
Anatomy, Head and Neck, Eye Orbicularis Oculi Muscle
- Article Author:
- John Tong
- Article Author:
- Michael Lopez
- Article Editor:
- Bhupendra Patel
- Updated:
- 7/27/2020 12:46:18 PM
- For CME on this topic:
- Anatomy, Head and Neck, Eye Orbicularis Oculi Muscle CME
- PubMed Link:
- Anatomy, Head and Neck, Eye Orbicularis Oculi Muscle
Introduction
The orbicularis oculi muscle is a muscle located in the eyelids. It is a sphincter muscle arranged in concentric bands around the upper and lower eyelids. The main function of the orbicularis oculi muscle is to close the eyelids. This occurs when the muscle contracts. It also assists in the drainage of tears from the eyes. Whenever the orbicularis oculi muscle contracts, the tears are drawn from the tear film via the lacrimal pump system.[1][2][3]
Structure and Function
The orbicularis oculi muscle closes the eyelids and assists in pumping the tears from the eye into the nasolacrimal duct system. The orbital section of the orbicularis oculi is more involved in the voluntary closure of the eyelid, such as with winking and forced squeezing. The preseptal section is involved in both the voluntary forced closure as well as the involuntary blink closure of the eye and keeping the eyelids closed during sleep. The pretarsal section is more involved in the involuntary blink closure of the eye and keeping the eyelids closed during sleep.
When the palpebral orbicularis muscle contracts, it shortens the canaliculi of the nasolacrimal duct system, squeezing the tears into the lacrimal sac. Also, the muscle also pulls the lacrimal sac laterally and forward, creating a vacuum to draw the tears into the sac.
Embryology
Orbicularis oculi muscle forms from mesoderm in the eyelids in the twelfth week. It is derived from the mesenchyme of the second pharyngeal arch.
Blood Supply and Lymphatics
The orbicularis oculi muscle receives its blood from the branches of the facial artery and superficial temporal artery (which are branches of the external carotid artery), as well as the ophthalmic artery (which is a branch of the internal carotid artery).
The common carotid arteries arise from the brachiocephalic trunk on the right side and directly from the aortic arch on the left side. At the superior border of the thyroid cartilage in the neck, each common carotid artery divides into the internal and external carotid arteries.
The external carotid artery continues superiorly and splits into a number of branches, including the facial artery, superior temporal artery, superior thyroid artery, lingual artery, facial artery, ascending pharyngeal artery, occipital artery, maxillary artery, and posterior auricular artery. The facial artery then courses from the mandibular area, up the side of the nose and to the medial canthus of the eye, where it is called the angular artery. Branches of the facial artery and superficial temporal artery supply the orbicularis oculi muscle.
The internal carotid artery enters the skull through the carotid canal in the temporal bone. It travels through the cavernous sinus and then splits off a major branch call the ophthalmic artery. The ophthalmic artery enters the orbit through the optic canal. Within the orbit, it divides into various branches, including the lacrimal artery, supraorbital artery, ethmoidal arteries, supratrochlear artery, central retinal artery, ciliary arteries, and muscular branches. Some of these branches, such as the lacrimal artery and supraorbital artery, supply the orbicularis oculi muscle.
Nerves
The orbicularis oculi are innervated by the seventh cranial nerve, the facial nerve. The upper half of the orbicularis oculi muscle receives its innervation from the temporal branch of the seventh cranial nerve (facial nerve), while the lower half receives its innervation from the zygomatic branch of the seventh cranial nerve (facial nerve).
Intracranially, the seventh cranial nerve starts in the pons of the brainstem. It goes through the internal acoustic meatus and then the facial canal of the temporal bone. The seventh nerve then exits the skull through the stylomastoid foramen, which is posterior to the styloid process of the temporal bone. It then passes through the parotid gland where it splits into five branches, which innervate the muscles of facial expression. These branches are the temporal branch, zygomatic branch, buccal branch, marginal mandibular branch, and cervical branch.
The temporal branch courses superiorly and medially to innervate the upper half of the orbicularis oculi muscle as well as the frontalis muscle and corrugator supercilii muscle. The zygomatic branch courses medially and innervates the lower half of the orbicularis oculi muscle.
Muscles
The orbicularis muscle is located just underneath the skin of the eyelid. In general, the muscle attaches to the medial canthal region medially and the lateral canthal region laterally. The orbicularis oculi muscle is divided into two sections, the orbital and palpebral sections. The palpebral section is further subdivided into the preseptal and pretarsal sections. These sections have a complex arrangement of attachments to the surrounding structures.
