Supraorbital Nerve Block
- Article Author:
- Andrew Napier
- Article Author:
- Orlando De Jesus
- Article Editor:
- Alan Taylor
- Updated:
- 7/31/2020 2:26:50 PM
- For CME on this topic:
- Supraorbital Nerve Block CME
- PubMed Link:
- Supraorbital Nerve Block
Introduction
The supraorbital nerve block is a procedure performed to provide immediate localized anesthesia for a multitude of injuries such as complex lacerations to the forehead, upper eyelid laceration repair, debridement of abrasions or burns to the forehead, removal of foreign bodies, or pain relief from acute herpes zoster. A regional block allows for minimal anesthetic use, which permits the operator to obtain the intended anesthesia over a larger surface area versus that of local infiltration. The smaller anesthetic volume used also allows for minimal dissemination of anesthetic into tissues, which will prevent the distortion of normal anatomy during the intended procedure.[1] This procedure requires knowledge of appropriate anatomical landmarks and minimal equipment.
Anatomy and Physiology
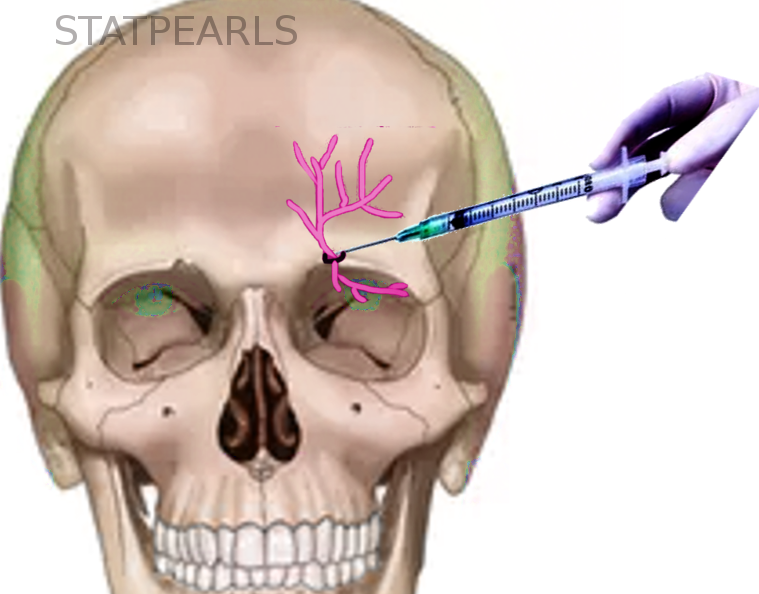
The recognition of the appropriate anatomy for this procedure is critical, as it is landmark-based. The supraorbital nerve is one of the terminal branches of the trigeminal nerve. The trigeminal nerve divides into three branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3).[2] The supraorbital nerve is a branch of the ophthalmic nerve. This sensory nerve branches into two separate terminal branches, known as the smaller supratrochlear nerve and the larger supraorbital nerve. The supraorbital nerve exits the cranium through an opening above the orbit known as the supraorbital notch or supraorbital foramen which lies within the medial one-third of the supraorbital margin, 2 to 3 cm lateral to the midline. The nerve then ascends the forehead and terminates at the region of the anterior scalp, thus providing sensory input for tissues up to the region of the lambdoidal suture (connection of the parietal and occipital bones). The supratrochlear nerve provides sensory information in a small area which is close to the midline. The supraorbital foramen can be visually identified by having the patient look straight ahead and then transect the pupil at the level of the patient’s orbital ridge. Palpation of this region reveals the area of interest for performing this nerve block.[3][4][5] A majority of supraorbital nerve exits existed as notches (73.8%) and the rest as foramina (26.2%).[6] Accessory exits were seen in 18.9% skulls. Of the skulls examined, 55.1% displayed bilateral supraorbital notches, 8.6% had bilateral supraorbital foramina, and 36.3% had a notch on one side and a foramen on the contralateral side.[6]
Beyond the orbital rim, the supraorbital nerve has two consistently present divisions: (1) a superficial (medial) division that passes over the frontalis muscle, providing sensory supply to the forehead skin and only to the anterior margin of the scalp; and (2) a deep (lateral) division that runs cephalad across the lateral forehead between the galea aponeurotica and the pericranium as the sensory nerve to the frontoparietal scalp.[7]
Patients with supraorbital neuralgia present with pain, tenderness, hypoesthesia, and allodynia in the territory supplied by the affected nerve. Fractures of the orbital roof, blunt trauma to the face, tumors of the orbit, and tight swimming goggles and motorcycle helmet can cause supraorbital nerve entrapment.
Indications
Indications for supraorbital nerve block encompass procedures of the forehead near the ipsilateral side of injection and at the anterior aspect of the scalp which may include:
- Debridement of burns or abrasions[8]
- Immediate relief of acute pain from herpes zoster[9]
- Postherpetic itch[10]
- Repair of complex lacerations[8]
- Removal of foreign bodies[8]
- Migraine (episodic and chronic)[11][12][13]
- Neuralgia (supratrochlear or supraorbital)[12][14][15]
- Trigeminal neuralgia[5][16]
- Cluster headache[12]
- Trabeculectomy surgery[17]
- Upper eyelid surgery[4]
- Oculoplastic surgery[18]
- Awake craniotomy[19][20]
- Cranial fixation and stereotactic frames placement[21]
- Hemicrania continua [22]
- Dermatologic/oncologic procedures[23]
Contraindications
Contraindications to the supraorbital nerve block include:
- Refusal of the patient
- Distortion of anatomical landmarks
- Overlying infection at the site of injection
- Allergy to local anesthetics
Equipment
Required equipment for the supraorbital nerve block include:
- Anesthetic agent: the choice of an anesthetic agent depends on the patient’s reported allergies and the intended duration of the nerve block. Lidocaine for up to 90-minutes of local anesthesia, bupivacaine for up to 8 hours of local anesthesia, and tetracaine for up to 3 hours of local anesthesia.
