Phakic Intraocular Lens Myopia
- Article Author:
- Sumaiya Hasan
- Article Editor:
- Koushik Tripathy
- Updated:
- 8/10/2020 10:52:41 PM
- For CME on this topic:
- Phakic Intraocular Lens Myopia CME
- PubMed Link:
- Phakic Intraocular Lens Myopia
Introduction
Myopia is a condition of nearsightedness in which parallel rays from infinity are focused before they reach the retina with the accommodation at rest. Various refractive surgical procedures are used to treat myopia namely laser in situ keratomileuses (LASIK), photorefractive keratectomy (PRK), laser-assisted subepithelial keratectomy (LASEK) or Epi-LASEK, intracorneal ring segments (ICRS or INTACS), clear lens extraction (CLE) or phakic intraocular lens/IOL (PIOL) implantation.
Excimer laser procedures are effective for the treatment of low and moderate myopia. Intracorneal ring segments may be used to treat low myopia, but their results are highly unpredictable. Highly ametropic eyes are not suitable candidates for laser procedures or ICRS and require options such as phakic IOL implantation. This provides for a better quality of vision not available with other techniques. The preservation of accommodation and minimal manipulation of the crystalline lens are other advantages.[1]
History of Phakic IOLs
In 1953, Benedetto Strampelli implanted an anterior chamber IOL (ACIOL) for the correction of severe myopia in phakic eyes. These did not come into practice due to endothelial complications, iritis, pupillary block, and glaucoma. Joaquin Barraquer introduced an IOL with elastic loops better adaptable to the anterior chamber for myopic phakic eyes. These IOLs also caused similar complications and thus did not become very popular.[2]
Over time phakic AC-IOLs progressively improved. Important contributions in the development of phakic IOL’s include the contribution by:
Fechner and Worst – iris fixed IOLs [3]
Baikoff – angle supported AC-IOLs [4]
Fyodorov - posterior chamber IOLs (PC-IOLs) with ciliary groove fixation [5]
Etiology
The normal process of emmetropization starts with hyperopia in the infancy of approximately +2 D. During the first two years of life, and there is a rapid decrease in this hyperopia to approximately +1 D. The shift towards emmetropia continues at a slower rate after three years until around six years of age.[6]
This is related to the rate of growth of the eyeball. In myopic individuals, the axial length increases at a much faster rate. Axial myopia is an increase in axial length and thinning of the sclera that is due to increased collagen degradation and reduced collagen synthesis.[7] Myopia may be categorized as mild myopia (0 D to −1.5 D), moderate myopia (−1.5 D to −6.0 D), and high myopia (−6.0 D or more).[8] Pathological myopia is usually seen with -8 D or more and is associated with typical retinal and macular degeneration.[8]
Various environmental factors play a role in the development of myopia, although no clear association has been established yet. Several day-to-day activities, such as decreased outdoor time and increased near work activities, including increased use of electronic devices, play a contributory role in the development of myopia.[9] Other proposed causes include genetic predisposition, low daily light exposure, and diet.[10]
Epidemiology
There is a huge variation in the prevalence of myopia in different regions and ethnic groups.[11] The prevalence of myopia can be estimated to be around 70% to 90% in Asia, around 30% to 40% in Europe and America, and 10% to 20% in Africa.[12]
High myopia contributes approximately 10 to 20% of the cases in young adults.[13] The major risk factors identified are intensive education and limited outdoor time.[13] Myopia progression in Asian children is faster than in Western children.[14] No gender predilection has been reported in the prevalence of myopia.
The morbidity caused due to vision impairment from uncorrected myopia along with irreversible visual loss from myopia-related complications warrants accurate global estimates of the situation and temporal trends critical for planning management.[9]
The percentage of moderate and high myopes opting for refractive surgery is approximately ten times and sixteen times more than low myopes, respectively.[15]
History and Physical
Preoperative history for implantation of a phakic IOL should begin with establishing realistic expectations for the procedure. A complete history of the refractive stability, comfort, and satisfaction with glasses or contact lenses, the age of first spectacle correction, any history of amblyopia or strabismus should be taken. Frequent change in the prescription of glasses needs to be evaluated in detail for conditions like keratoconus or pellucid marginal degeneration.
Patient’s Age: A young aged motivated patient who has achieved refractive stability and has less than 0.5 D of refractive change in 1 year is an ideal candidate for phakic IOL.[16] The concept of presbyopia needs to be clearly explained while counseling a patient for any kind of refractive surgery.[17]
Pupil Size: A scotopic pupil size larger than the optical zone of the implant would lead to glare and halos, which may be severely debilitating in the postoperative period and may even demand explantation of the IOL.[18]
A complete corneal evaluation with endothelial cell count and topography is important before planning a phakic IOL implantation.
