Lupus Miliaris Disseminatus Faciei
- Article Author:
- Nathaniel Slater
- Article Editor:
- Ronald Rapini
- Updated:
- 8/10/2020 4:42:23 PM
- For CME on this topic:
- Lupus Miliaris Disseminatus Faciei CME
- PubMed Link:
- Lupus Miliaris Disseminatus Faciei
Introduction
Lupus miliaris disseminatus faciei (LMDF) is an idiopathic granulomatous disease affecting facial skin primarily. Nosologically, it is on a spectrum of facial granulomatous dermatoses and shares overlapping features with rosacea and sarcoidosis. In most cases, this disorder resolves spontaneously within several years but can leave potentially disfiguring scarring.
The name derives from a historic putative association with tuberculosis, as discussed below. More recent authors have proposed adopting the term facial idiopathic granulomas with regressive evolution (FIGURE) instead of the entrenched LMDF. However, it does not appear that a name change has been widely accepted.[1] Older terms for a similar facial granulomatous dermatosis include micropapular tuberculid, Lewandowsky’s eruption, and lupoid rosacea.[2] Acne agminata has been used to refer to similar lesions in the axilla.
Etiology
The etiology of LMDF is uncertain. The earliest reports presumed that lesions of LMDF were related to tuberculosis based on similar clinicopathologic findings to other tuberculids. The term tuberculid was historically used for reactive conditions associated with tuberculosis, in which the actual infectious agent is present elsewhere and is not found in the skin lesions. However, nowadays, LMDF does not arise in association with pulmonary tuberculosis and does not generally respond to anti-tuberculous medications. Tuberculin skin testing is often negative in these patients.[3] Moreover, investigations, including histochemical staining for mycobacteria and tissue cultures, as well as PCR based studies, have consistently failed to demonstrate evidence of M. tuberculosis organisms within the LMDF granulomas.[4][5] A possible relationship with an unknown non-tuberculous mycobacterium has not been completely excluded.[4]
