Anatomy, Abdomen and Pelvis, Anal Canal
- Article Author:
- Abdelwahab Ahmed
- Article Editor:
- Waqar Qureshi
- Updated:
- 7/31/2020 3:59:00 PM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Anal Canal CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Anal Canal
Introduction
The anal canal, thought of mostly as the final exit for what we ingest, is more intricate a structure than most would believe. At an average of 2.5 cm to 4 cm in length, it plays a vital role as a defense against organisms trying to make their way into the body, can differentiate between solid/ liquid and gas, and as a set of muscles that continence. Often not considered until something is wrong, the anal canal has its fair share of pathologies, some of which require measures as conservative as a sitz bath, while others severe enough to require surgical resection or radiation.
Structure and Function
The anal canal serves as the continuation of the rectum to the end of the alimentary system, the anus. It has two sphincters; the internal anal sphincter (IAS) and the external anal sphincter (EAS). The structure of the internal and external sphincters is quite different from one another. The transition from the rectum to anus is marked by the anorectal ring, which is the area where the muscles of the intrinsic and extrinsic sphincters blend superiorly with the puborectalis muscle. The division between the internal and external anal sphincters is marked by the pectinate line, a series of longitudinal folds, called anal columns, consisting of columnar epithelium. The superior portion of the anal canal contains the IAS, and the inferior portion includes the EAS. Each sphincter has a distinct neurovascular supply. The function of each is as follows[1][2]:
- Internal Anal Sphincter (IAS)
- Not under voluntary control
- The function is dependent on the integrity of the rectoanal inhibitory reflex (RAIR), which involves the reflexive relaxation of the IAS in the presence of rectal distension.
- Maintains a resting pressure in the absence of rectal distension
- The resting pressure of the IAS is widely accepted as a direct measure of its functionality and is often assessed in a variety of pathologies.
- External Anal Sphincter (EAS)
- Under voluntary control
- Acts to keep the orifice of the anal canal closed and relaxes upon defecation
- While the RAIR causes the IAS to relax in the presence of rectal distension, the EAS serves to keep the stool in the anal canal until one is ready to defecate.
Embryology
As with its structure and function, the embryology of the anal canal differs between the IAS and the EAS. The IAS derives from the endoderm of the hindgut. The EAS derives from the ectoderm. At birth, the EAS is not fully developed and not yet under complete voluntary control. The individual usually achieves voluntary control of the EAS near the ages of 18 to 24 months.[3][4]
Blood Supply and Lymphatics
One way to approach the blood supply and lymphatics of the anal canal is to consider the supply above and below the pectinate line and that which supplies both. [5]
Above the pectinate (dentate) line:
This area is supplied by the terminal branches of the superior rectal artery. This artery is a branch of the inferior mesenteric artery. The lymphatic drainage above the pectinate line is to the inferior mesenteric lymph nodes.
Below the pectinate line:
This area is supplied by the middle rectal artery and the inferior rectal artery. The middle rectal artery is a branch of the internal iliac artery while the inferior rectal artery is a branch of the internal pudendal artery. The lymphatic drainage below the pectinate line is to the superficial inguinal lymph nodes.
Portosystemic Venous Connection- The Overlap:
The venous drainage above the pectinate line is to the superior rectal veins which drain into the inferior mesenteric vein and ultimately drain into the systemic veins. The venous drainage below the pectinate line is to the internal pudendal veins which drain into the internal iliac vein and ultimately into the portal venous system. Present between these two systems of drainage is a portosystemic anastomosis which allows for these systems to be connected. This connection can have consequences when one system has much more pressure than the other and can result in the development of anorectal varices. Not unique to the anal canal, these portosystemic anastomoses are also present at the level of the esophagus and the umbilicus.[6]
Nerves
Similar to the blood supply and lymphatics, it is also useful to discuss the nervous system of the anal canal from the perspective above and below the pectinate line. These two areas have different innervations and respond to different stimuli. [7]
Above the pectinate (dentate) line:
This region receives autonomic innervation from the inferior hypogastric plexus. The parasympathetic innervation inhibits the tone of the IAS and evokes a peristaltic contraction to allow defecation. Sympathetic innervation works oppositely to maintain the tone of the IAS and preserve continence. This region of the anal canal is sensitive to stretch.
Below the pectinate line:
This region receives somatic innervation derived from branches of the pudendal nerve. This region of the anal canal is sensitive to pain, temperature, and touch.