A substantially deep anterior chamber is mandatory for a phakic IOL. Most phakic IOLs require an anterior chamber depth of at least 3 mm.[19]
Relative Contraindications for Phakic IOLs Include:[16]
- Cataract
- Chronic uveitis
- Low endothelial cell count
- Visually significant retinopathies
- Iris abnormalities
- Angle abnormalities
- Glaucoma
Indications for FDA (Food and Drug Administration, USA) Approved Phakic IOLs:[20]
Visian ICL: correction of myopia from -3.0 to -15.0 D and reduction of myopia from -15.0 to -20.0 D with less than 2.5 D of astigmatism at the spectacle plane in patients aged 21 to 45 years with an anterior chamber depth of more than 3.0 mm and refractive stability within 0.5 D for one year before implantation.
Artisan/ Verisyse IOL: Correction of myopia from -5.0 to -20.0 D with less than 2.5 D of astigmatism at the spectacle plane in patients aged more than 21 years with an anterior chamber depth of more than 3.2 mm and refractive stability within 0.5 D for six months before implantation.
Contraindications for FDA Approved Phakic IOLs:[20]
Visian ICL: Anterior chamber angle less than grade 2 determined by gonioscopy, pregnant or nursing females, endothelial density in the range 1900 to 3875 cells/mm^2 depending on age.
Artisan/Verisyse IOL: Any angle abnormality, iris abnormalities such as peaked pupil or elevated iris margin, pregnant or nursing females, endothelial density in the range 2000 to 3550 cells/mm^2 depending on age.
Evaluation
The following factors need to be considered in the preoperative evaluation:
Refraction: Both manifest and cycloplegic refraction should be performed. The best-corrected visual acuity in the undilated and cycloplegic state (after performing cycloplegia with homatropine or tropicamide) should be recorded.
Anterior chamber depth (ACD): Most phakic IOLs require ACD of at least 3 mm.
Anterior chamber angle and gonioscopy: Gonioscopy should be performed preoperatively to identify narrow or abnormal angles, which may lead to further postoperative narrowing and secondary glaucoma after phakic IOL implantation. The accepted range of iridocorneal angle aperture for phakic IOL implantation is more than or equal to 30 degrees, which corresponds to Shaffer grade 3 and 4 or Scheie grade 0 and 1.[21]
Corneal topography should be performed as is done in all refractive workups.
Specular microscopy: Including specular microscopic measurement of endothelial cell count, cell shape (polymorphism), and variation in cell size (polymegathism). Phakic IOL implantation leads to endothelial cell loss in the postoperative period, more so for the anterior chamber IOLs (ACIOLs) and so a healthy preoperative endothelium with a cell count of at least 2300 per millimeter square should be ensured.[16][22]
Sulcus to sulcus (STS) measurements: This is essential for sizing of the phakic IOL and measurement of lens vault (distance between the posterior surface of the IOL and the anterior lens capsule) in case of a phakic posterior chamber IOL (PCIOL). An approximate calculation of the size of the IOL depending on the vault is made using the white to white (WTW) measurement by adding 0.5 mm to the measured value in myopes and subtracting 0.5 mm in hyperopes. WTW may be measured using calipers, scanning slit topography, digital caliper, Scheimpflug-based devices, ultrasound biomicroscopy (UBM), or digital ultrasounds.[23][24][25] As the measurement values may vary depending on the method used, it is prudent to use an average of the values. It has been suggested that directly measuring the STS diameter using ultrasound biomicroscopy or very high frequency (VHF) digital ultrasound may be a more reliable method for the size estimation of phakic IOLs.[26][27]
Ideal vault size for phakic posterior chamber IOLs is 1 plus or minus 0.5 of the corneal thickness, which is in the range of 250 to 750 microns.[28]
IOL power calculation: Biometry, keratometry, anterior chamber depth (ACD), lens thickness, preoperative refraction need to be accurately measured, and the appropriate formula applied. Van der Hejde nomogram may be used for IOL power calculation.[29]
Peripheral retinal examination and laser of retinal breaks are important to prevent complications of retinal detachments in the postoperative period, especially as pupil dilation remains limited with anterior chamber IOLs.
