
Mechanical Ventilation
- Article Author:
- Sean Hickey
- Article Editor:
- Al Giwa
- Updated:
- 4/22/2020 10:07:16 AM
- For CME on this topic:
- Mechanical Ventilation CME
- PubMed Link:
- Mechanical Ventilation
Introduction
Although mechanical ventilation can be a complex and seemingly elusive topic, expectations are that physicians and healthcare professionals who deal with critically ill patients have a basic familiarity with the management of a patient on a ventilator. Additionally, providers must also understand how applying mechanical ventilation affects patient physiology and response to disease states. The focus of this article will be on the management of the intubated patient in the first few hours of care on mechanical ventilation and will review the basics of mechanical ventilation.
The primary indications for mechanical ventilation are: [1]
- Airway protection in a patient who is obtunded or has a dynamic airway, e.g., from trauma or oropharyngeal infection
- Hypercapnic respiratory failure due to a decrease in minute ventilation
- Hypoxemic respiratory failure due to a failure of oxygenation
- Cardiovascular distress whereby mechanical ventilation can offload the energy requirements of breathing
- Expectant course, e.g., anticipated patient decline or impending transfer
Function
Mechanical ventilation works by applying a positive pressure breath and is dependent on the compliance and resistance of the airway system, which is affected by how much pressure must be generated by the ventilator to provide a given tidal volume (TV). The TV is the volume of air entering the lung during inhalation.[1] Compliance and resistance are dynamic and can be affected by the disease state(s) that led to the intubation. Understanding the changes in compliance and resistance will allow you to pick the proper ventilator strategies.
There are four stages of mechanical ventilation. [1] There is the trigger phase, the inspiratory phase, the cycling phase, and the expiratory phase. The trigger phase is the initiation of an inhalation which is triggered by an effort from the patient or by set parameters by the mechanical ventilator. The inhalation of air into the patient defines the inspiratory phase. The cycling phase is the brief moment when inhalation has ceased but before exhalation has begun. The expiratory phase is the passive exhalation of air from the patient.
Once the decision is made to place a patient on mechanical ventilation, the clinician may be presented with multiple different options on how to set up the ventilator. There are many kinds of modes of ventilation, such as assist-control (AC), synchronized intermittent mechanical ventilation (SIMV), and pressure support ventilation (PSV). [2] The ventilator can then be set to provide a given volume or pressure. Several leading voices in emergency medicine and critical care recommend utilizing volume assist control (VAC) as it is simple to use, safe, and available on all ventilators. [3] Further, it provides complete ventilator support which offsets fatigue in patients who are critically ill.
After choosing the mode, the rest of the parameters have to be set on the ventilator. These parameters are the respiratory rate (RR), inspiratory flow rate (IFR), the fraction of inspired oxygen (FI02), and positive end-expiratory pressure (PEEP). Respiratory rate is generally adjusted to move towards normocapnia, or to offset severe acidosis. The inspiratory flow rate is how fast the inspiration is provided, generally expressed in liters/minute. [2] FI02 is the fraction of inspired air and should be set to the lowest level to achieve an SP02 of 92-96%, as hyperoxemia has been shown to increase mortality in critically ill patients. [4] PEEP is used to increase the functional residual capacity, and to stent open collapsable alveoli thus reducing atelectatic-trauma. [1] Finally, all patients on mechanical ventilation should have the head of the bed elevated to at least 30 degrees and have continuous waveform end-tidal carbon dioxide (CO2) (ETCO2) monitoring. According to a 2016 Cochrane review on ventilator-associated pneumonia (VAP), "a semi-recumbent (30º to 60º) position reduced clinically suspected VAP by 25.7% when compared to a 0° to 10° supine position", however, they acknowledge that the data is severely limited. [5]
Issues of Concern
When placing a patient on mechanical ventilation, there is a change in their natural negative pressure ventilation to one of positive pressure ventilation; this will affect the heart-lung physiology and can alter the patient's hemodynamic status. The addition of positive pressure ventilation increases interthoracic pressure. The increase in interthoracic pressure will lead to a decrease in right ventricular preload, and left ventricular preload and afterload. It will also increase the right ventricular afterload. [6] While these effects could have a minimal change on a healthy person's hemodynamics, it can cause profound alterations in the hemodynamics of a critically ill patient. For example, a patient in acute pulmonary edema will benefit from the reduced preload while someone in septic shock would not.