Physiologic Variants
Little variation exists in the literature on the anal canal. Multiple case reports have discussed anal canal duplication in which a neonate is born with an extra anal canal, either superior or posterior to the main canal. Investigation revealed the duplicated canal to have most of the same features as a normal anal canal; however, it ends in a blind pouch with no connection to the rectum. Currently, it is treated with surgical excision as it can serve as a potential nidus of inflammation, fistulization, or malignancy.[8]
There is, however, a variation of the anal canal as we age. The IAS increases in thickness as we age; the effect is more pronounced in females over the age of 50. Current guidelines consider maximal IAS thickness greater than 4 mm as abnormal in patients under 50 years of age. The cut-off is increased to 5 mm in those over 50 years of age. This becomes important when identifying patients with hypertrophy of the IAS.[9]
Surgical Considerations
The tight space and compact anatomy of the anal canal creates a difficult compartment for surgical procedures. During surgery involving the anal canal, the surgeon can appreciate the different zones and will be able to identify the pectinate line marking the transition between the upper portion and lower portion of the anal canal.
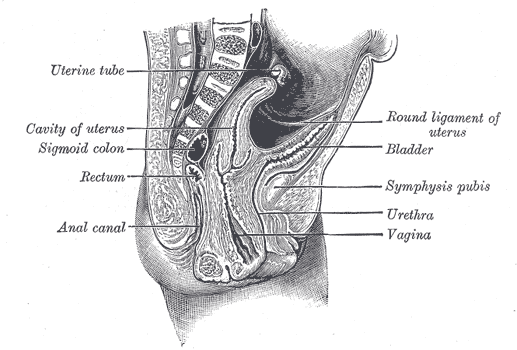
The anatomy of the anal canal makes sphincter-saving surgery during cases of lower rectal cancer very challenging. These surgeries come with potential consequences like anal sphincter compromise with incontinence or permanent colostomy. Because of the limited window available for surgeons, other approaches have been explored, such as transvaginal, transperineal, trans-sacral, and abdominal access.[10]
Clinical Significance
Incontinence
As mentioned above, the anal canal and its muscles serve to keep us continent. Consequently, any failure of the anal canal musculature may result in fecal incontinence. The current guidelines suggest anal manometry to assess for sphincter tone as a possible cause. Positive manometry revealing a dysfunction of sphincter tone is usually followed by anorectal imaging to evaluate structural integrity.[11]
Hemorrhoids
Hemorrhoids are a common anal disorder which involves the engorgement of veins in the lower part of the anus and rectum. A variety of factors predispose individuals to the development of hemorrhoids such as pregnancy, age, diarrhea, chronic constipation, sitting for too long (especially on the toilet), heavy lifting, anal intercourse, obesity, and genetics.
There are two major types of hemorrhoids: (1) internal hemorrhoids and (2) external hemorrhoids. Internal hemorrhoids are deep within the anal canal and are usually painless because of the lack of sensory innervation in that region, being above the dentate line. These hemorrhoids often present with painless bleeding and, upon straining, may prolapse out of the anus. External hemorrhoids exist within the skin around the anal opening and are often painful and itchy.
As far as treatment, hemorrhoids often resolve on their own, but patients can relieve the discomfort using dietary fiber, stool softeners, and daily sitz bath. It is also important to advise these patients about adequate fiber intake, decreased straining in the washroom, and decreased time spent sitting on the toilet. Large or bothersome hemorrhoids may be treated In the office with banding or by surgical hemorrhoidectomy.[12][13]
Anal Cancer
Anal cancer is a disease in which the normal cells of the anus become malignant. Most cases are related to the human papillomavirus (HPV). Factors that enhance the risk of anal cancer include smoking and immunodeficiency. The prognosis of anal cancer is mostly dependent on the size of the tumor and whether cancer has spread to the lymph nodes. Following the identification of anal cancer, it is staged from 0 to 5 based on size and spread with stage 5 carrying the worst prognosis. Treatment of anal cancer often includes surgery, radiation therapy, chemotherapy, or some combination of these methods.[14]
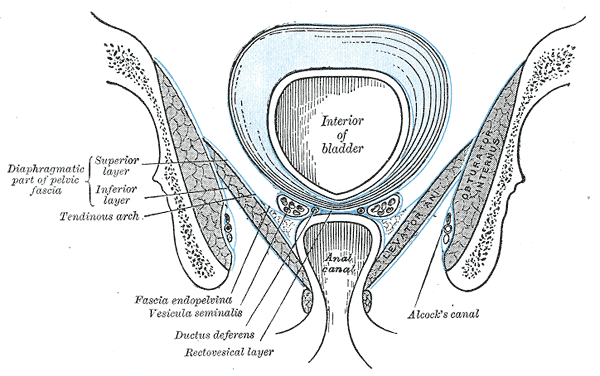
(Click Image to Enlarge)
(Click Image to Enlarge)

Median sagittal section of pelvis, Sacrum, Peritoneum, Vesical Layer, Fascia of urogenital diaphragm; Superior and Inferior Layer, Bladder, Prostate, Symphysis pubis, Rectum, Anal Canal, corpus cavernosum penis and Urethra, Bulb, Scrotum, Urogenital diaphragm, Colles Fascia, Transversus Perinei Superficialis, Rectal Layer, Vesicula seminalis, Rectovesical layer, Capsule of Prostate
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)
(Click Image to Enlarge)