Anatomy, Bony Pelvis and Lower Limb, Arteries
- Article Author:
- Daniel Arias
- Article Editor:
- Raghavendra Marappa-Ganeshan
- Updated:
- 8/16/2020 2:42:34 AM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Arteries CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Arteries
Introduction
The bony pelvis and lower limbs receive vascular supply from the distal continuations of right and left common iliac arteries. The primary blood supply to the bony pelvis is from the divisions of iliac arteries while the lower limbs receive supply via obturator artery and divisions of the common femoral artery.
Blood supply to the lower limbs and pelvis have several significant medical, musculoskeletal, and surgical considerations that make a thorough understanding of the anatomy vital to patient care. The goal of this activity is to provide a review of the arterial supply of the bony pelvis and lower limb, to improve practitioner knowledge and medical care.
Structure and Function
Bony Pelvis
The bony pelvis is a structure formed from the ilium, ischium, and pubis, with the sacrum completing the pelvic ring. Arterial supply derives from the distal bifurcation of the aorta which forms right and left common iliac arteries. These further subdivide to create the internal and external iliac arteries.
The external iliac artery courses along the pelvic brim, producing circumflex iliac artery and the pubic branch. The circumflex iliac artery supplies the iliac crest, while the pubic branch supplies the superior pubic ramus and continues as the femoral artery after crossing the inguinal ligament.
The internal iliac artery courses along the posteromedial ischium, producing the anterior and posterior divisions.[1]
The posterior division forms the iliolumbar artery, superior gluteal artery, and lateral sacral arteries. Iliolumbar artery courses retrograde along the medial aspect of the ilium and lateral aspect of the lumbar vertebrae to supply the superior aspect of the ilium and lower lumbar vertebrae. The superior gluteal artery exits the pelvis via superior sciatic foramen superior to the piriformis muscle, producing a nutrient branch to the ilium. The lateral sacral artery courses along the lateral sacrum, supplying the sacrum and forming an anastomotic arterial plexus with the median sacral artery (a distal continuation of the aorta).
The anterior division produces the obturator artery and the inferior gluteal artery. The obturator artery traverses the pelvis, exiting through the obturator foramen. Before exiting the pelvis, there may be an anastomotic connection between obturator artery to external iliac circulation, known as accessory obturator artery, or corona mortis; the clinical significance of this variant is a topic of discussion below.[2] Inferior gluteal artery exits the pelvis via the greater sciatic foramen between the piriformis and ischiococcygeus muscles.
Femur
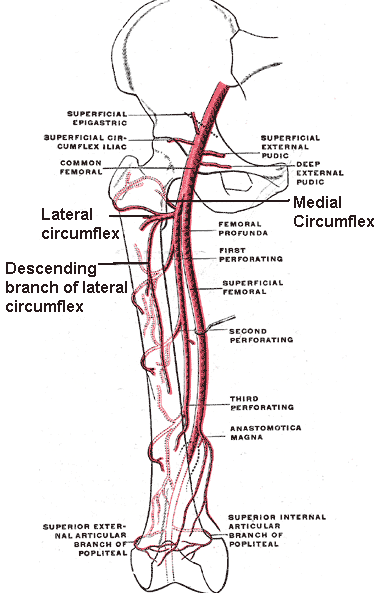
A description of the arterial supply to the femur best divides into thirds. The proximal third of femur includes the femoral head, neck, trochanters, and metaphysis. The medial femoral circumflex artery provides the primary supply to this region, but also involves the lateral femoral circumflex, anastomosis of the inferior gluteal artery, and flow through the foveal artery via the ligamentum teres.[3] There are several important anastomoses near the head and neck of femur, known as the cruciate anastomosis; this is a confluence of arteries at the level of the lesser trochanter, comprised of the following vessels: medial femoral circumflex artery, lateral femoral circumflex artery, inferior gluteal artery, and first perforator of profunda femoris artery.[4] The profunda femoris artery supplies the middle third.[5] The distal third includes the medial and lateral femoral condyles. The medial femoral condyle gets its supply from descending genicular artery, a branch of the femoral artery proximal to adductor hiatus. The superior lateral genicular artery supplies the lateral femoral condyle. These arteries create an anastomosis around the distal femur.[6]
Gluteal Region
Superior and inferior gluteal arteries provide blood to the gluteal region.
