Neuroma
- Article Author:
- Mate Zabaglo
- Article Editor:
- Mark Dreyer
- Updated:
- 8/10/2020 4:43:44 PM
- For CME on this topic:
- Neuroma CME
- PubMed Link:
- Neuroma
Introduction
Neuromas are benign tumors of the nervous system most commonly arising from non-neural nervous tissue, although they are not considered neoplasms. Certain neuromas have a particular location and symptoms, while others can develop anywhere in the body. The term neuroma is often used for post-traumatic swelling of nerves as well. They develop as an injured nerve starts to heal in an uncontrolled manner resulting in a lump of unorganized axon fibers and non-neural tissue growth. Neuromas often arise post-trauma, including elective surgery. They can be part of a syndrome such as neurofibromatosis, or they can be a true neoplasm such as acoustic neuroma or Morton neuroma.
Diagnosis is mainly clinical, and treatment is most often surgical excision with a strong emphasis on prevention, meaning surgical exploration and repair of nerve injuries.
Etiology
Neuromas can divide into true neoplasms, traumatic neuromas, and neuromas as part of a syndrome.
True neoplasms include neural fibrolipoma, acoustic neuroma, ganglioneuroma, neurothekeoma, nerve sheath myxoma. Neural fibrolipoma is a sausage-shaped localized expansion of epineurial adipose and fibrous tissue of a segment of a major nerve. Acoustic neuroma or vestibular schwannoma is an intracranial tumor presenting with tinnitus hearing loss and vertigo. Ganglionneuroma is a sympathetic autonomic nervous tumor commonly arising in the abdomen, which can produce hormones. Neurothekeoma and nerve sheath myxoma are both perineural tumors.
Traumatic neuromas can develop after blunt or sharp trauma or traction injury. Mortons neuroma(localized interdigital neuroma) is a traumatic neuroma of the third metatarsal interspace. A Pacinian neuroma is a unique tumor consists entirely or partly of Pacinian corpuscles, which are dermal tactile receptors. Elective surgery is also a significant cause of traumatic neuromas. It is common to see neuroma formation following elective hand surgery, especially the superficial radial nerve is susceptible, or after knee arthroplasty, the saphenous nerve is vulnerable.[1]
Neuromas can develop after amputation called stump neuroma. The symptoms they produce should not be confused with phantom limb pain.
Neuromas can be part of a syndrome such as neurofibromatosis or MEN2B. Neurofibroma (or neurofibromatosis) is a genetic condition in which multiple neuromas form in various places of the central and peripheral nervous system. They can present as skin lesions, can cause hearing and balance issues or pain. There is no known cure; surgery has a role in symptom control. Multiple endocrine neoplasia 2B (MEN2B) is a genetic syndrome consisting of medullary thyroid carcinoma, pheochromocytoma, and mucosal neuromas.
Epidemiology
While the incidence of neuromas varies in the literature, one must consider that most neuromas are asymptomatic, and therefore go undetected. One study looking at hand injuries found incidence at 1% after nerve repair and at 7.8% after finger amputation,[2] and another study for hand injuries found incidence at 6.6% after finger amputation.[3]
Pathophysiology
An essential step in neuroma formation is widely accepted to be the injury of the perineurium as, without an intact perineurium, the axon fibers cannot go through. As soon as perineurium is damaged, the axons will escape. Another critical step is thought to be neuroinflammation.[4] As the axons get to the extraperineurial space where there is already tissue damage, there will be inflammation. The compounds released during inflammation can aid neuroma formation.
The injured nerve endings start to regenerate in an unregulated fashion disrupting the mostly linear organization of fibers resulting in an unorganized growth. This growth will create and transmit signals which the central nervous system can interpret as pain.
