Lower Extremity Blocks
- Article Author:
- Thomas Rodziewicz
- Article Author:
- Samir Patel
- Article Editor:
- Emily Garmon
- Updated:
- 9/7/2020 10:03:23 AM
- For CME on this topic:
- Lower Extremity Blocks CME
- PubMed Link:
- Lower Extremity Blocks
Introduction
The lumbosacral plexus (L1 to S4 nerve roots) innervates the lower extremity. Unlike the brachial plexus in the upper extremity, the lumbosacral plexus is not easily blocked with a single-injection technique. Consequently, neuraxial blocks were preferred in the past when lower extremity anesthesia or analgesia was desired. As technological advancements have increased the number of outpatient procedures, neuraxial techniques have become less desirable.[1][2][3][4] Simultaneously, ultrasound-guided techniques have gained widespread use and popularity, which has improved the identification of individual nerves and accuracy of lower extremity blocks. Although two or more separate injections are usually required for a complete lower extremity block, this is often the best option available for outpatients.
Anatomy and Physiology
The lumbosacral plexus divides into four nerves (femoral, lateral femoral cutaneous, obturator, and sciatic), which entirely innervate the lower extremity. The femoral nerve provides sensation and motor function to the anterior thigh. It continues as the saphenous nerve to provide sensation to the medial leg, foot, and great toe. The lateral femoral cutaneous nerve supplies sensation in the lateral thigh. The obturator nerve supplies sensory to the medial thigh and motor to the thigh adductors. Neither the lateral femoral cutaneous nor the obturator nerve have any sensory or motor input to the lower leg. The sciatic nerve runs with the posterior cutaneous nerve of the thigh and provides sensory and motor to the posterior thigh. The sciatic nerve continues posteriorly and divides into the tibial and common peroneal nerves just cephalad to the popliteal fossa, and provides sensory and motor to the anterior, lateral, and posterior lower leg. Five nerves provide sensory and motor to the foot:
- Saphenous nerve supplies sensation to the medial foot and a portion of the great toe
- Deep peroneal supplies the web space between the great toe and the second toe
- Superficial peroneal nerve supplies the majority of the dorsum of the foot and toes
- Sural nerve supplies the lateral foot and a portion of the fifth toe
- Posterior tibial nerve divides into the medial and lateral plantar nerves, and supplies the sole and plantar surface of the toes.
Indications
Lower extremity blocks are useful in providing targeted anesthesia to the hip, knee, ankle, or foot. Particularly in patients for whom general or neuraxial anesthesia are contraindicated, local blocks may be a useful alternative to provide adequate analgesia. Furthermore, blocks are frequently utilized post-operatively to improve pain control and lower the opioid burden acutely post-operatively. There is the added effect of restoring mobility to patients who may otherwise be limited by pain in the early postoperative period. This early mobilization is important in minimizing complications such as venous thromboembolism and bedsores, as well as progressing early in physical therapy.[5][6]
Contraindications
Lower extremity blocks should not be performed under the following conditions:[7][8]
- Presence of coagulopathy - In patients with a high risk of venous thromboembolism, nerve blocks may blind practitioners to early signs of a DVT
- Low platelet count, or anticoagulated patients - Patients with a high risk of bleeding may experience bleeding at the injection site, which could present complications for the procedure
- Skin infection at the site of the block - The introduction of a needle through a skin infection may frequently result in seeding the lower extremity or nerve with a deep infection
- Allergy to local anesthetic - Patients with a demonstrated drug allergy to the anesthetic agent of choice should not undergo a lower extremity block for risk of anaphylaxis or other allergic response
Equipment
Equipment used includes:
- Povidone iodine solution or chlorhexidine
- Sterile towels and gauze
- Sterile gloves (gown is required for catheter placement, but not single shot block)
- Control syringe to aspirate before injection of local anesthetic (block volume is typically 20 mL to 40 mL)
- Needles (18 or 20 gauge needle for drawing up the local anesthetic and a 25 gauge needle for injection)
- Local anesthetic with epinephrine and/or other additives, such as dexamethasone or dexmedetomidine
Personnel
It is important to understand that a lower extremity block is a minor procedure but has the potential to cause major complications. Thus, the procedure should be performed in a designated area with standard American Society of Anesthesiologists (ASA) monitors, intravenous access, and resuscitation drugs and equipment immediately available, including intralipid.