The superior gluteal artery is a division of the posterior division of the internal iliac artery. It exits the pelvis via greater sciatic foramen, superior to the piriformis muscle, coursing between gluteus minimus muscle and gluteus medius muscle. Superior gluteal artery supplies gluteus minimus, gluteus medius, gluteus maximus, and tensor fascia lata muscles.
The inferior gluteal artery is a division of the anterior division of the internal iliac artery. It exits the pelvis via greater sciatic foramen inferior to the piriformis muscle and superior to ischiococcygeus muscle. It takes a course deep to gluteus maximus and superficial to the external rotators of the hip. Inferior gluteal artery supplies gluteus maximus, piriformis, superior gemellus, obturator internus, inferior gemellus, and quadratus femoris muscles, as well as contributions to the greater trochanter of the femur and sciatic nerve.[7]
The Medial Compartment of Thigh
Obturator artery exits the pelvis via obturator canal, a passage in obturator foramen formed by obturator membrane. It supplies the majority of the contents within the medial compartment of thigh including obturator externus, pectineus, adductor magnus, adductor brevis, adductor longus, and gracilis muscles.[8]
Anterior Compartment of Thigh
External iliac artery exits the pelvis deep to the inguinal ligament, becoming the common femoral artery. The common femoral artery lies lateral to femoral vein and medial to femoral nerve and inhabits the femoral sheath along with femoral vein. Upon passing inguinal ligament, common femoral artery produces superficial circumflex iliac artery and superficial epigastric artery. Common femoral artery then produces profunda femoris artery, which produces medial and lateral circumflex femoral artery. The distal iliopsoas muscle is supplied by the medial femoral circumflex artery, while the iliolumbar artery supplies the proximal aspect. The lateral circumflex artery supplies the vastus lateralis and rectus femoris. The remainder of the musculature in the anterior compartment of thigh including vastus intermedius, vastus medialis, and sartorius receive their supply from the femoral artery.[9]
Posterior Compartment of Thigh
Profunda femoris artery produces perforating arteries, so named because they perforate the adductor magnus to supply posterior compartment of thigh. Thus, supply to biceps femoris, semimembranosus, and semitendinosus muscles arises primarily from these perforating branches. The semimembranosus muscle and semitendinosus muscle additionally receive supply from the inferior gluteal artery.[10]
Popliteal Region and Knee
Distally, femoral artery passes through adductor hiatus in adductor magnus to become popliteal artery. Immediately prior to passing through the adductor canal, femoral artery also produces descending genicular artery, which bifurcates to form the articular and saphenous branches of the knee. At the level of the femoral epicondyles, the popliteal artery produces superior lateral and superior medial genicular arteries. The superior lateral genicular artery forms an anastomosis with the descending branch of the lateral circumflex femoral artery. On reaching the level of the tibial plateau, the popliteal artery produces the inferior lateral and inferior medial geniculate arteries. A patellar anastomosis forms from the superior lateral, superior medial, inferior lateral, and inferior medial geniculate arteries, with additional contribution from the articular branch of descending genicular artery. Distal to lateral and medial inferior genicular arteries, popliteal artery bifurcates to form anterior and posterior tibial arteries. From the anterior tibial artery arise anterior and posterior tibial recurrent arteries. The posterior tibial recurrent artery branches off the anterior tibial artery prior to it passing through the interosseous membrane, forming an anastomosis with inferior genicular arteries and supplying the tibiofibular joint. The anterior tibial recurrent artery branches off the anterior tibial artery after passing through the interosseous membrane and anastomoses to contribute to the patellar plexus.[11]
Tibia