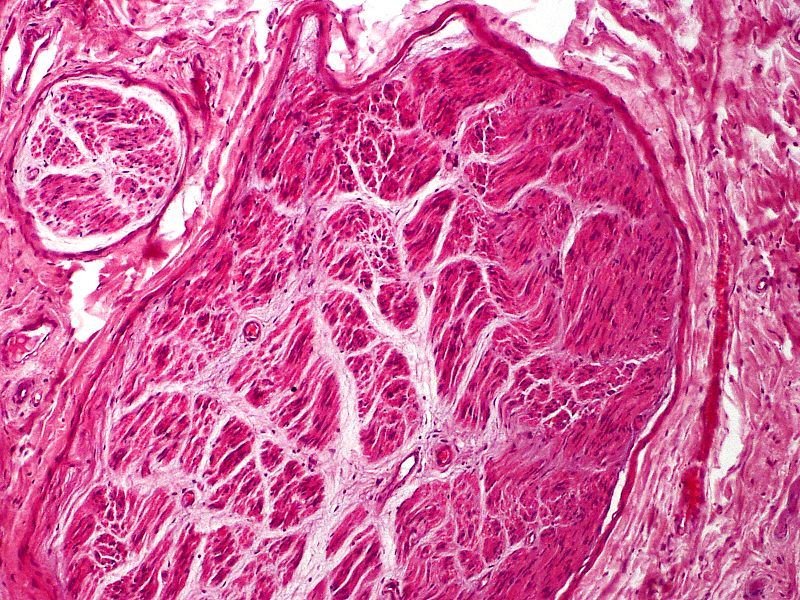
Histopathology
Myofibroblasts are frequently part of the scar either scattered through or in aggregates mainly present in the 2 to 6 months post-injury. After this time, as more collagen is laid down, their number diminishes.[5]
With standard HE stains, one can observe the irregular axon fascicles surrounded by prominent perineurium in various stages of maturation. Depending on when the sample gets taken, perineurium can also still be damaged. Especially close to the cut nerve endings, Schwann cells and myofibroblasts can be present within the scar tissue. There is also a relatively high content of glycosaminoglycans.
There is a very rare subtype of neuroma called Pacinian corpuscle neuroma. Pacinian corpuscles are mechanoreceptors in various organs, including the skin. This post-traumatic neuroma can form after skin injuries, frequently in fingers. It can be easily identified under the microscope as the corpuscles are larger in size and number than usual.
History and Physical
History should reveal a trauma of the affected region in the not too distant past. Special care should be taken to establish where and how was the injury treated, was there any attempt at repairing the nerve.
If there is no history of trauma, the differential should shift towards genetic causes of the neuroma and true neoplasms.
Neuroma pain can be burning, sharp, tingling sensation, or numbness.
On examination, a well defined hard lump is usually palpable, which can be adherent to nearby structures. On pressure, patients can experience a sensation similar to electric shock.
Evaluation
The diagnosis of neuroma is mainly dependent on history and examination. In cases where there is uncertainty, X-rays can be taken to rule out bone injury as a cause of pain and to rule out bone malignancy. Ultrasound, computed tomogram (CT) and magnetic resonance imaging (MRI) will show well-defined soft tissue mass but are rarely necessary investigations.
There are no laboratory tests that would aid diagnosis. After surgical excision, it is common practice to send lesions for histopathology examination to rule out malignancy.
Treatment / Management
There is no consensus on how to best treat an already formed neuroma.[6] Prevention is essential as this condition affects the quality of life. Following injuries or during elective operations after transection of a nerve is transected, the surgeon should reconnect the two nerve endings where possible. Following injuries where the nerve damage is suspected, patients must seek medical attention in centers where usually plastic surgeons can diagnose, explore, and treat nerve damage. Many different surgical strategies exist to prevent neuroma formation after trauma, none of which are superior to each other. Neurorraphy significantly reduces neuroma formation to 1% from 7.8% untreated or amputated.[2] Generally accepted principal surgical aims are: repair should not be under tension, in a theatre environment with loupe or microscope magnification, align nerve so that same axon can reconnect. Careful and minimal debridement is also accepted. If there is a gap, it is common to sacrifice a less crucial sensory nerve to provide a nerve graft for the repair, which can be multi-stranded. If the two ends cannot be rejoined (amputation), it is common to bury the nerve or suture it onto muscle to help prevent neuroma formation; this is called targeted muscle reinnervation.
For an already formed neuroma, there is also a range of treatments. There are simple methods such as ice packs, elevation, and rest to reduce swelling. A variety of pharmacological therapies would include non-steroidal anti-inflammatory drugs (NSAIDs), local anesthetic creams or injections, or intralesional steroid injections. Unfortunately, often, the pain is resistant to most pharmacological analgetic methods.