Similar to other facial granulomatous eruptions, it is often postulated that initial immune-mediated damage to the hair follicle leads to subsequent rupture of the follicle and an allergic or foreign body granulomatous response to keratin, sebum, or microbial components in the dermis.[6] This hypothesis is supported by observations that the granulomatous infiltrate is often centered around a follicular structure, which can sometimes be seen on serial histologic sectioning if not initially evident.[1] It is unknown whether altered antigenicity of the hair follicle or sebaceous gland structures with subsequent T-cell mediated destruction or other disruption of the pilosebaceous unit is the inciting event. A relationship with hormonal effects on the pilosebaceous unit, as seen in certain acneiform variants, has not been shown.[1]
Epidemiology
LMDF is uncommon, although precise incidence rates are not well reported. LMDF can be seen across a wide range of ages, but most commonly presents in young adults (33 years was the average age in one series) and is rare in older adults.[5] A clear gender predilection has not been established, though in one retrospective review, the average age of females (43 years old) was older than male patients (23 years old), and all patients beyond their mid-30s were female.[7]
Pathophysiology
LMDF has been considered by some as a variant of granulomatous rosacea, whereas other authors make the case for LMDF as a distinct entity.[8] The different clinical manifestations of rosacea are thought to result from the same underlying inflammatory pathways, including abnormalities of the innate immune system and neurovascular aberrations.[9] However, these vascular abnormalities are not seen in patients with LMDF. Demodex folliculorum mites are often found in skin biopsies from patients with rosacea and may play an etiologic role, but Demodex mites have not been consistently observed in skin biopsies from patients with LMDF.[1][4]
