL and is only accurate in detecting an intact ACL.
Treatment / Management
Acute treatment consists of the “RICE” therapy, which includes rest, ice, compression of the affected knee, and elevation of the affected lower extremity. Patients should be non-weight bearing and may utilize crutches, or a wheelchair if necessary. Pain relief can be achieved with over the counter medications such as NSAIDs but is typically at the discretion of the treating physician.
ACL injuries, depending upon their severity, can be managed nonoperatively or operatively. The patient with an anterior cruciate ligament injury should be referred to the orthopedic physician to discuss treatment options and a physical therapist (PT) for rehabilitation.
Nonoperative treatment is typically reserved for those with low functional demands, type and severity of ACL tear, and time of injury and subsequent assessment. Continued monitoring and treatment by an orthopedist and physical therapist is necessary and will only improve their functional status and stability post-injury. Of note, about half of the patients who initially choose the non-operative pathway will later choose to undergo surgical repair.
The decision to undergo operative treatment is based upon a multitude of factors such as patient’s baseline level of physical activity, functional demands, age, occupation, and other associated injuries, if present. [8][9][10]Athletes and individuals who are younger and more active tend to opt for surgical repair and reconstruction. Other candidates for surgical repair/reconstruction are those with significant instability of the knee and/or multiple knee structures injured. Operative treatment is typical with a tissue graft. In a recent systematic review, 81% of those involved treated with ACL reconstruction returned to some athletic activity, 65% returned to the preinjury level of competition, and 55% of high-level athletes returned to normal play and competition. Although, it has been reported that of those who undergo surgical repair, overall 90% return to near normal functioning. The factors that may contribute to a lower percentage of return to play may be secondary to external factors such as fear of reinjury.
Differential Diagnosis
- ACL tear
- Epiphyseal fracture of femur or tibia
- Medial collateral knee ligament injury
- Meniscal tear
- Osteochondral fracture
- Patellar dislocation
- Posterior cruciate ligament injury
- Tibial spine fracture
Pearls and Other Issues
Return to activity is variable and patient dependent. Average return to full activity and/or sports participation is estimated to be between 6 to 12 months after surgical reconstruction depending upon their progress with PT and the type of sport/activity to which they are returning. However, some studies have shown up to 18 months or more for the graft to become fully functional and incorporated. Early/premature return to activity can lead to reinjury and graft failure.
Enhancing Healthcare Team Outcomes
The diagnosis and management of ACL are best by an interprofessional team that includes an emergency department physician, orthopedic surgeon, sports physician, nurse practitioner, and a physical therapist. The initial treatment of ACL is RICE therapy. ACL injuries, depending upon their severity, can be managed nonoperatively or operatively. The patient with an anterior cruciate ligament injury should be referred to the orthopedic physician to discuss treatment options and a physical therapist (PT) for rehabilitation. Care coordination between PT and the treating clinician is often the task of a specialty-trained orthopedic nurse, who is also able to counsel the patient on their condition and treatment. The outcomes for patients with ACL injury are good but the recovery may take at least 3 to 9 months of intense physical therapy.[2][11]
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
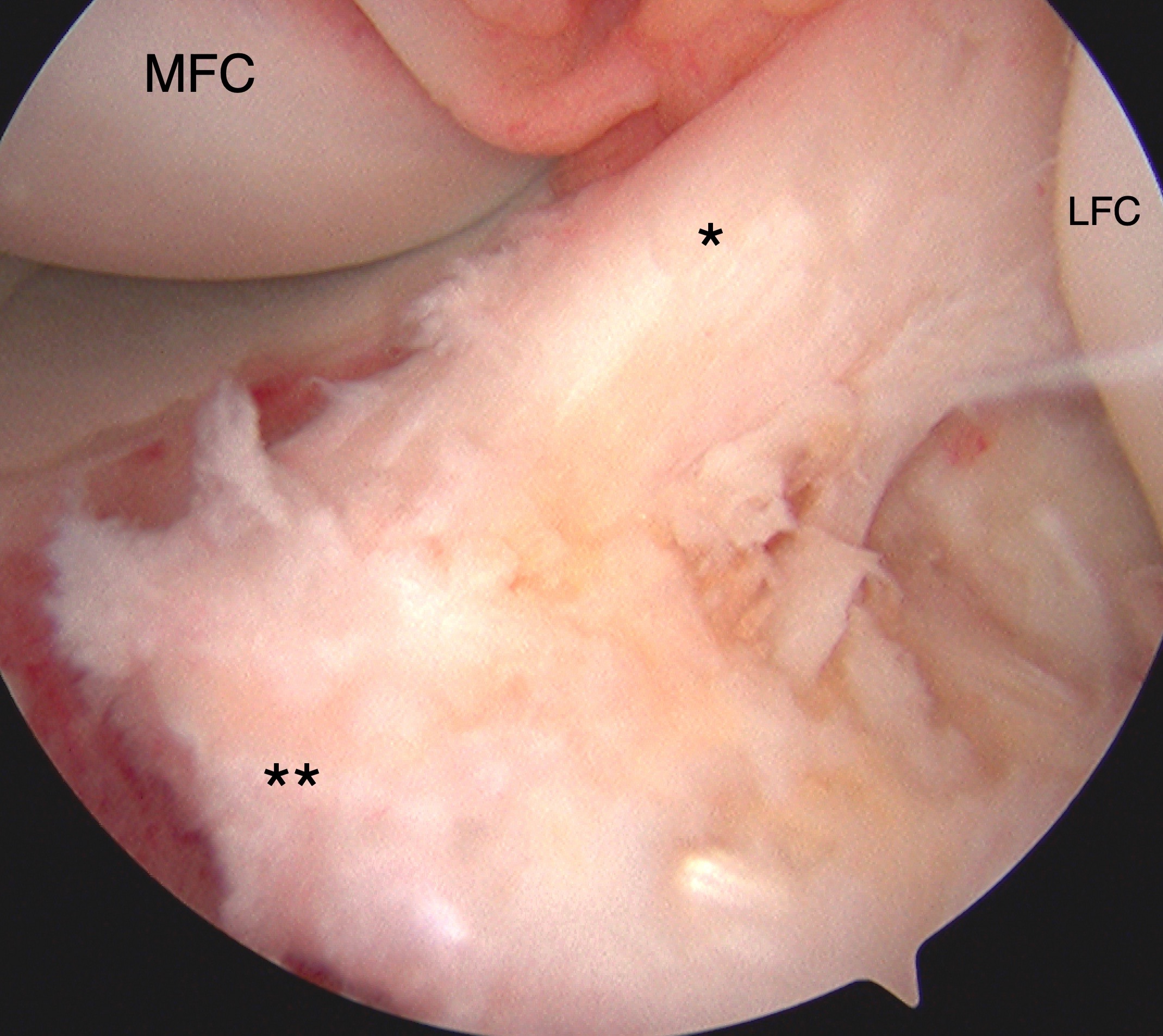
Tibial eminence avulsion injury confirmed with direct visualization during knee arthroscopy with arthroscopic-assisted internal fixation suture reduction technique. The anterior cruciate ligament (*, ACL) and insertional footprint on the tibia (**) are denoted. The medial (MFC) and lateral (LFC) femoral condyles are also labeled for reference.
Contributed by Matthew A Varacallo MD

