Anatomy, Head and Neck, Parotid Gland
- Article Author:
- Hannah Chason
- Article Editor:
- Brian Downs
- Updated:
- 7/27/2020 12:13:36 PM
- For CME on this topic:
- Anatomy, Head and Neck, Parotid Gland CME
- PubMed Link:
- Anatomy, Head and Neck, Parotid Gland
Introduction
The parotid gland, along with the submandibular and sublingual glands, is one of the three paired major salivary glands. The parotid is the largest of the three glands and is bordered superiorly by the zygomatic arch, anteriorly and medially by the masseter, and posteriorly by the sternocleidomastoid. The saliva secreted from these glands moistens the mouth which helps with chewing, swallowing, phonation, and digestion.
The facial nerve courses through the body of the parotid gland, creating a unique relationship which requires focused attention when performing parotidectomies or other surgery in the region of the gland.[1]
Structure and Function
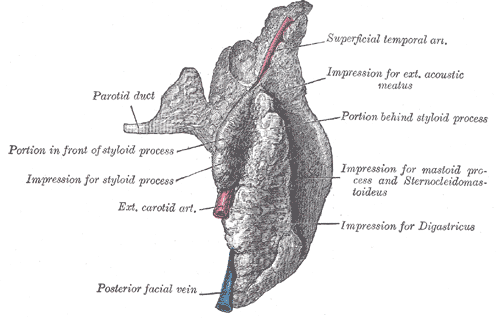
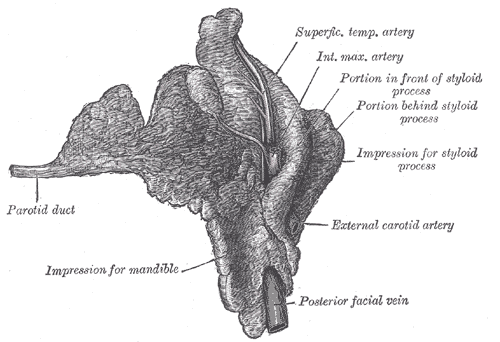
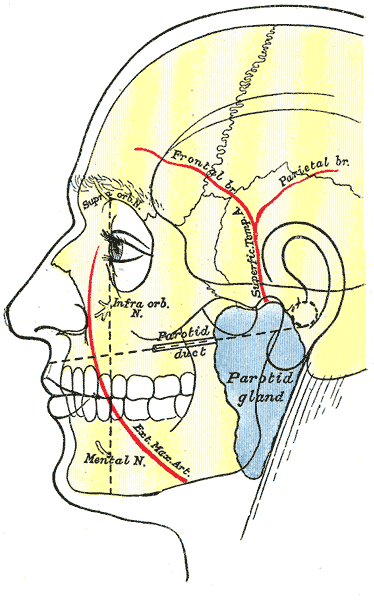
The parotid gland can be palpated anterior and inferior to each ear on the lateral surface of the cheek. The inferior aspect is located posterior to the level of the angle of the mandible, and the superior aspect is adjacent to the zygomatic arch. Each parotid gland is comprised of a superficial lobe and a deep lobe divided by the posterior facial vein and facial nerve. Between the lobes of the gland is fatty tissue to accommodate movement of the mandible. The superficial lobe lies lateral to the facial nerve and overlies the lateral surface of the masseter muscle. The deep lobe lies medial to the facial nerve and is situated between the mastoid process of the temporal bone and the mandibular ramus. Surrounding each gland is a fascial capsule called the parotid sheath.[2]
The parotid duct (Stensen's duct), which provides an exit for the gland’s secretions, passes through the anterior edge of the gland in the superficial lobe, turns medially at the anterior border of the masseter, penetrates the buccinator, then enters the oral cavity lateral to the second maxillary molar.[2]
As one of the three large paired salivary glands, the parotid is a serous gland that produces saliva to moisten the mouth, helping with chewing, swallowing, phonating, and digestion. Saliva also functions to prevent dental caries. The parotid tissue is composed of serous acinar cells and may contain accessory glandular tissue formed of mucinous acinar cells. Each serous acinus is surrounded by myoepithelial cells that are bordered by a basement membrane layer. The myoepithelial cells contract to help expel secretions from the acini. Saliva is first produced in the acinar lumen and then altered into a mixture of electrolytes and macromolecules as it is actively transported through the ducts. The saliva is hypotonic by the time it has reached the mouth, but salivary flow rates can influence the electrolyte composition. In addition to electrolytes, saliva also contains mucin and digestive enzymes. The most important enzyme is amylase, which is important in the initial digestion of carbohydrates. Under certain pathological conditions such as dehydration, salivary flow can decrease, the gland can swell, and infection can ensue. This painful condition is called sialadenitis.
Embryology
The salivary glands begin to develop between weeks 6 and 7 of gestation. They start as epithelial buds in the oral cavity then extend into the underlying mesenchyme.
Blood Supply and Lymphatics
Blood Supply
The external carotid artery (ECA) is the arterial supply to the parotid. The ECA bifurcates into the superficial temporal artery (STA) and maxillary artery (MA) medial to the parotid gland. The STA branches into the transverse facial artery, which runs anteriorly between the zygoma and parotid duct and supplies the parotid duct, parotid gland, and masseter muscle. The MA supplies the infratemporal fossa and the pterygopalatine fossa after exiting the medial portion of the parotid.