Technique
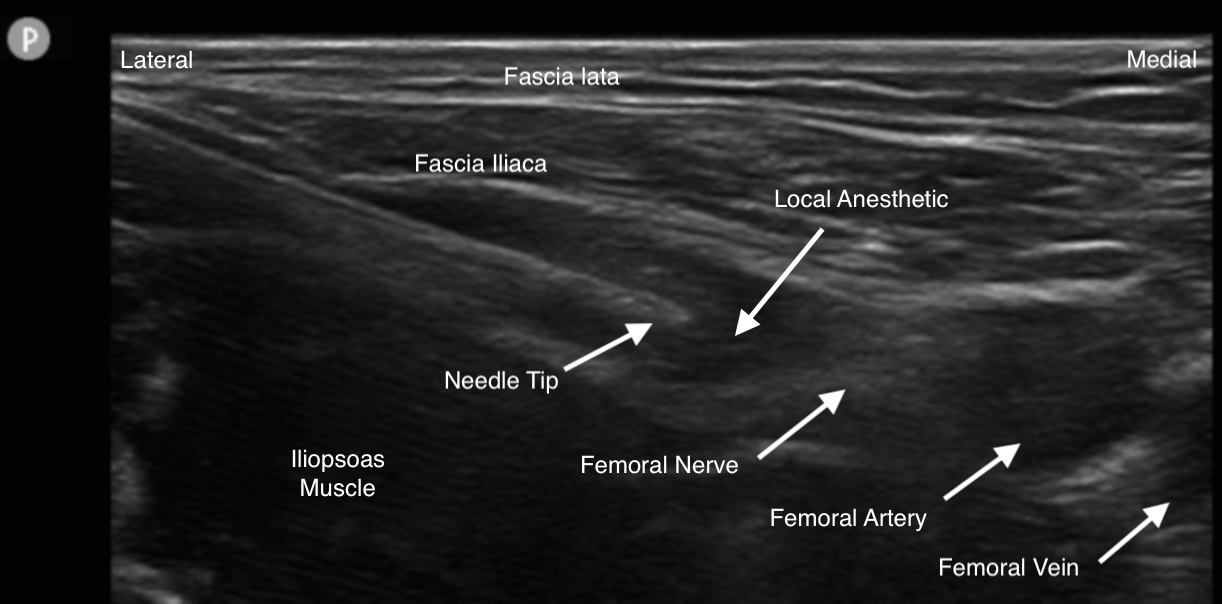
The femoral nerve can be blocked deep to the fascia iliaca just caudad and medial to the anterior superior iliac spine (fascia iliaca compartment) or at the femoral crease. Anatomic, stimulator, and ultrasound-guided techniques have been described. The fascia iliaca is a continuous band of fascia in this region, so local anesthetic injected under this fascia reliably produces a block of the femoral and lateral femoral cutaneous nerves. The obturator nerve is less reliably blocked the more caudad the block is performed. The saphenous nerve can be blocked at the mid-shaft femur (adductor canal) or with a field block at the tibial plateau. Saphenous nerve blocks have gained recent popularity because the sensation is blocked while sparing motor function for ideal physical therapy and rehabilitation.
