Anatomy, Shoulder and Upper Limb, Hand Lumbrical Muscles
- Article Author:
- Michael Valenzuela
- Article Editor:
- Matthew Varacallo
- Updated:
- 9/17/2020 11:32:23 PM
- For CME on this topic:
- Anatomy, Shoulder and Upper Limb, Hand Lumbrical Muscles CME
- PubMed Link:
- Anatomy, Shoulder and Upper Limb, Hand Lumbrical Muscles
Introduction
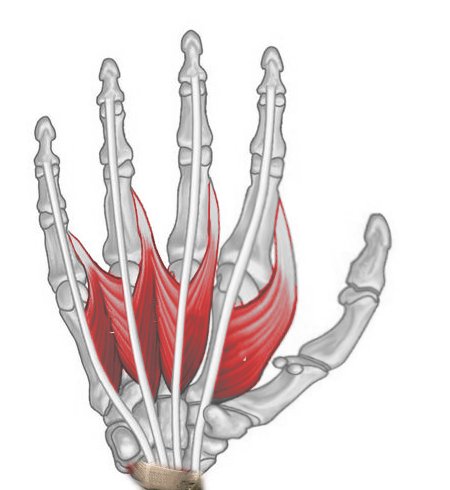
The lumbrical muscles of the hand are a group of four intrinsic hand muscles. Due to their cylindrical, “worm-like” appearance, the lumbricals are named after the earthworm genus Lumbricus. All four lumbricals flex their respective metacarpophalangeal joint and extend the proximal interphalangeal and distal interphalangeal joints. The lumbricals are unique in that both their origins and insertions are tendons (Figure 1). Another peculiarity is that fact that the lumbricals arise from their partial antagonist, the flexor digitorum profundus.
Structure and Function
The first two, lateral lumbricals are unipennate muscles. The first lumbrical originates on the lateral side of the first tendon of the flexor digitorum profundus and inserts into the extensor hood of the second digit. The second lumbrical originates on the lateral side of the second tendon of the flexor digitorum profundus and inserts into the extensor hood of the third digit.
The third and fourth, medial lumbricals are bipennate muscles. One head of the third lumbrical originates on the medial portion of the second tendon of the flexor digitorum profundus while the other head originates at the lateral portion of the third tendon of the flexor digitorum profundus. The third lumbrical inserts into the extensor hood of the fourth digit. The lateral head of the fourth lumbrical originates at the lateral surface of the fourth tendon of the flexor digitorum profundus while the medial head of the fourth lumbrical originates at the lateral portion of the fourth tendon of the flexor digitorum profundus. The insertion site for the fourth lumbrical is the extensor hood of the fifth digit.
Functions of the lumbricals include flexion at the respective metacarpophalangeal (MCP) joint and extension at the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints. Interestingly, the lumbricals arise from their partial antagonist, the flexor digitorum profundus. Besides providing flexion at the wrist and MCP joint, the flexor digitorum profundus flexes the PIP and DIP joints, whereas the lumbricals are extenders of the PIP and DIP joints. The tendons of all lumbricals pass anteriorly to the deep transverse metacarpal ligaments.
Embryology
By the completion of the fourth week of embryonic development, four limb buds arise from somites and mesenchyme of the lateral plate mesoderm that is covered by a layer of ectoderm.[1][2] Development of the upper extremities is propagated by a plethora of protein factors, with fibroblast growth factors (FGF) and Sonic hedgehog (Shh) playing vital roles. The gene expression and subsequent interactions of these various proteins contribute to the development of three spatial limb axes: proximodistal, anteroposterior, and dorsoventral.[1][2]
Development of the hand begins with flattening of the distal upper extremity buds around days 34-38 of embryonic development. Somites form the limb musculature while mesenchyme of the lateral plate mesoderm forms bone and cartilage. Somitic mesoderm of the hand divides into superficial and deep layers, with the superficial muscles developing earlier than deep muscles. The lumbrical muscles originate from the deep layer of this mesoderm, and by the twelfth week of development, tendons are fully developed and functional.[2]
Blood Supply and Lymphatics
Vascular supply to the lumbricals arises from four different vessels. The superficial palmar arch provides the primary supply to the lumbricals, with deep palmar arch, dorsal digital arteries, and palmar digital arteries also contributing.
