Lidocaine
- Article Author:
- Gabriel Beecham
- Article Author:
- Pankaj Bansal
- Article Author:
- Trevor Nessel
- Article Editor:
- Amandeep Goyal
- Updated:
- 7/10/2020 10:40:38 AM
- For CME on this topic:
- Lidocaine CME
- PubMed Link:
- Lidocaine
Indications
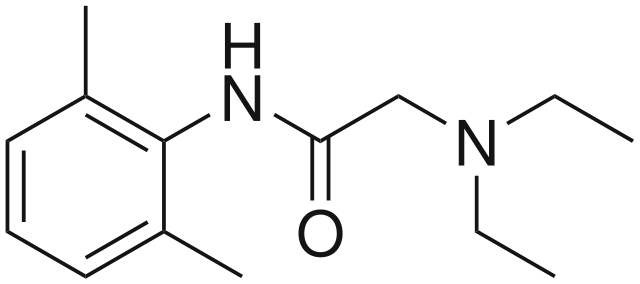
Lidocaine, formerly also referred to as lignocaine, is an amide local anesthetic agent. First synthesized between 1943 and 1946 by Nils Löfgren and Bengt Lundquist, it is a tertiary amine derived from xylidine, and its use rapidly became widespread given its superior safety profile compared to older local anesthetic agents.[1] The drug is commonly used for local anesthesia, often in combination with epinephrine (which acts as a vasopressor and extends its duration of action at a site by opposing the local vasodilatory effects of lidocaine). Given intravenously, it can be used during advanced airway management as an adjuvant to tracheal intubation, obtunding the hypertensive response to laryngoscopy and potentially reducing the incidence of myalgia and hyperkalemia when succinylcholine is given. Lidocaine is a class Ib antiarrhythmic agent on the Vaughan-Williams classification, and its use is indicated in the management of acute ventricular tachydysrhythmias. It also has roles as an adjuvant analgesic in the management of chronic pain.
Mechanism of Action
As with other local anesthetics, the site of action of lidocaine is at sodium ion channels on the internal surface of nerve cell membranes. The uncharged form diffuses through neural sheaths into the axoplasm before it then ionizes by combining with hydrogen ions. The resulting cation binds reversibly to sodium channels from the inside, locking them in the open state and preventing nerve depolarization. As lidocaine is a weak base with a dissociation constant (pKa) of 7.7,[2] approximately 25% of molecules will be un-ionized at a physiological pH of 7.4 and will be available to translocate inside the nerve cells, meaning that lidocaine has a more rapid onset of action than other local anesthetics with higher pKa values. Efficacy decreases in the presence of inflammation; this can be due to acidosis decreasing the proportion of un-ionized lidocaine molecules, a faster decrease in lidocaine concentration due to increased blood flow, and potentially also increased production of inflammatory mediators like peroxynitrite which act directly on sodium channels.[3]
In cardiac myocytes, lidocaine slows the rise of the cardiac action potential during phase 0, thereby increasing the effective threshold potential.
Lidocaine is 65% protein-bound to albumin and alpha1-acid glycoprotein in the plasma, giving it a medium duration of action compared to other local anesthetic agents. It is less lipid soluble than other agents, limiting its overall potency. Its volume of distribution is 0.7 to 1.5 L/kg and is hepatically metabolized.
Administration
Various routes of administration utilize different preparations of lidocaine.
- Very dilute concentrations, in the order of 0.05 to 0.1%, can be infiltrated subcutaneously in large volumes to provide tumescent local anesthesia, resulting in swelling and firmness of the site which may be beneficial for certain surgical procedures.
- Dilute solutions of 0.25 to 0.5% are used for intravenous regional anesthesia (Bier's block) or infiltration into subcutaneous tissue.
- 1 to 2% solutions are used for regional nerve blocks including epidural anesthesia and are also available in intravenous preparations for antiarrhythmic use.
- 1 to 2% aqueous gels, typically including an antiseptic such as chlorhexidine, are used to topicalize and lubricate the urethra prior to procedures like Foley catheterization.
- 4% solution is used for topical anesthesia of the mucous membranes of the airway, including the mouth, pharynx and respiratory tract, either by gargling, spraying or using an atomizer.
- 5% ointment, typically mixed with hydrocortisone, is employed topically on other mucous membranes such as the skin or in the rectum.
- 10% solution is also used topically for airway anesthesia, typically by spraying from a metered dose atomizer.