Categorizing the arterial supply to the tibia is best by dividing the tibia into the proximal fifth, proximal diaphysis, distal diaphysis, and distal fifth. The proximal fifth of the tibia receives is vascular supply by the anterior and posterior tibial arteries, as well as the medial inferior geniculate artery. The proximal diaphysis of the tibia is supplied by anterior and posterior tibial arteries, while distal diaphysis is supplied almost exclusively by semicircular periosteal branches of the anterior tibial artery. The distal fifith of tibia differs between populations. In approximately two-thirds of people, fibular artery and anterior tibial artery combine to supply this region, while in the other one-third of people, the anterior tibial artery supplies it alone.[12]
Fibula
The primary arterial supply to fibula is from the fibular artery, through proximal contributions are made from the anterior tibial artery.[13]
Lateral Compartment of the Leg
The peroneus (fibularis) longus and peroneus (fibularis) brevis comprise the muscular content of the lateral compartment of the leg, both receiving supply via the fibular artery. The fibular artery is a tributary of the posterior tibial artery, arising just distal to the interosseous membrane. It courses deep to the fibula and produces perforating branches which facilitate muscular arterial supply.[14]
Anterior Compartment of the Leg
Anterior tibial artery supplies the majority of the anterior compartment of the leg. After passing through the interosseous membrane, anterior tibial artery courses along the interosseous membrane lateral to tibialis anterior, medial to extensor digitorum longus, and medial to extensor hallucis longus. It supplies the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius muscles.[15]
Superficial Posterior Compartment of the Leg
The plantaris, gastrocnemius, and soleus comprise the muscular content of the superficial posterior compartment of the leg. The plantaris and gastrocnemius muscles are supplied by sural arteries which are a group of short arteries arising from popliteal artery. The soleus receives supply from the posterior tibial artery, popliteal artery, and peroneal artery. The posterior tibial artery takes its course deep to soleus and superficial to the deep posterior compartment of the leg.[16]
Deep Posterior Compartment of the Leg
Popliteus, flexor hallucis longus, tibialis posterior, flexor digitorum longus form the deep posterior compartment of the leg. Popliteus is deep to the popliteal artery from which it receives its vascular supply. The posterior tibial artery lies lateral to flexor digitorum longus and medial to tibialis posterior and supplies both of these muscles. Flexor hallucis longus gets supplied by the peroneal artery, which lies deep to it.[16]
Tarsal Bones, Metatarsals, and Phalanges
Combination supply from dorsalis pedis, fibular, posterior tibial, medial plantar, and lateral plantar arteries provide blood to the tarsal, metatarsal, and phalangeal bones. The periosteal and endosteal vascular supplies often differ and make up separate anastomotic plexuses. Talar vascular supply is via the artery of the tarsal sinus (a branch of the fibular artery), branches of dorsalis pedis artery, as well as the artery of the tarsal canal and the deltoid branch from the posterior tibial artery.[17] The calcaneus is supplied by the calcaneal anastomosis which forms from branches derived from the fibular and posterior tibial artery.[18] The navicular bone recieves blood from branches of the dorsalis pedis and posterior tibial artery.[19] The lateral plantar artery supplies the cuboid.[20]. The cuneiform bones obtain plantar blood supply from the medial plantar artery and extraosseous blood supply from dorsalis pedis.[21] The dorsal and plantar metatarsal arteries supply the metatarsal bones; dorsal metatarsal arteries are branches of dorsalis pedis, while plantar metatarsal arteries are branches of the posterior tibialis artery.[22] The fifth metatarsal gets supplied from the fibular artery, lateral plantar artery, and dorsalis pedis artery. There is a notable watershed area in the proximal base of the fifth metatarsal that carries a propensity for fracture nonunion secondary to avascular necrosis. This topic will have further coverage in the clinical significance section.[23] [24] Phalanges of the foot receive vascular supply from the dorsalis pedis artery and plantar metatarsal arteries.[25]
The Dorsal Compartment of Foot
The anterior tibial artery emerges lateral to tibialis anterior tendon and extensor hallucis longus tendon, and medial to extensor digitorum tendon in the foot to become dorsalis pedis artery. The dorsalis pedis artery supplies both extensor digitorum brevis and extensor hallucis brevis. [26]
The Interosseous Compartment of Foot