Clinical Significance
Three clinical strategies may be chosen to assist in ventilator management.
Lung Protective Strategy:
This strategy should be used for any patient with the potential to develop acute lung injury (ALI) or whose disease state risks progression to acute respiratory distress syndrome (ARDS). This low tidal volume (LTV) strategy developed after the landmark ARDSnet trials, specifically the ARMA study, which showed that low tidal volume ventilation in patients with ARDS improved mortality. [7] This method is used to avoid barotrauma, volume trauma, and atelectatic trauma. Pneumonia, severe aspiration, pancreatitis, and sepsis are examples of patients with the acute potential to develop ALI and should be managed with the LTV strategy.
Tidal volume (TV) should be initially set at 6 ml/kg based upon ideal body weight.[8][7][9][10] As patients develop ALI and progress into ARDS, their lungs become progressively recruited and develop shunts, which leads to decreased functional lung volume. [3] A low tidal volume strategy offsets the decreased functional lung volume. Tidal volume should not be adjusted based on minute ventilation goals. Respiratory rate is adjusted based upon minute ventilation goals and the acid-base status of the patient. An initial rate of 16 breaths/minute is appropriate for most patients to achieve normocapnia. [11] A blood gas should be sent approximately 30 minutes after initiation of mechanical ventilation and RR adjusted based upon the acid-base status and PaCO2 of the patient. Normocapnia is a PaCO2 of 40 mmHg. If the PaCO2 is significantly greater than 40, then the RR should be increased. If the PaCO2 is significantly lower than 40, then the RR should be decreased. It is important to remember that the ETCO2 is not a reliable indicator of PaCO2 as the ETCO2 can be affected by the physiological shunt, dead space and decreased cardiac output. [3] Inspiratory flow rate should be set at 60L/minute. If the patient appears to be trying to inhale more during the initiation of inspiration, then it can be increased. [3]
Immediately after intubation, an attempt should be made to reduce the FI02 to 40% to avoid hyperoxemia. [4] From there, adjustments of the FI02 and PEEP are simultaneously controlled in the lung-protective strategy. Difficulty in oxygenation in ALI is due to de-recruited alveoli and physiological shunt. To counteract this, you should increase the FIO2 and PEEP together. The oxygenation goal of 88%-95% should follow the ARDSnet protocol. [9]
Table 1. ARDSnet PEEP/FIO2 Protocol [9]
Upon connecting a patient to mechanical ventilation, it is essential to frequently reassess its effects on the patient, especially the alveoli. This assessment is by examining the plateau pressure and driving pressure. The plateau pressure is the pressure applied to small airways and alveoli. The plateau pressure should be under 30, to prevent volume trauma, which is an injury to the lung secondary to overdistension of the alveoli. To obtain the plateau pressure, one must perform an inspiratory pause. Most ventilators have a button to calculate it. The driving pressure is the ratio of the tidal volume to the compliance of the lung, providing an approximation of the "functional" amount of lung that hasn't been de-recruited or shunted. [12] The driving pressure can be calculated simply by subtracting the amount of PEEP from the plateau pressure. [12] The driving pressure should remain below 14. If plateau and driving pressures start to exceed these limits, then decrease TV to 4ml/kg. Respiratory rate can be increased to compensate for the decrease in minute ventilation, though permissive hypercapnia might be necessary. Permissive hypercapnia is a "ventilation strategy to allow for an unphysiologically high partial pressure of carbon dioxide (PCO) to permit lung-protective ventilation with low tidal volumes." [13] Recruitment maneuvers have been found to increase mortality in moderate to severe ARDS and should not be routinely used. [14]