- Consider local diphenhydramine if the patient is allergic to both amides and esters local anesthetics.
- 25 ga needle for adults, 30 ga needle for pediatrics
- 5-10 mL syringe
- Skin cleansing agent such as chlorhexidine or betadine
- Access to lipid emulsion solution in case of local anesthetic systemic toxicity
- Ultrasound if desired for guided injection
Preparation
Prior to starting the procedure, one should educate the patient regarding the risks and benefits of the supraorbital nerve block and then obtain informed consent from the patient. One should then bring all necessary equipment to the bedside and prepare the materials for the procedure.
When lidocaine is combined with epinephrine, the maximum amount that the patient can be given 7 mg/kg per dose. The total dosage of lidocaine with epinephrine given should not exceed 500 mg total. When lidocaine is given without epinephrine the patient can be given 4.5 mg/kg per dose, not to exceed 300 mg total.
When bupivacaine is combined with epinephrine, the maximum amount that the patient can be given is 3 mg/kg per dose. The total dosage of bupivacaine with epinephrine given should not exceed 225 mg per dose with a maximum dose of 400 mg/24h. When bupivacaine is given without epinephrine the maximum amount that the patient can be given is 2.5 mg/kg per dose, not to exceed 175 mg per dose with a maximum of 400 mg/24h.
Technique
The supraorbital nerve block procedure utilizes the following steps:
- Identify appropriate landmarks
- Using aseptic technique clean the injection area using a skin cleansing agent
- Place the patient in a supine position
- From a position lateral to the patient’s head, insert a 25-30-gauge needle in a medial and cephalad direction into the inferior edge of the supraorbital ridge approximately 0.5 cm below the supraorbital notch
- Advance the needle slightly being careful not to penetrate the supraorbital foramen
- Perform a test aspirate
- Inject 0.5-1 mL of local anesthetic solution to form a subcutaneous wheal and then continue to inject 1-3 mL of local anesthetic
- Firmly place a small roll of gauze above the orbital rim to prevent ballooning of anesthetic at the superior aspect of the eyelid
Due to the various branching of the ophthalmic nerve, the nerve block may not be successful after the first attempt. Injection of additional local anesthetic medial and laterally along the orbital rim will adequately reach all nerve branches.[4]
Complications
Complications of the supraorbital nerve block may include:
- Formation of hematoma or eyelid swelling
- Delayed periorbital ecchymosis
- Infection
- Bleeding
- Vascular injection of anesthetic
- Nerve injury including neurapraxia or neurolysis
- Local anesthetic systemic toxicity
- Allergic reaction to the local anesthetic
Clinical Significance
There are numerous ways in which to provide anesthesia to patients that are in pain so that they may obtain relief. Aside from the management of pain, this anesthesia will also allow the clinician to perform procedures effectively and prevent further discomfort to the patient. A method of providing this anesthesia resides in the form of targeting tissues or a peripheral nerve itself, both of which propagate signals of pain from tissues to the brain and brainstem.
Adequate anesthesia may be accomplished by the local infiltration of an anesthetic directly into a tissue, or in a targeted manner such as a nerve block. Local infiltration of an anesthetic agent allows for the repair of simple injuries to a given anatomic location, but its use is limited in those who have suffered injuries to a larger surface area or have multiple separated injuries. Additionally, local infiltration of a wound may distort the area of repair. In such cases, a nerve block is an option to provide a larger region of anesthesia with a smaller relative amount of anesthetic.[24]
Enhancing Healthcare Team Outcomes
The supraorbital nerve block is a procedure best performed with a group of professionals in the healthcare team, which includes a physician or midlevel provider, nursing staff, and a pharmacist. The staff must elicit a full history and physical exam including a history of adverse drug reactions, in particular, prior history of local anesthetic use to identify alternatives if needed. Approaching this procedure in a team-based manner will help to limit adverse events. The interprofessional team paradigm is optimally suited to manage these cases, leading to better outcomes via coordination and communication between clinicians, nursing, pharmacists, and other ancillary personnel. [Level 5]
The following list should be assessed and adequate provisions identified before the start of the procedure:
- Assessment of any adverse events that the patient may have had to local anesthetics
- Calculation of maximum weight-based dosage of chosen local anesthetic
- Consultation with a pharmacist about the availability of a lipid emulsifying agent in the event of local anesthetic systemic toxicity
- Patient monitoring for signs and symptoms of local anesthetic systemic toxicity such as the perception of a metallic taste, altered mental status, respiratory distress, seizures, tachycardia, dysrhythmia, atrioventricular block, or cardiovascular collapse.[25] [Level 3]
- Availability of staff trained in advanced cardiac life support in the event of cardiovascular symptoms or emergency.