The orbital section of the orbicularis oculi muscle attaches medially to the anterior limb of the medial canthal tendon and the surrounding periosteum. Laterally, the orbital section attaches to the lateral palpebral raphe. At the muscle’s peripheral borders, it interdigitates into the surrounding muscles, such as the frontalis muscle superiorly.
The preseptal orbicularis oculi muscle divides medially into a deep head and a superficial head. The deep head of the muscle attaches to the fascia around the lacrimal sac as well as the posterior lacrimal crest, while the superficial head of the muscle attaches to the anterior limb of the medial canthal ligament. Laterally, the preseptal orbicularis oculi muscle attaches to Whitnall’s lateral orbital tubercle, which is deep to the lateral palpebral raphe.
The pretarsal orbicularis oculi muscle also divides medially into a deep head and a superficial head. The deep head of the muscle attaches behind the posterior lacrimal crest and to the medial canthal tendon, while the superficial head of the muscle attaches to the anterior lacrimal crest. The deep or posterior head of the pretarsal orbicularis oculi muscle is also known as Horner’s muscle. Laterally, the muscle attaches to the lateral canthal tendon. The superior and inferior pretarsal orbicularis oculi muscles are overlain the respective upper and lower eyelid tarsi. The muscle is firmly adherent the underlying tarsus.
The marginal portion of the palpebral orbicularis muscle adjacent to the eyelid margin is known as the muscle of Riolan or pars ciliaris. This superficial portion of the muscle can be seen along the length of the upper and lower eyelid margins as a colored line and is a surface anatomic landmark known as the gray line. The gray line is a clinical landmark often used in the surgical repair of lacerations of the eyelid margin to help surgeons realign the margins precisely.
Clinical Significance
If the orbicularis oculi muscle does not function for any reason, such as with Bell’s palsy or paralysis of the seventh cranial nerve, then the eyelids cannot close well. This condition requires aggressive lubrication of the eye with artificial tear drops and ointment to prevent exposure keratitis. If not treated adequately, the poor closure of the eyelids can result in significant pain, corneal scarring, corneal ulcer, and ultimately corneal perforation with a possible loss of the eye.[4][5][6]
The orbicularis oculi muscles can also contract involuntarily in benign essential blepharospasm. This can severely affect a person's ability to perform activities of daily living, such as reading and driving, as the person has a hard time holding the eyes open to see properly. Periodic chemodenervation of the orbicularis oculi muscle with botulinum toxin injections can significantly ameliorate the symptoms.[7][8]
(Click Image to Enlarge)
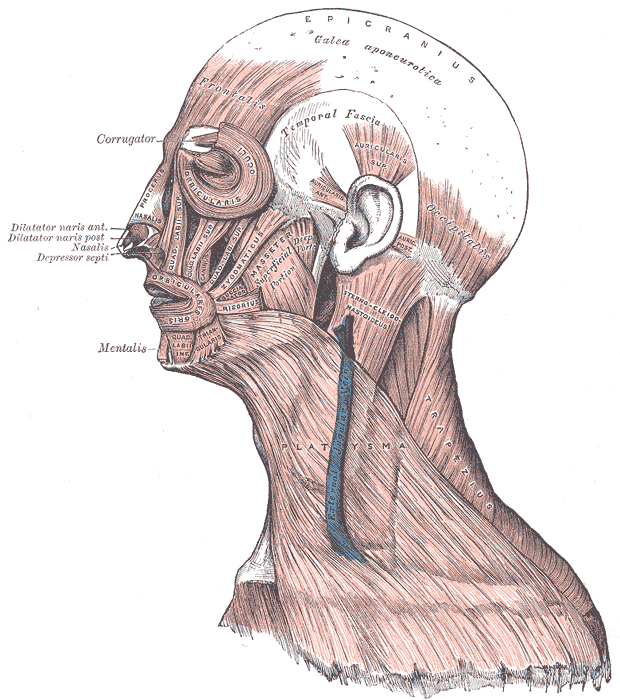
Head Face and Neck Muscles, Epicranius, Galea aponeurotica, Frontalis, Temporal Fascia, Auricularis Superior, Auricularis Anterior, Auricularis Posterior, Occipitalis, Sternocleidomastoid, Platysma, Trapezius, Orbicularis Oculi, Corrugator, Procerus Nasalis, Dilatator Naris Anterior, Dilatator Naris Posterior, Depressor Septi, Mentalis, Orbicularis Oris, Masseter, Zygomaticus, Risorius
Contributed by Gray's Anatomy Plates