Obstructive Strategy:
Generally, patients with obstructive lung disease (OLD), such as asthma and COPD, are often treated with non-invasive ventilation. However, they sometimes require intubation and placement on mechanical ventilation. Obstructive lung disease is characterized by narrowed airways and the collapse of the small airways on expiration. [1] This condition leads to increased airflow resistance and decreases the expiratory flow, resulting in more time required to exhale the tidal volume fully. If inhalation begins before the full tidal volume has been exhaled, then there is some residual air left inside the chest. The intrathoracic pressure increases as more and more air gets trapped inside the alveoli. This pressure is termed auto-PEEP, and this pressure must be overcome during inhalation. As the amount of air trapped inside the chest increases, you have to flatten off the diaphragm and expansion of the lungs which decreases compliance; called dynamic hyperinflation. As auto-PEEP and dynamic hyperinflation progress, there is an increased work of breathing, decreased efficiency of inhalation, and potential for hemodynamic instability due to the high intrathoracic pressure. Given these unique circumstances in OLD, the ventilator strategy employed must offset these pathologically increased intrathoracic pressures. Furthermore, ventilatory management must be combined with maximal medical therapy such as in-line nebulizers to reverse the obstructive process.
The most important thing to accomplish when managing the ventilator for an obstructive patient is to increase the expiratory phase, which will allow for more time to exhale, which in turn will reduce auto-PEEP and dynamic hyperinflation. [1][3][11] It is important to recall that most patients will require deep sedation in order not to over-breathe the ventilator, and inspire too often. The tidal volume should be set at 8ml/kg, while the respiratory rate should start at ten breaths per minute. [3] These settings will allow for ample time for a full expiration and hence decreased auto-PEEP which tends to employ the above described permissive hypercapnia strategy by focussing on lowered tidal volumes and oxygenation over elevated PaCO2. Inspiratory flow rate should be set at 60 L/minute. FI02 should be set at 40% after the initiation of ventilation. As obstructive lung disease is typically a problem with ventilation and not one of oxygenation, the FIO2 should not need to be increased. Minimal PEEP should be employed, with some studies advocating for a PEEP of zero while some advocate for a small amount of PEEP to help overcome auto-PEEP. [3][11] The plateau pressure should be less than 30.
The ventilator waveform requires careful assessment. If the waveform does not reach zero by the beginning of the new breath, then the RR must be decreased, or else hyperinflation and auto-PEEP will rise. If an obstructive patient suddenly desaturates or drops their blood pressure, they should be disconnected from the vent to allow for a full exhalation with a clinician pushing on their chest to facilitate exhalation. After this, a full work-up specifically ruling out pneumothorax due to volume trauma should be undertaken. [11] If plateau pressures are chronically high, then pneumothorax must also be ruled out.
Intermediate Strategy:
The PReVENT trial showed no difference in an intermediate tidal volume strategy (10ml/kg) versus a low tidal volume strategy (6ml/kg) in patients without ARDS.[15] If the patient is being placed on mechanical ventilation and has no obstructive physiology or risk to develop acute lung injury, then an intermediate tidal volume strategy using 8-10ml/kg could be employed. Generally, as this patient would not have oxygenation or ventilation difficulties, minimal ventilator settings could be employed. Starting with a tidal volume of 8ml/kg, RR of 16, IFR of 60 L/minute, FIO2 of 40%, and PEEP of 5, with titration as needed, is a reasonable starting point.