The dorsalis pedis artery enters the foot on the dorsal surface, producing the arcuate artery at the level of the metatarsal bases. From this arcuate artery arise the dorsal metatarsal arteries, which supply the second, third, and fourth dorsal interossei muscles. The first dorsal interosseous muscle gets its blood supply by the distal continuation of dorsalis pedis artery. The plantar metatarsal arteries contribute to the supply of dorsal interossei and make up the majority of supply to plantar interossei muscles. These plantar metatarsal arteries are branches of the deep plantar arterial arch, which is an anastomotic arch formed by lateral plantar artery and deep plantar artery. The deep plantar artery is a tributary of the dorsalis pedis artery that dives between heads of first dorsal interosseous muscle to join deep plantar arch.[27]
Lateral Compartment of Sole
Posterior tibial artery bifurcates distally to the tibial tunnel to form the lateral and medial plantar arteries. Lateral compartment of sole receives its arterial supply from the lateral plantar artery. This compartment includes abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi.[28]
Central Compartment of Sole
The lateral plantar artery supplies adductor hallucis and quadratus plantae. Both lateral and medial plantar arteries supply lumbrical muscles. The medial plantar artery supplie vascualrity to the flexor digitorum brevis.[29]
The medial compartment of sole
Abductor hallucis and flexor hallucis brevis comprise medial compartment of the foot. These are both supplied by the medial plantar artery.[29]
Embryology
In all mammals, research has found that limb supply develops from branches of the dorsal root of the umbilical artery, which forms a primitive axial artery, known as the ischiadic artery, that is present early in limb development. A second developmental artery arises later in development traversing the pelvis and proximal thigh that will go on to form the external iliac artery, femoral artery, and inferior epigastric artery.[30]
Physiologic Variants
There is a high level of variability in branch points of arteries and dominance of circulation. This caries clinical significance, as discussed below. Some of the most predominant examples of physiologic variance include the inconsistent presence of the corona mortis, the incongruity in the dominance of proximal femoral arterial dominance, trifurcation of the tibial artery to form anterior tibial, posterior tibial, and fibular arteries, as well as the inconsistent presence of a superficial plantar arterial arch of the foot. There is a plethora of anatomic variation of each of the vessels before described that carry varying degrees of clinical importance.[8][31][32][33][34]
Physiologic variation also occurs with varying age. One example exists in the femoral head, where a significant blood supply exists within ligamentum teres before adulthood but degenerates, leaving the main supply to come from the medial femoral circumflex artery.[35]
Surgical Considerations
The iliac arteries and lower extremity circulation are considered to be highly anatomically variable; therefore, to avoid complications, it is important to plan surgically on an individual basis.[36]
Vascularized Bone Grafting
In instances of significant bone loss, bone grafting may be particularly helpful. The fibular bone graft relies on the supply from the peroneal artery, and this conveys better viability than nonvascularized bone grafts and synthetic alternatives. Fibular bone grafts are the most common vascularized bone grafts, though iliac crest, pubis, rib, radius, ulna, scapula, femur, humerus, and metatarsal grafts are also options.[37]
Meniscus Blood Supply
The blood supply to the meniscus has three zones: red, pink, and white. These zones decrease in vascularity from the periphery to the interior; this is important in that many meniscal injuries occur in the interior zone and thus have limited ability to heal.[38]
Soft Tissue Flaps
Many variations of soft tissue flaps derive from the lower extremities. These have relevance in everything from trauma to diabetic ulcer coverage. Choosing the appropriate flap can have a dramatic impact on the outcome of the procedure.[7][39][40]
Clinical Significance
There are various important considerations for clinical practice concerning the arterial supply of the lower extremity. The following conditions are essential for the clinician to understand and retain in his or her differential diagnoses when evaluating the pelvis and lower extremities.