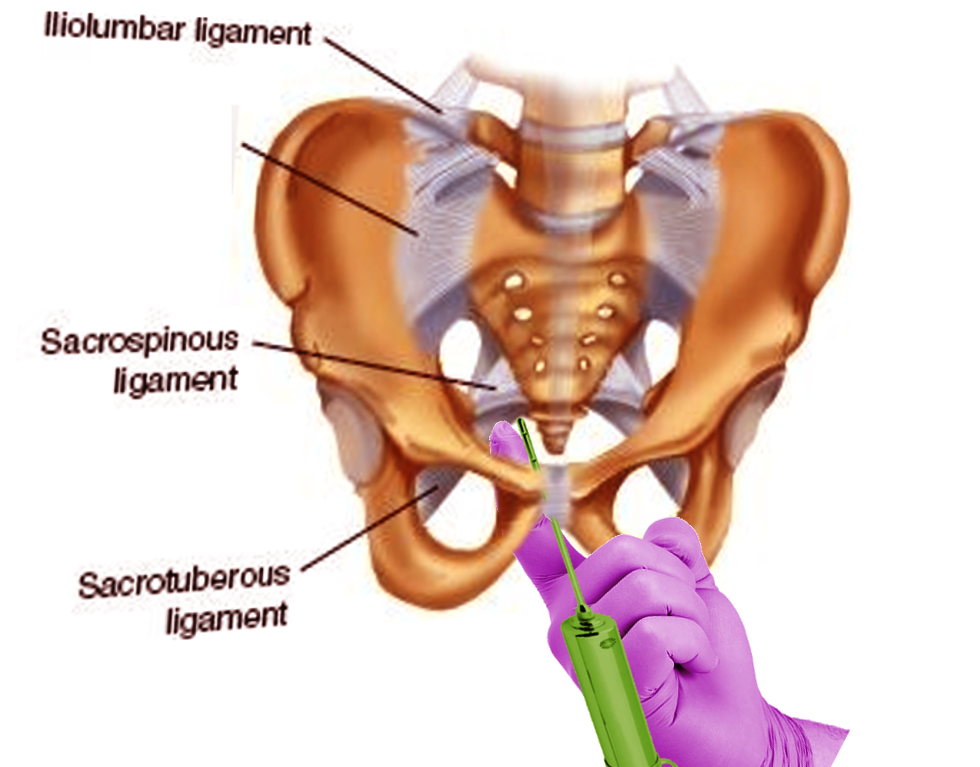
The sciatic nerve is blocked in the gluteal region (classical approach) between the greater trochanter and ischial tuberosity, just deep to the gluteus muscles and superficial to the quadratus femoris. The sciatic nerve can also be blocked as it travels through the thigh adductors (anterior sciatic approach). Finally, the sciatic nerve can be blocked approximately 6 cm above the popliteal fossa (popliteal block) before the nerve dividing into the tibial and common peroneal nerves. Anatomic and ultrasound-guided approaches have been described for the blockade of the sciatic nerve at these three main locations.
A complete block of the foot can be accomplished at the ankle with five injections. The saphenous nerve is blocked anterior to the medial malleolus. The deep peroneal nerve is blocked at the anterior ankle between the extensor hallucis longus and extensor digitorum longus. The superficial peroneal nerve is blocked anterior to the lateral malleolus. The sural nerve is blocked between the lateral malleolus and the Achilles tendon. The posterior tibial nerve is blocked posterior to the medial malleolus.
Complications
Local Complications from the Injection
- Hematoma
- Infection
- Injury to the nerve
- Anesthetic blockade of adjacent structures
- Block failure
Systemic Toxicity
- Dizziness, lightheadedness
- Blurred vision
- Ringing, buzzing in ears
- Metal taste in mouth
- Numbness/tingling around mouth, fingers or toes
- Drowsiness or confusion
- Seizures and cardiac arrest
Clinical Significance
The femoral nerve block includes both motor and sensory nerves. This block can be used for surgery on the knee or repair of trauma to the medial aspect of the upper and lower extremity. After the procedure, the patient will have marked weakness in the quadriceps and should not be allowed to ambulate until all sensation has returned.
The adductor canal block is similar to the femoral nerve block but only affects the lower extremity and blocks the sensory nerves. It can also be used for surgery on the knee and medial aspect of the lower leg.
The popliteal block at the knee is often used for surgery on the lower extremity.
The fascia iliac compartment block can block the femoral, obturator and lateral femoral cutaneous nerves. It is often used for hip fractures and total hip arthroplasties. The block provides prolonged pain relief in the hip, anterior and medial thigh area.
Most lower extremity blocks last 6 to 24 hours. However, it is important to remember that sometimes these local nerve blocks may not work or the duration may be short. Other options for lower extremity blocks include the use of spinal and epidural anesthesia.
Enhancing Healthcare Team Outcomes
Lower extremity blocks are usually performed by anesthesiologists but it is vital that a nurse is dedicated to the monitoring of the patient. Resuscitative equipment must be in the room where the procedure is being done. Complications, though rare, do have the potential to cause cardiac or respiratory arrest, bleeding and nerve damage.[9] an interprofessional team approach will provide the safest and best results for the patient. [Level V]
(Click Image to Enlarge)