Neuroanatomy, Optic Chiasm
- Article Author:
- Ashley Ireland
- Article Editor:
- Iverson Carter
- Updated:
- 7/31/2020 2:56:51 PM
- For CME on this topic:
- Neuroanatomy, Optic Chiasm CME
- PubMed Link:
- Neuroanatomy, Optic Chiasm
Introduction
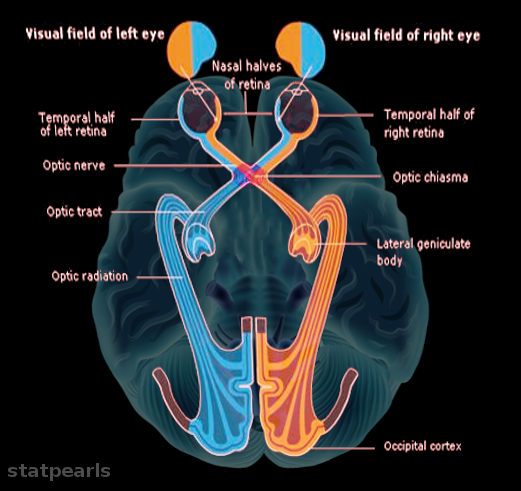
The visual pathway consists of all the anatomical elements essential in processing visual information. The pathway begins at the retina, which takes gross visual impulses to the brain through the optic nerve (cranial nerve II), to the optic chiasm, optic tract, lateral geniculate bodies, and finally, the visual cortex of the brain for interpretation.[1] The optic chiasm represents a fundamental and evolutionary aspect of the visual pathway – an adaptation to assist humans with binocular vision and stereopsis, otherwise known as depth perception.[2]
Structure and Function
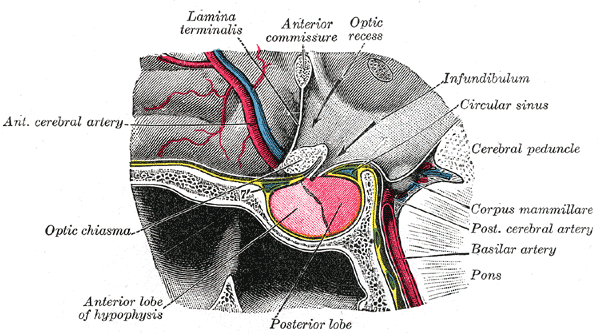
The average optic chiasm is about 3.5 mm in height and 15 mm in width.[3] It is found directly inferior to the hypothalamus, making it susceptible to disturbance secondary to hypothalamic disorders. It is located relatively superior to the sella turcica, and therefore the pituitary gland, which it contains, making it susceptible to secondary pituitary disorders.[4]
The optic nerve is one of 12 cranial nerves and is comprised of the axons of retinal ganglion cells (RGCs), originating in the outer retina. The RGC axons add up to about 1 to 1.5 million nerve fibers for the average human adult but decrease gradually with age.[5] From there, its path divides into four portions: the intraocular portion (subdivided into the prelaminar, laminar, and post-laminar portions), the intraorbital portion, the intra-canalicular portion, and the intracranial portion.[6] Between the intraocular and intraorbital portions, the RGC fibers pass through the optic canal - a small fissure within the lesser wing of the sphenoid bone.[7] The beginning of the optic tract is the termination of the intracranial portion of the optic nerve. The RGC fibers decussate within the chiasm in a ratio of crossed to uncrossed fibers of 53:47.[8] Beyond the optic chiasm, the RGC fibers have the name of the optic tract, which will eventually synapse in one of the six layers of the lateral geniculate nucleus, located in the thalamus. The path continues, and optic fibers leaving the LGN, known as optic radiations, end their journey in the striate visual cortex.
The optic chiasm contributes to stereopsis and binocular vision by processing visual information from one side of the visual field in the contralateral visual cortex. Visual information from the left visual field projects onto the nasal retina of the left eye and the temporal retina of the right eye. Information from the right visual field likewise projects onto the temporal retina of the left eye and the nasal retina of the right eye. Since the nasal fibers from both eyes decussate at the optic chiasm, the information from the right visual field, projected onto the nasal retina of the right eye, meets with the right visual field information that projected onto the temporal retina of the left eye. Therefore all of the right visual field information leaves the optic chiasm as the left optic tract. This concept applies vice versa to the left visual field information.[9]
Embryology
At approximately seven weeks gestation, crossed nerve fibers first appear and form the optic chiasm. Uncrossed nerve fibers of the chiasm do not develop until about 11 weeks gestation.