Treatment / Management
Treatment of high myopia can be done using spectacles, contact lenses, keratorefractive procedures, CLE, and phakic IOLs Spectacles may induce aberrations in cases of high myopia, and the patient may thus be intolerant to their use. Contact lens use is cumbersome, and they need to be changed and cleaned periodically, making them unsuitable for many candidates. Keratorefractive procedures alter the normal asphericity and shape of the cornea and may lead to various complications in the postoperative period, such as haze (PRK) or flap related complications and ectasia (LASIK). Moreover, the patient needs to fit into the corneal topography and thickness criteria to be able to undergo these procedures. CLE leads to a loss of accommodation and thus is unsuitable for young aged patients.[30][31] Also, CLE in high myopia may be associated with an increased risk of retinal detachment.[32]
Preoperative laser iridotomy or intraoperative surgical iridectomy needs to be performed to avoid pupillary block in the postoperative period for the anterior chamber IOLs, and the posterior chamber PRL and Visian ICL 4 models.[33]
Prognosis
Success with the lens depends largely on accurate preoperative evaluation, which determines the vaulting in case of a PCIOL and sizing in case of an ACIOL.[34] Newer models of IOLs have incorporated features to minimize contact with iris and conform better to the geometry of the eye.[35]
Refractive outcomes are good, and with optimum calculations, these IOLs can effectively correct myopia of up to 20 dioptres (D) with good results.
Studies have shown PIOLs to have good postoperative visual outcomes such as a mean postoperative uncorrected visual acuity (UCVA) of better than 20/40 in the majority of patients.[36][37]
Complications
Endothelial cell loss: It is more common with ACIOLs. This may lead to corneal decompensation, and in extreme cases, explantation of the IOL may be required when the endothelial count drops below 2000 cells per millimeter square. A 1% mean annual reduction in endothelial cell count has been seen in angle fixed IOLs when the distance between the corneal endothelium and the edge of the IOL is 1.43 mm.[38] This increases to 1.7% when the distance reduces to 1.2 mm and is minimal when the distance is 1.66 mm.[38]
In a study on the implantation of anterior chamber phakic IOLs, the NuVita IOL reported 2.35% endothelial cell loss at one year and was thus withdrawn.[39] Average endothelial cell loss at one year, as seen in different studies on other models, was 3.86% in ZSAL-4,[40] 1.83% in iris fixated IOL's,[41] 2% in IPCL[42], 0.9% in ICL.[43]
In a 12 year retrospective study on 144 eyes implanted with ICL, Moya et al. reported 6.46% surgically induced endothelial cell loss during the first year, beyond which an average yearly decrease rate of 1.20% was noted.[44]
IOL rotation happens due to inappropriate sizing. May lead to induced astigmatism in cases of toric IOLs.
Pigment dispersion may lead to lens deposits. Usually, no intervention is required.
Chronic inflammation and uveitis are more common with ACIOLs.
Pupil distortion is seen in ACIOLs. This may lead to intractable glare and maybe cosmetically unacceptable.