As above, a ruptured follicular infundibular cyst has been found in histologic sections of some patients with LMDF.[4] Using a PCR assay, one study of nine patients with LMDF demonstrated higher levels of Propionibacterium acnes bacteria within granulomatous areas separated by microdissection, as compared with normal-appearing regions of skin. The authors suggested that the presence of P. acnes in the dermis around a disrupted hair follicle, in combination with host factors, may play a role in pathogenesis.[10]
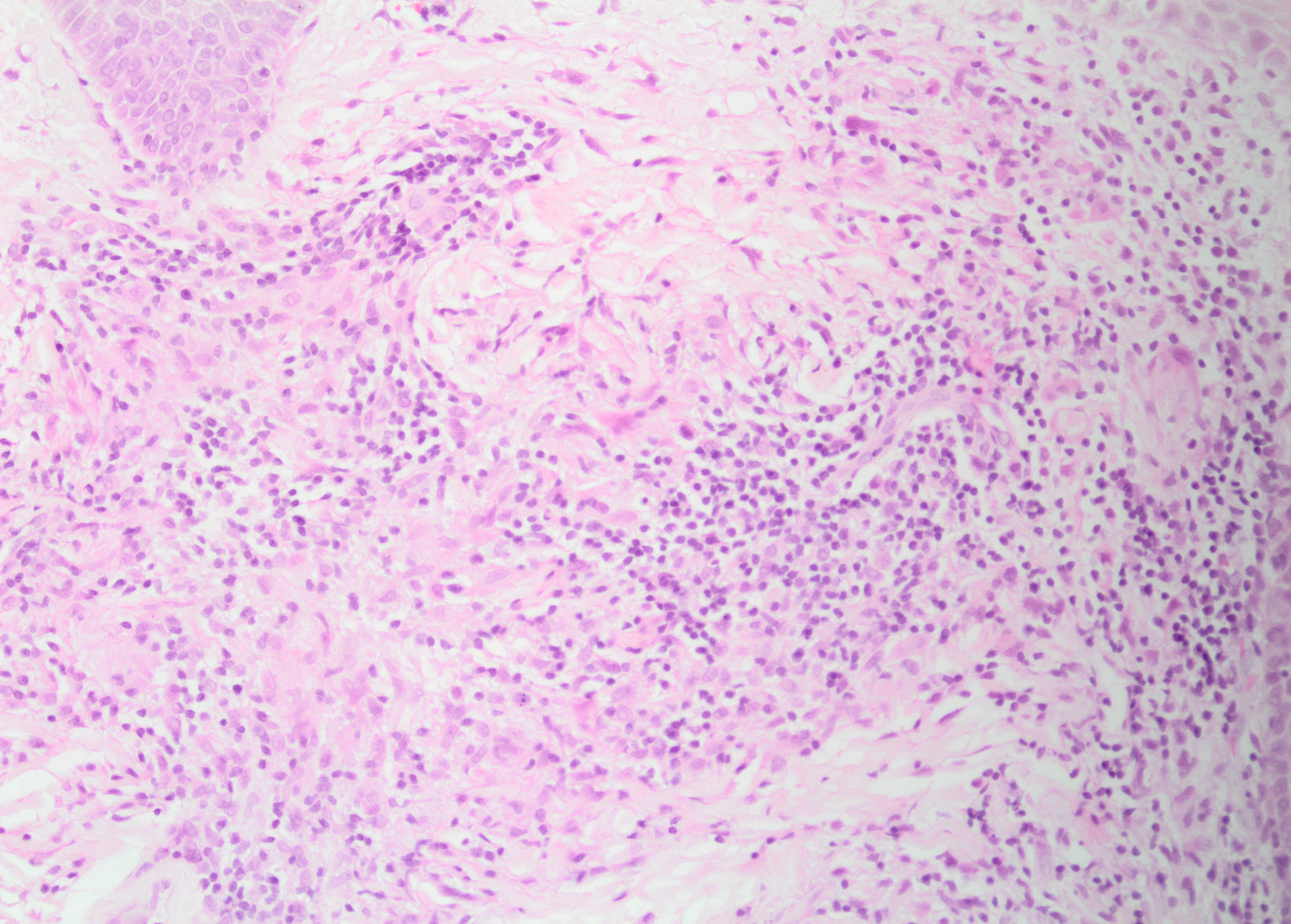
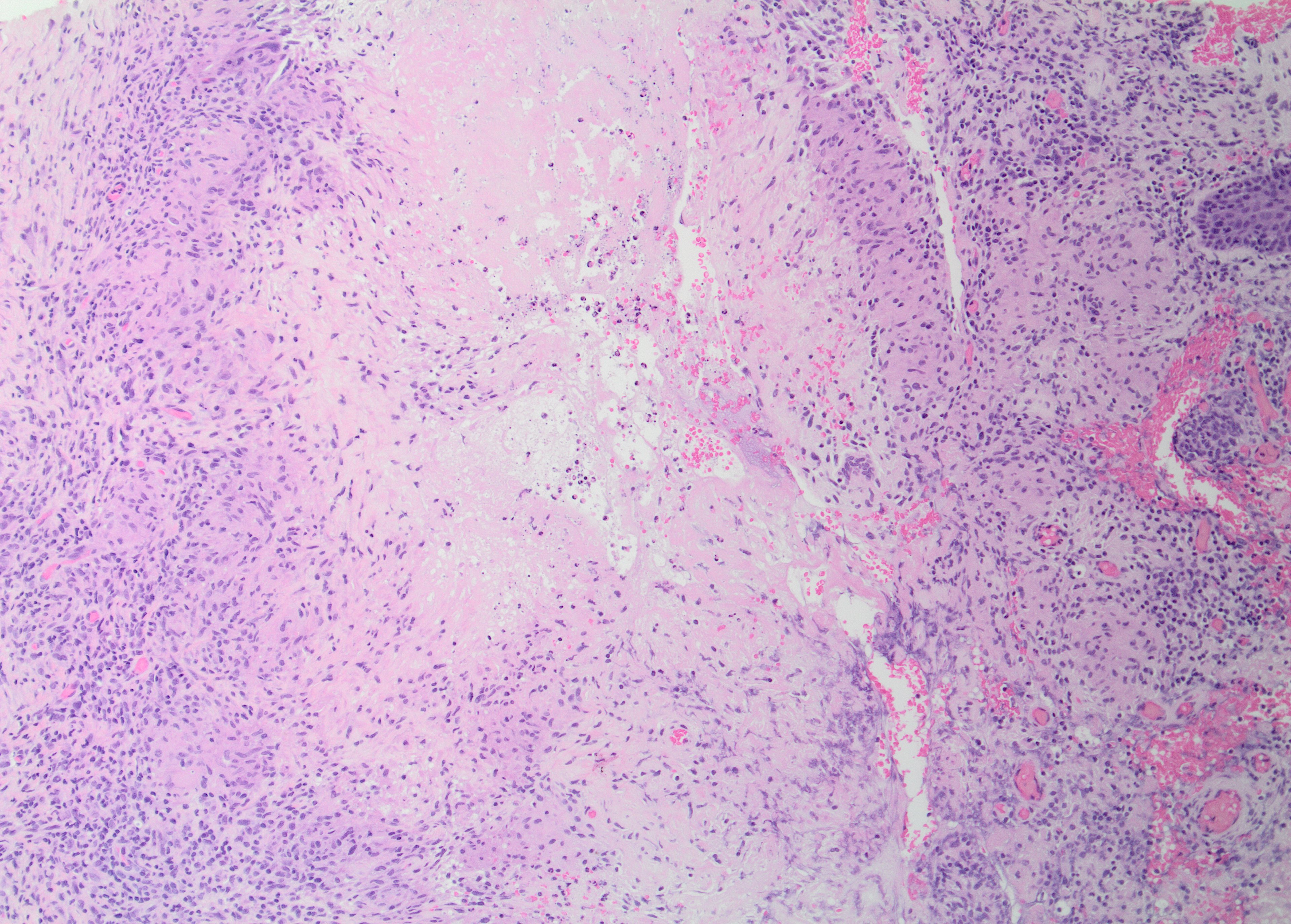
Histopathology
The histologic hallmark of LMDF is a granulomatous infiltrate, in some cases centered around hair follicle structures. Both sarcoidal (non-caseating) and tuberculoid (with central caseation necrosis) granulomas have been observed, as have diffuse infiltrates of lymphocytes and histiocytes without well-formed granulomas. The latter may be characteristic of early lesions, and may also demonstrate a peri-adnexal pattern. Accompanying neutrophils with or without neutrophilic microabscesses have been variably observed. Fibrosis is seen in late lesions, correlating with clinical scar formation. There is significant histologic overlap with granulomatous rosacea and other granulomatous disorders affecting the face.[1]
History and Physical
Patients often present with a relatively abrupt onset of asymptomatic red, yellow, brown, or skin-colored papules or nodules, which are occasionally pustular and symmetrically distributed predominantly on facial skin. The lower eyelids are most characteristically involved, and involvement of forehead, cheeks, nose, upper lips, ears, chin, or neck is common.[4] Extra facial involvement is uncommon but has been reported in some cases, including on the trunk, extremities, and genital skin.[2] Co-morbidities have not generally been reported in association with LMDF.