Myelination of retinal ganglion cells proceeds in a central-to-peripheral manner. Myelination begins at five months gestation in the LGN, proceeding to the optic tract at six months, optic chiasm at 6 to 7 months, and the optic nerve at eight months.
The optic stalk appears at 28 days gestation. At approximately seven weeks gestation, ganglionic axons invade and grow down the stalk to convert it into the embryonic optic nerve. It is not until the axons reach about 20 or 21 mm that they form the optic chiasm.[10]
Blood Supply and Lymphatics
The circle of Willis, otherwise known as the cerebral arterial circle, encircles the optic chiasm. It is composed of anastomoses of blood vessels that communicate the anterior and posterior blood supply of the brain. The following components comprise the circle of Willis:
- The left and right anterior cerebral arteries, connected through the anterior communicating artery.
- The left and right internal carotid arteries
- The left and right posterior cerebral arteries
- The left and right posterior communicating arteries, which connect the left and right internal carotid arteries to the left and right posterior cerebral arteries, respectively
The left and right anterior cerebral arteries, in addition to a branch of the internal carotid artery known as the superior hypophyseal artery, provide the blood supply to the optic chiasm.[11]
Surgical Considerations
The optic chiasm is a very important landmark during anterior circulation aneurysm and transsphenoidal surgeries.
Clinical Significance
The fibers from the nasal retina in each eye view visual stimuli from the temporal visual field. These are the fibers that decussate in the optic chiasm, and if the optic chiasm becomes compromised (severed, compressed, or ischemic), the result is vision loss in the temporal field of each eye. This condition is referred to as heteronymous bitemporal hemianopsia.[12]
Another significant clinical correlation is a pituitary adenoma, which is a malignant tumor of the hypophyseal (pituitary) gland. The gland is located in the pituitary fossa, approximately 10 mm inferior to the optic chiasm. Particularly a problem with macroadenomas (greater than 10 mm in size), these tumors compress the optic chiasm, causing the patient to experience bitemporal hemianopsia. These tumors can cause an increase or decrease in pituitary hormones, but most commonly result in a decrease in plasma testosterone, and may result in hypogonadism or gynecomastia in males.[13]
Tumors resulting in the compression of the blood supply to the optic chiasm may also result in a bitemporal hemianopsia visual field defect.
Generally, lesions that result in bi-temporal hemianopsia are not significant enough to disturb normal visual function, such as driving a car. In most cases, 110 to 120 degrees of the central visual field is retained.[12] Standard automated perimetry (SAP) can be used to detect visual field defects that result from lesions in the optic chiasm. Research has found SAP to be more accurate in earlier detection of lesions than Goldmann visual field testing.[14]
Research studies have found that a clinically significant decrease in optic chiasmal width can correlate with optic nerve atrophy, and in some cases, subsequent visual impairment.[14]
In patients with ocular albinism, there are many significant associated symptoms, including searching nystagmus, ill-developed macula, and strabismus. The strabismic adverse effect is not amenable to therapy due to an inappropriate, irreparable crossing of fibers in the optic chiasm; this is known as inappropriate axonal rerouting. In this case, fibers that are supposed to radiate ipsilaterally to the brain, cross instead to the contralateral cortex. These patients often have normal skin and hair color, but with decreased pigmentation of the iris, as well as a blonde fundus with visible choroidal vasculature. This condition may result in a permanent loss of visual acuity.[15]
Glial cells are important mediators of homeostasis within the central nervous system and include cells such as oligodendrocytes, which provide myelination of nerve fibers, as well as many other crucial non-neuronal cells. Gliomas are tumors originating in the glial cells of the central nervous system. Gliomas can occur in the optic nerve and optic chiasm. While they comprise a vast majority of malignant brain tumors occurring in humans, optic gliomas are typically benign. Patients can undergo sporadic vision loss and recovery, as well as proptosis, and involuntary eye movements. While optic nerve gliomas can spontaneously regress, it is unlikely. Treatment options include surgery (rarely), chemotherapy, corticosteroids, and radiation. Optic nerve gliomas are associated (30%) with a condition known as neurofibromatosis type 1. Additionally, they can occur jointly with hypothalamic tumors.[16]
(Click Image to Enlarge)