The aqueous preparations from 0.5 to 2% are available in either plain forms or with 1 per 200000 epinephrine (dentistry sometimes uses versions with 1 per 100000 epinephrine or more) and are available with or without preservatives. Other products include medicated plasters impregnated with lidocaine, intended to treat chronic postherpetic neuralgia. Lidocaine and prilocaine are available premixed in a eutectic 5% cream (containing 2.5%) which is often used to anesthetize small areas of skin prior to procedures.
Doses used for infiltrative or regional anesthesia will depend on the specific block. When lidocaine is used to obtund airway reflexes, the dose is 1 to 2 mg/kg given 2 to 5 minutes before intubation. For cardiac dysrhythmias, the initial dose is 1 to 1.5 mg/kg given intravenously, optionally followed with an infusion.
Adverse Effects
Most side effects occur when plasma concentrations rise to toxic levels. The drug reaches the intravascular compartment most rapidly when it is administered into the intercostal space, followed by the caudal, epidural, brachial plexus, femoral and subcutaneous spaces. The maximum safe dose by body weight may be taken to be 3 mg/kg, or 7 mg/kg when using preparations with epinephrine, although the literature quotes various other doses. Smaller amounts than this can still result in side effects and toxicity if given intravascularly.
Lidocaine is thought to be more neurotoxic than other local anesthetics, especially when high concentrations applied directly to nervous tissue. Use of highly concentrated lidocaine (2.5 to 5%) for spinal anesthesia correlates with a greater incidence of transient radicular irritation syndrome, which is a self-limiting painful condition affecting the calves, thighs, and buttocks.[4]
Contraindications
The drug is contraindicated in patients with a known severe adverse reaction. Anaphylactic reactions to lidocaine are possible but rare.
Methemoglobinemia can occur due to lidocaine metabolism to O-toluidine.[5] This metabolite is more likely when very high doses are given, but it may also occur with lower doses where the patient is taking other medications that can precipitate methemoglobinemia, or where the patient has a hemoglobinopathy or another cause of anemia.
Lidocaine should not be used as an antiarrhythmic if the dysrhythmia may be secondary to local anesthetic toxicity.
Lidocaine preparations containing epinephrine cause demonstrable cardiovascular effects even if only given in small amounts, and it is prudent for basic hemodynamic monitoring to be carried out before and during use solutions containing vasopressors, particularly if there is any specific concern over the patient's cardiovascular status.[6]
Monitoring
Lidocaine has a narrow therapeutic index, and plasma level monitoring may be necessary for patients with hepatic impairment who are on prolonged infusions.
Toxicity
Signs and symptoms of mild toxicity become apparent at plasma levels greater than 5 mcg/mL, beginning with slurred speech, tinnitus, circumoral paresthesiae and feeling faint. Above 10 mcg/mL, the patient may experience seizures or loss of consciousness. The myocardium and central nervous system are further depressed at 15 mcg/mL, progressing to cardiac arrhythmias, respiratory arrest and cardiac arrest above 20 mcg/mL.[6] Animal studies suggest that the dose of lidocaine required to result in cardiovascular collapse is 7.1 times higher than the dose needed to induce seizures.[8] This ratio is significantly higher than other local anesthetic agents, meaning that lidocaine may be less likely than other local anesthetics to progress rapidly through neurological signs and symptoms to full cardiovascular collapse in cases of toxic dosing.
Administration of the drug should immediately cease if toxicity is suspected. In the case of cardiorespiratory collapse, there should be airway support and breathing assistance to prevent the development of respiratory acidosis, which may exacerbate toxicity and potentiate lidocaine's negative chronotropic and inotropic effects.[7] Vital function support including oxygen, IV fluids, and inotropes should be instituted if required. Intravenous lipid emulsion is indicated as a rescue therapy, especially in cases of refractory cardiovascular collapse.[8]
Enhancing Healthcare Team Outcomes
All healthcare workers including PAs and nurse practitioners who use lidocaine should be familiar with its toxicity and how to manage it. Lidocaine may cause significant pain on initial injection due to the agent stimulating nociceptors before it exerts its effects on sodium channels; this can be counteracted by buffering the lidocaine with small volumes of sodium bicarbonate shortly before use, making the solution less acidic.[9] Pain can also be reduced by warming the solution to body temperature, injecting more slowly, using narrow cannulas, and injecting at 90 degrees to the skin.[10]