Evaluation
Symmetrically distributed inflammatory papules or papulopustules with histologically confirmed granulomatous inflammation should lead to consideration of the diagnosis. A background of erythema, telangiectasias, or a propensity for flushing would favor a diagnosis of granulomatous rosacea, as would exacerbation of disease by such triggers as steroid use, sunlight, alcohol, or spicy foods.[1][5] Exclusion of an infectious etiology by histochemical stains (e.g., Ziehl-Neelson stain) and/or tissue cultures is often prudent, although the sensitivity of these tests is imperfect. Many authors have included serum calcium and angiotensin-converting enzyme levels in their workup, with or without chest X-ray and ophthalmologic exam, to help exclude sarcoidosis.[2] Serologic assays for tuberculosis and treponemal infection may also be considered.[4]
Treatment / Management
The evidence for treatment of LMDF is limited to case series and retrospective reviews and should be considered even though the disease course is usually self-limited. This disease tends to be poorly responsive to topical or systemic therapies that are first-line for granulomatous rosacea. The efficacy of oral tetracyclines is poor, whereas the response to isotretinoin is mixed.[8] In one series, patients demonstrated a better response to oral prednisolone (administered at starting doses of 10mg daily) or oral dapsone (100mg daily). The combination of these two agents seemed to be especially effective, including in patients who had failed monotherapy with either alone. In the same series, the combination of oral dapsone with topical tacrolimus was reported to produce an excellent response in 7 of 7 patients.[1] Other studies also report good responses to systemic corticosteroids.[11] Early, effective treatment may reduce the risk of significant scarring.
Differential Diagnosis
As discussed, cutaneous tuberculosis or other infections, especially fungal, mycobacterial, treponemal, or leishmanial, should be considered. A bilateral, symmetric, relatively rapid onset in an otherwise well patient without associated symptoms makes an infectious etiology less likely. If an infection is excluded, the clinical and pathologic differential may include granulomatous rosacea at one end of the spectrum, and cutaneous sarcoid at the other.
Like LMDF, granulomatous variants of rosacea can present with bilateral, symmetric facial papules with similar morphology. There is considerable histologic overlap, including relationship to pilosebaceous units, although LMDF may have larger granulomas that are more prone to caseation necrosis, and is not expected to have actinic damage, vascular dilation, or the presence of Demodex mites.[5] The clinical features and course may help discriminate these entities. Notably, LMDF occurs in the absence of phymatous changes, ocular involvement, or vascular manifestations of rosacea such as background erythema, flushing, or telangiectasia. Compared to rosacea, LMDF tends to affect adults at a younger age, including some cases in adolescents and exceptional cases in children and may affect men more commonly.[5] The involvement of eyelids, upper lips, and neck is more common in LMDF, and extra facial involvement can occur.[2] LMDF is more likely than rosacea to spontaneously resolve within several years, but more prone to significant pitted scarring. As discussed above, LMDF responds somewhat differently to treatment than rosacea, being less successfully treated with antibiotics and more successfully treated with corticosteroids.[1][2][4]
Sarcoidosis should be excluded by clinical and/or laboratory investigations, especially in those whose disease is slow to regress or shows progression.[6] While LMDF has also been proposed as a possible forme fruste of sarcoid, it lacks clinical, laboratory, or radiographic evidence of extracutaneous manifestations, and does not progress to visceral involvement. Histologically, the granulomatous infiltrate is more prone to caseation and often associated with pilosebaceous units.[2] Deep-seated, annular, or solitary lesions, or lesions involving the scalp or only a part of the face, should raise concern for the possibility of sarcoidosis.[6]
Other facial granulomatous disorders, including granulomatous perioral dermatitis, may also be considered in the differential.
Prognosis
LMDF is a skin-limited disease. The natural history of the disease is usually spontaneous involution over months to several years, with a mean duration of 18 months in one series.[7]
Complications
The primary long-term complication is facial scarring, which can be significant and disfiguring. Early treatment may prevent or minimize significant scarring.[1]
Deterrence and Patient Education
Unlike rosacea, there are no documented lifestyle risk factors for LMDF. Once the diagnosis is made after appropriate workup as above, patients should be reassured about the skin-limited nature of the disease, the expected eventual resolution, and the potential for treatment to reduce the risk of permanent scarring.
Enhancing Healthcare Team Outcomes
Patients with LMDF should be managed by an interprofessional team approach in order to improve outcomes. Primary care providers and dermatologists will be involved. Certain treatment options, including dapsone and systemic corticosteroids, require careful education and monitoring, which should be reinforced by and coordinated with nursing and pharmacy professionals. (Level 5)
(Click Image to Enlarge)
(Click Image to Enlarge)