Airway Pressure Release Ventilation:
APRV is a form of continuous positive airway pressure (CPAP) that is characterized by a timed pressure release while allowing for spontaneous breathing. [16](See Figure 1) While previously considered a rescue strategy, APRV has recently gained acceptance as a primary ventilatory mode. Its indications for Acute Lung Injury (ALI)/Acute Respiratory distress syndrome (ARDS), multifocal pneumonia, and severe atelectasis make it a very attractive ventilatory option.
APRV functions by providing a continuous pressure to keep the lungs open with a timed-release to a lower set pressure.[17][18] The continuous pressure phase of APRV transmits pressure to the chest wall which allows for the recruitment of both proximal and distal alveoli. The prolonged continuous pressure phase with the short release phase avoids the continuous cycles of recruitment-derecruitment that occur in pressure/volume control vent settings.[19] This helps to avoid atelectrauma, barotrauma and resulting ventilator induced lung injury. [19](See Figure 2) The timed release allows for a passive exhalation and improved clearance of CO2. Since APRV relies upon spontaneous ventilation it requires less sedation compared to conventional modalities thus mitigating adverse events due to sedation. Spontaneous breathing has the benefit of increasing end-expiratory lung volume, decreasing atelectasis, and improves ventilation to dependent lung regions. [19] Spontaneous breathing, further, improves the hemodynamic profile by decreasing intrathoracic pressure, thus improving preload and cardiac output.
Setting up APRV requires the adjustment of four main variables, P-high, P-low, T-high, and T-low. [17][18] P-high is the continuous pressure that is set, while P-low is the pressure release part of the cycle. T-high is how long the continuous pressure is set to last, while T-low is the duration of the release phase. The patient should initially be set on AC/VC immediately post intubation until paralysis wears off. Then, an inspiratory hold should be performed to determine the plateau pressure. This plateau pressure becomes the P-high and should generally be around 27-29cm H2O, though obese patients may require a higher pressure. The P-low is generally set to 0, however, there is generally intrinsic PEEP as full exhalation does not occur. The T-high is generally set to 4-6 seconds, while the T-low to .2-.8 seconds in restrictive lung disease and .8-1.5 seconds in obstructive lung disease. To properly set the T-low, you should examine the Flow-Time Waveform on the ventilator. The T-low should be set to approximately 75% of the Peak Expiratory Flow Rate (PEFR).[19][17] (See Figure 3) The T-low needs to be continuously readjusted to 75% of the PEFR as lung recruits over time. FI02 should be titrated downwards once the patient is on APRV and comfortable.
Spontaneous breathing is paramount in APRV; thus, a small amount of pressure support or automatic tube compensation should be added to account for the endotracheal tube’s intrinsic resistance. [17] Hypoxemia can be corrected by increasing the P-high and T-high. [17] Hypoxemia can also be corrected by shortening the T-low. Permissive hypercapnia is allowed in APRV however hypercapnia can be corrected if needed by decreasing sedation, and/or by increasing P-high and T-high. It can further be corrected by increasing the T-low. Increasing the T-low can be problematic however as APRV relies upon intrinsic PEEP (iPEEP) to keep the lungs open during P-low. If the T-low increases, the iPEEP will decrease thus risking derecruitment of alveoli.
Other Issues
Before initiating mechanical ventilation one should also consider what medications to provide for post-intubation pain control and sedation. An "analgesia first" sedation strategy is recommended with the most commonly used agent being fentanyl due to its forgiving, i.e., minimally hypotension inducing hemodynamic properties.[20][21] If the patient is still agitated while getting an analgesia sedation regimen then additional agents, such as propofol can be added dependent on the patient's hemodynamics and clinical needs. A chest x-ray and a blood gas should be obtained to determine proper endotracheal placement and to assess minute ventilation. Many centers are now utilizing ultrasound to confirm endotracheal tube (ETT) placement; however, its use as not become standard of care. Plateau pressures should be checked frequently to assess alveolar integrity.