Pupillary block and glaucoma: Pupillary block may occur due to inappropriate vaulting in the case of PCIOLs. It may resolve after pupil dilation and use of pressure-lowering agents, but the definitive treatment is the creation or enhancement of a previously created peripheral iridotomy. Retained viscoelastic material may also cause raised intraocular pressure (IOP). Angle fixed IOLs may block the angles and lead to a rise in IOP.
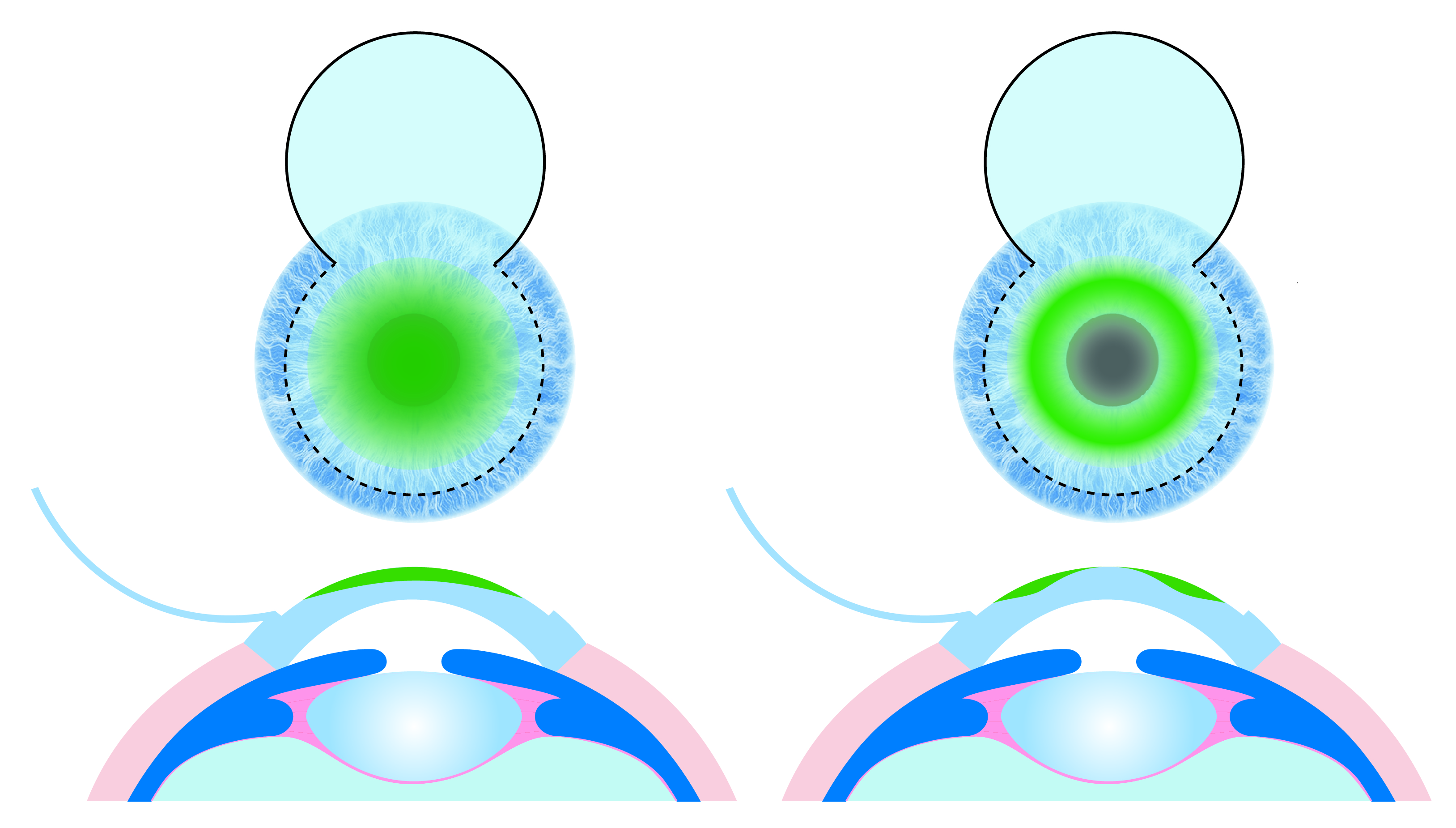
Glare and halos are seen when the scotopic pupil size is greater than the optic of the IOL. Miotic agents may be given for resolution.
Cataract formation occurs in low PIOL vault or undersized PCIOL. This is mostly in the form of anterior subcapsular opacities that develop due to the pressure of the IOL on the crystalline lens. Lens material also plays a role. Silicone in PRL may predispose more to cataract formation than Collamer of ICL.[45][46][47]
In a 5-year retrospective study, Brar et al. reported that, in a total of 957 eyes, significant anterior subcapsular cataract (ASC) requiring explantation developed in four eyes (0.4%).[48] In an eight-year follow up of 41 eyes implanted with V4 ICL by Igarashi et al., asymptomatic ASC was reported in four eyes (9.8%).[49] Sanders et al., in their study on 106 eyes with -12.00 D or more of preoperative myopia reported clinically significant cataracts in seven eyes (6.6%), whereas no cataract occurred in 420 eyes with preoperative myopia less than -12.00 D. They thus concluded that a higher degree of baseline myopia more frequently predisposes to cataract formation.[50]
As most cases are high myopes, there are chances of rhegmatogenous retinal detachments (RRD) more than emmetropic eyes, in the range of 0.7% to 3.2%.[51] However, such eyes with high myopia are already predisposed to retinal detachment, and the association of PIOL with RRD needs further evaluation.
Deterrence and Patient Education
Patients need to be aptly counseled preoperatively with complete knowledge of all available options and realistic expectations set for postoperative outcomes along with necessary information on the possible complications.
Pearls and Other Issues
Any residual refractive error may be corrected using bioptics, which is the combination of an intraocular procedure with a keratorefractive procedure. Pseudophakic ametropia may also be corrected with the help of phakic IOLs.[52]
Enhancing Healthcare Team Outcomes
A high myopia-patient may commonly present to a primary healthcare provider, so the patient must be counseled appropriately about the various treatment options available. The patient should be evaluated completely by an optometrist and efficiently worked up by an ophthalmic technician as the success of the procedure largely depends on the preoperative measurements.
Proper consideration needs to be given to any medical condition the patient may be having and should receive treatment for the same. The nurses are also vital members of the interprofessional group as they monitor the patient's vital signs and assist with the education of the patient and family as well as compliance on follow up. Pharmacists can ensure appropriate postoperative dosing of medication. This collaborative, interprofessional approach to care can ensure optimal patient outcomes.
(Click Image to Enlarge)