The retromandibular vein is formed from the maxillary and superficial temporal veins and provides venous outflow for the parotid. It courses deep to the facial nerve, and it may have variable anatomy before it joins the external jugular vein.
Lymphatics
There are many lymph nodes within and around the parotid glands. The parotid is the only salivary gland with two nodal layers which drain into superficial and deep cervical lymph systems. Most nodes are located within the superficial lobe between the gland and the parotid capsule. The parotid gland and external auditory canal drain to both the superficial and deep nodes. The superficial nodes additionally drain the pinna, scalp, eyelids, and lacrimal glands. The deep nodes drain the middle ear, nasopharynx, and soft palate. Skin cancers from the face and/or scalp, as well as other head and neck cancers, can cause pathologically enlarged lymph nodes in the parotid gland which can indicate regional spread of carcinoma.
Nerves
Parasympathetic innervation to the parotid comes from the glossopharyngeal nerve (CN IX) and causes secretion of saliva. The parasympathetic fibers of CN IX originate in the inferior salivatory nucleus in the medulla and travel through the jugular foramen to the inferior ganglion. A small branch of CN IX, called the tympanic or Jacobsen's nerve, forms the tympanic plexus within the middle ear. These preganglionic fibers become the lesser petrosal nerve and course through the middle cranial fossa before exiting through the foramen ovale. They synapse in the otic ganglion, and the postganglionic parasympathetic fibers join the auriculotemporal nerve to innervate the parotid gland to secrete saliva.
The neurotransmitters acetylcholine (ACh) and norepinephrine (NE) both act within the parotid. ACh binds muscarinic receptors to stimulate acinar activity and ductal transport. It also utilizes second messenger activity via production of inositol triphosphate leading to increased calcium concentration within the cells to increase salivary volume secretion.
Norepinephrine transmits sympathetic nervous system impulses via postganglionic sympathetic fibers to the salivary glands. NE binds beta-adrenergic receptors resulting in activation of the adenylate cyclase second messenger system leading to the formation of cAMP and phosphorylation of various proteins and activation of enzymes. Sympathetic outflow thickens saliva.
The facial nerve courses through the parotid gland, providing motor supply to the muscles of facial expression but does not provide innervation to the gland itself.
Surgical Considerations
Because the facial nerve courses through the glandular substance of the parotid gland, an accurate understanding of the anatomy is crucial when performing parotidectomies. Any surgery for parotid tumor should identify the facial nerve. Identification of the facial nerve trunk (FNT) and its branches are critical to prevent damage to the nerve. Some bony and soft tissue landmarks commonly used to identify the FNT are the cartilaginous tragal pointer, the tympanomastoid suture, the posterior belly of digastric, the styloid process, and the retromandibular vein.[1]
If an obstructing stone (sialolithiasis) causes refractory inflammation despite medical treatment, a procedure called sialoendoscopy can be performed for relief. A sialoendoscopy uses an endoscope to visualize the stone to aid in management.
Neoplastic disease can affect the parotid gland. The most common primary parotid tumor is pleomorphic adenoma. Metastatic disease can also affect the parotid via lymph node involvement. Management of neoplastic disease of the parotid typically includes surgical resection.
Clinical Significance
Sialadenitis
- Sialadenitis is due to inflammation of the salivary gland caused by obstruction and infection by bacteria, viruses, or stones.
- Signs and symptoms include pain, swelling of the gland, and fever.
- The most common microorganisms causing sialadenitis are staphylococcal bacteria and the mumps virus.[3]
- Treatment includes antibiotics for bacterial infections, oral hydration, warm compresses, and sialagogues. For cases of refractory infection, surgical management (i.e., to drain abscess) may be indicated.[4]
Sialolithiasis
- Sialolithiasis is a stone or calculus lodged in a salivary duct. It is the most common cause of obstructive salivary gland disease and is responsible for half of all major salivary gland disorders.[5]
- Signs and symptoms include pain and swelling in the affected duct, particularly during and after eating.[6]
- Ultrasound imaging is the first step in diagnosis. CT, MRI and MR sialography can be used in patients with a high suspicion for ductal obstruction but a negative or inconclusive ultrasound study.[5]
- The goal of treatment is to increase the flow of saliva through the duct with oral hydration or sialogogues. Surgical removal of the calculus is required for chronic sialolithiasis that has failed conservative treatment.[7]
(Click Image to Enlarge)
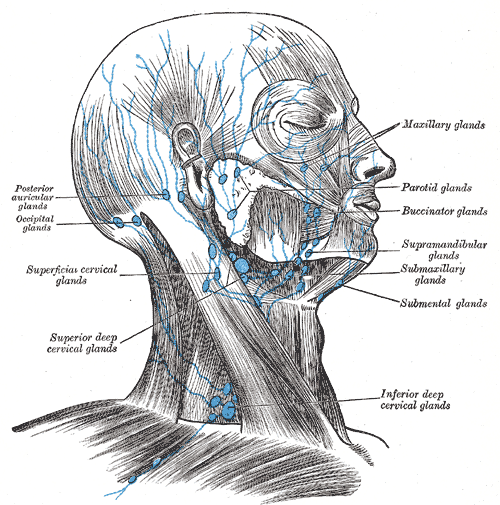
Lymph notes of the head and Neck, Posterior auricular glands, occipital glands, Superficial cervical glands, Superior deep cervical glands, Inferior deep cervical glands, Submental glands, Submaxillary glands, Supramandibular glands, Buccinator glands, Parotid glands, Maxillary glands
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)