Lymphatic drainage of the upper limbs divides into superficial and deep lymphatic drainage. Lymphatic plexuses of the skin of the palm and dorsum of the hand ascend with the cephalic and basilic veins towards the axillary and cubital lymph nodes, respectively. Deep lymphatic vessels follow the primary deep veins and eventually terminate in the humeral lymph nodes.
Nerves
Innervation of the first and second lumbricals is by the digital branches of the median nerve. The third and fourth lumbricals receive innervation from the deep branch of the ulnar nerve.
Physiologic Variants
Classical teaching says that the median nerve innervates the lateral two lumbricals, and the ulnar nerve innervates the medial two lumbricals. While this is the case for roughly 50-60 percent of hands, 20-30 percent of hands have median nerve innervation to only the first lumbrical with approximately 20 percent of hands having median nerve innervation to the first three lumbricals.[3] Furthermore, one cadaveric study found that the third lumbrical possessed dual innervation from both median and ulnar nerves in 64 percent of specimens.[4] While innervation to individual lumbricals can be quite variable, most agree that the first lumbrical always receoves its nerve supply from the median nerve, and the fourth lumbrical is always innervated by the deep branch of the ulnar nerve.[3][4][5]
Other physiological variations of the lumbrical muscles include a double first lumbrical and a bipennate second lumbrical, which were found in roughly 10 percent of specimens in one study. This study also found an absent third lumbrical in two percent of specimens.[3]
Distal insertions sites also show high variability in the lumbricals, with an increasedg variability from lateral to medial lumbricals. Such locations include the proximal phalanx, volar aspect of the metacarpophalangeal joint, the extensor hood, or any combination of these sites.[6] Additional insertions into the extensor hood are most common in the first lumbrical, and attachments to bone and the volar plate are most common in the fourth lumbrical.[6][7]
Surgical Considerations
The use of lumbrical flaps has been described in cases of carpal tunnel syndrome and other median nerve injuries, such as neuromas in continuity.[7] One case study looked at a diabetic patient with a hand infection leading to exposure of the median nerve. Due to the acuity of inflammation, soft tissue reconstruction was not advised at this time. The authors subsequently used the first lumbrical to cover the exposed median nerve to avoid further damage.[7] This same study examined a patient that was surgically treated for carpal tunnel syndrome of her right hand. The patient presented to the authors after her pain persisted despite aggressive intervention. Upon re-exploration, the median nerve was found compressed within extensive scar tissue. The authors used the second lumbrical to cover the median nerve to buffer it from the overlying scar tissue with the continued resolution of symptoms 18 months after.[7]
Another study used intrinsic muscles of the hand as flaps for painful neuromas in continuity. In half of the patients, the authors used lumbrical flaps to cover the injured nerve after neurolysis, with all patients reporting relief of their pain.[8] While there was concern regarding a possible decrease in hand strength due to translocation of a lumbrical, the authors found no significant changes in strength or hand function as noted by the patients.[8]
Clinical Significance
While the lumbrical muscles have shown use in protecting the median nerve from further injury, several reports have shown that aberrant lumbrical anatomy can cause damage to the nerve.[3][9][10][11] If the lumbrical origin is too proximal, or even within the carpal tunnel at rest, then the median nerve is at higher risk of compression and subsequent injury.[9][10][11] Moreover, any lumbrical with anomalous origin can hypertrophy secondary to overuse, resulting in carpal tunnel syndrome.[12]
As previously discussed, the first two lumbricals are typically innervated by the median nerve. As such, any insult to the median nerve, including penetrating trauma, compression injury, brachial plexus injury, or infection may result in weakness or atrophy of the lateral two lumbricals. Additionally, any injury to the ulnar nerve can manifest as weakness or even atrophy of the medial lumbrical muscles. Entrapment of the ulnar nerve ranks asis the second most common compression neuropathy patients present with, and it is typically caused by nerve root impingement, brachial plexus compression, or nerve entrapment at the elbow, forearm, or wrist.[13]
For clinicians to assess lumbrical muscle strength, with the palm supine, the patient is instructed to flex the metacarpophalangeal joints while keeping the interphalangeal joints extended. The clinician then applies a counterforce along the palmar surface of the proximal phalanx of digits 2-5 individually. Resistance may also be applied separately on the dorsal surface of the middle and distal phalanges of digits 2–5 to test extension of the interphalangeal joints while maintaining flexion of the metacarpophalangeal joints.