Corona mortis
A meta-analysis of 21 studies demonstrated the presence of the corona mortis in nearly half of all hemipelvis instances.[2] This fact carries critical clinical implications due to the potential for hemorrhage after pelvic injury, as well as importance in surgical planning in the retropubic region.
Legg-Calve-Perthes
Legg-Calve-Perthes disease highlights the tenuous blood supply to the femoral head and neck. It is an idiopathic disorder of the hip that results in avascular necrosis of the femoral head. This condition develops in children, typically between the ages of 5 and 8 years. The etiology remains a source of debate, though researchers have identified genetic links and coagulopathies are suspected by some authors to contribute. Children present with mild hip pain, limp, and a limited range of motion. When this presents under 6 years of age, nonoperative management with physical therapy has equal outcomes compared to surgery. Patients 6 years and older seem to benefit from surgical intervention.[41]
Avascular Necrosis of the femoral head
There is a myriad of other causes of avascular necrosis of femoral head. These include fracture, dislocation, coagulopathy, sickle cell disease, and many other etiologies. The etiology of necrosis is often unknown or a combination of various risk factors, including smoking, hyperlipidemia, glucocorticoid usage, genetic predisposition, and autoimmune disease. Femoral head sparing surgical approaches are generally preferred in younger patients, though arthroplasty is often necessary.[42]
Popliteal artery laceration (knee dislocation)
Knee dislocations are considered to be surgical emergencies because of the risk of neurovascular complications. Popliteal artery injury is reported to occur in 7.8 to 11.1% of patients with knee dislocations. Additionally, patients found to have vascular injury demonstrate an increased risk of other medical and surgical morbidity. There is significant variability in the reported rates of vascular injury in the setting of knee dislocations, but it remains important to assess patients for these complications, especially in the context of high energy trauma.[43]
Peripheral arterial disease (PAD)
Peripheral arterial disease is a significant cause of morbidity and a predictor of mortality, especially in diabetic patients. It is an atherosclerotic process that results in decreased ability to walk secondary to pain (known as intermittent claudication), as well as sensory deficits. Early medical and surgical intervention can help patients to have better outcomes.[44]
Compartment syndromes
The lower leg is the most prevalent site of compartment syndrome, especially in the context of tibial shaft fractures. This condition may occur in any of the four compartments of the lower leg; however, it most commonly occurs in the anterior compartment. Timely identification of the development of compartment syndrome is vital to prevent the destruction of tissues.[45]
Talus Fracture
About 80% of the talus is covered with articular cartilage and has no true muscle or tendinous attachment. It receives blood in a retrograde fashion. Blood supply is disrupted often with talar neck fractures, which has a higher risk of delayed union and non-union. Displaced talar neck fractures are better treated with surgical fixation to minimize these risks.
Jones Fractures
The fifth metatarsal has particular importance of its blood supply as fractures of the base of the fifth metatarsal have a propensity to non-union secondary to avascular necrosis; this is because there is an avascular watershed zone between the most proximal aspect of the base, known as the proximal tubercle, and the diaphysis.[24] The proximal fifth metatarsal divides into three zones: zone 1 is the proximal tubercle, zone 2 is the metaphyseal-diaphyseal junction, and zone 3 is the proximal metaphysis. Fractures are usually through the second zone, which carries an increased risk of avascular necrosis. This necrosis is the reason it may be advisable to consider surgical fixation of these fractures, which has demonstrated a decreased rate of nonunion.[46]