If the patient suddenly desaturates, then the DOPES mnemonic should be followed to determine the causes of the problem. DOPES stands for displacement, obstruction of the ETT or airways, pneumothorax/pulmonary embolism/pulmonary edema, equipment failure, and stacked breaths. The patient should immediately be disconnected from the ventilator and switched to a bag valve mask. The person bagging should ventilate calmly and allow for a full exhalation. Following this, a systematic approach should be followed. Does the patient still have a good waveform on their ETCO2? If not then the ET tube may have become dislodged. Does the patient bag easily or difficulty? If bagging is difficult, this will inform you of some sort of obstructive problems such as an obstructed ET tube, pneumothorax, or bronchospasm. If the patient bags easily and SpO2 rises rapidly then it points to equipment failure. While this is under evaluation, another provider should be assessing the patient with an ultrasound of the lungs and heart, and a chest X-ray should be obtained ASAP. Pulmonary embolism should be a consideration if no other cause of the desaturation is found.
Enhancing Healthcare Team Outcomes
The management for a patient on mechanical ventilation requires an interprofessional team involving physicians, nurses, and respiratory therapists. Good communication among the team is paramount. Respiratory therapists provide a crucial role in managing the ventilated patient, and their expertise should be utilized extensively. [22] Finally, only one dedicated professional should be in charge of the ventilator and vent changes should not be made without communication with others in charge of the patient. [Level III]
(Click Image to Enlarge)

Figure 1. APRV Pressure cycles with superimposed Spontaneous Breathing Airway pressure release ventilation is a form of continuous positive airway pressure (CPAP). The Phigh is equivalent to a CPAP level; Thigh is the duration of Phigh. The CPAP phase (Phigh) is intermittently released to a Plow for a brief duration (Tlow) reestablishing the CPAP level on the subsequent breath. Spontaneous breathing may be superimposed at both pressure levels and is independent of time-cycling.
Habashi NM. Other approaches to open-lung ventilation: Airway pressure release ventilation. Critical Care Medicine. 2005;33(Supplement).
(Click Image to Enlarge)
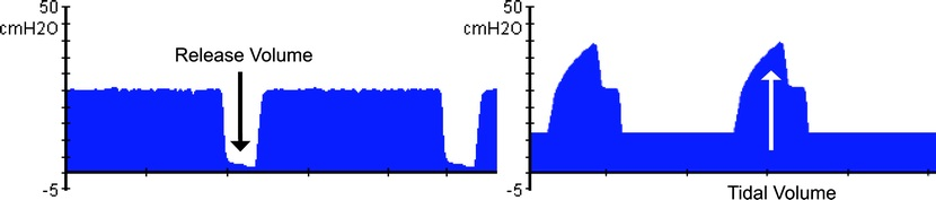
Figure 2. Tidal Volume during APRV vs Conventional Ventilation Ventilation during airway pressure release ventilation is augmented by release volumes and is associated with decreasing airway pressure and lung distension. Conversely, tidal volumes during conventional ventilation are generated by increasing airway pressure and lung distension.
Habashi NM. Other approaches to open-lung ventilation: Airway pressure release ventilation. Critical Care Medicine. 2005;33(Supplement).
(Click Image to Enlarge)

Figure 3: Depiction of a Peak Expiratory Flow Curve A patient with a lung that initially has low compliance has a steeper expiratory flow curve (30°) and will require a short release phase (TLow) (0.3 s in this example) to terminate the expiratory flow rate at 75% of the peak expiratory flow (PEFR). As the lung recruits and becomes more compliant, the slope decreases to 45°, requiring an extension in the TLow time, in this example to 0.5 s. With alveolar recruitment and increasing compliance, the lung is able to accommodate larger tidal volumes. Thus, airway pressure release ventilation allows for mechanical ventilation that is time controlled and adaptive to the patient's respiratory system mechanics (time-controlled adaptive ventilation).
Habashi NM. Other approaches to open-lung ventilation: Airway pressure release ventilation. Critical Care Medicine. 2005;33(Supplement).