The neuroma can be injected with phenol or dehydrated alcohol under ultrasound guidance sclerosing the lesion.[7] A surgical excision is an option, but recurrence rates are high, with a considerable variation in literature ranging from 15% to 50%.[8][9] Often, neuromas still get surgical management as other modalities are often ineffective.
Differential Diagnosis
History and examination are often enough to differentiate between neuroma and other conditions, also to distinguish between the types of a neuroma. Where there is doubt, an X-ray can help to differentiate from fracture and establishing a possible connection to bone. Ultrasound, CT, or MRI scans can help distinguish from malignant conditions, although seldom used.
Post excision histopathology examinations are usually undertaken for similar reasons and provide a higher level of ability to identify the nature of the lesion.
Pertinent Studies and Ongoing Trials
The current focus is on prevention, and various studies are looking at how we could reduce post-traumatic neuroma formation during surgical repair.
The CoNNECT randomized trial still in progress is looking at end to end, end to end plus conduit, and no direct suture only conduit secured repairs to determine if tubes are beneficial and if sutureless solutions merit consideration.
A study is looking at a substance that actively decreased neuroma formation when continuously released to repair site.[10]
A group of Chinese scientists is looking into autologous vein grafts to be used instead of nerve grafts to bridge short gaps after nerve injury.[11]
There is also work being done to use stem cells to help nerves regenerate after an injury. Although the main aim is to improve function rather than to reduce neuroma formation.[12]
Treatment Planning
In regards to prevention, it is clear that connecting the two nerve endings will provide the best outcome, so patients with nerve symptoms should go on a theatre list where there is an operating microscope, also loupe magnification available. Often these are extremity injuries, and patients would benefit from having an anesthetist on the list who can perform regional blocks.
The evidence does not provide clear guidance yet when it comes to operating on formed neuromas but seems to point towards excision and transposition or neurolysis and coverage as the most effective method of pain relief.[13]
Prognosis
After digital amputation, 6% of people will develop a neuroma.[3] When operated at the time of injury, this can decrease to 1%.
Neuromas are a benign condition and would be extremely rare to spread or metastasize. It can, however, increase in size, become more painful, become tethered.
There are no studies that are looking at traumatic neuroma regression. However, there are multiple which are looking at acoustic neuroma regression rates, which appear around the 4% mark.[14] This action results in some patients having active observation rather than surgery.
Complications
A neuroma is a painful condition with no other significant symptom or complication. This pain, however, is often so severe that patients have to undergo surgery.
Complications of surgery are a non-specific infection, bleeding, scarring, anesthetic risks. Unfortunately, recurrence rates are high.
Postoperative and Rehabilitation Care
Dressings are necessary for the wound healing period. Nerve repair occurs without tension; there is usually no need to protect the repair with a rigid brace or plaster, only bulky dressing.
Deterrence and Patient Education
Patients need to understand that any injury to any nerve can cause neuroma formation, and their best chance to avoid is to undergo surgery. Also, recurrence rates should be part of the discussion.
Enhancing Healthcare Team Outcomes
Neuroma prevention and treatment are mostly dependent on the surgeon. Still, during the patient journey, many healthcare professionals are encountered, and they must know about the prevention and treatment of neuromas to signpost, appropriately manage, and refer patients, and must function as an interprofessional team. Surgical teams have to be vigilant about intraoperative nerve damage and adequately repair as non-repaired injuries have a high risk of neuroma formation.
If a patient sustains an injury in the community and attends a minor injuries unit or an emergency department, it is vital that triaging and treating staff do not overlook checking for sensation and motor function. If nerve damage is suspected, it is essential to refer the patient to the appropriate specialist team.
While surgery is the primary form of treatment, patients can try various conservative pain-relieving pharmacological and non-pharmacological options. If they work, the patient does not have to have surgery. For pharmacological options, a pharmacist should participate in optimizing pain control and helping prevent opioid dependence. Nursing staff will prove invaluable in all phases of management regardless of whether it is surgical or conservative and can serve as a gatekeeper to the clinician for patient concerns, as well as their monitoring duties. Using this interprofessional approach will drive optimal patient outcomes. [Level V]
(Click Image to Enlarge)
(Click Image to Enlarge)