Tension Pneumothorax
- Article Author:
- Ruchi Jalota
- Article Editor:
- Edouard Sayad
- Updated:
- 8/11/2020 7:32:32 PM
- For CME on this topic:
- Tension Pneumothorax CME
- PubMed Link:
- Tension Pneumothorax
Introduction
Pneumothorax is the collapse of the lung when air accumulates between the parietal and visceral pleura inside the chest. The air is outside the lung but inside the thoracic cavity. This places pressure on the lung and can lead to its collapse and a shift of the surrounding structures. Pneumothoraces can be traumatic or atraumatic. Traumatic pneumothoraces occur secondary to penetrating or blunt trauma or iatrogenic. Iatrogenic pneumothorax is a traumatic pneumothorax that results from injury to the pleura, with air introduced into the pleural cavity secondary to diagnostic or therapeutic medical intervention. Atraumatic pneumothoraces are further divided into primary (unknown etiology) and secondary (patient with an underlying pulmonary disease).
Pneumothoraces are classified as simple (no shift of mediastinal structures), tension (shift in mediastinal structures present), or open (air passing through an open chest wound). A tension pneumothorax is a severe condition that results when air is trapped in the pleural space under positive pressure, displacing mediastinal structures, and compromising cardiopulmonary function. Early recognition of this condition is life-saving both outside the hospital and in modern ICU. Knowledge of necessary emergency thoracic decompression procedures are essential for all healthcare professionals. Traumatic and tension pneumothoraces are life-threatening and require immediate treatment.[1]
Etiology
Causes of traumatic pneumothorax:[2][3][4]
Iatrogenic: (Induced by a medical procedure)
- Central venous catheterization in the subclavian or internal jugular vein
- Lung biopsy
- Barotrauma due to positive pressure ventilation
- Percutaneous tracheostomy
- Thoracentesis
- Pacemaker insertion
- Bronchoscopy
- Cardiopulmonary resuscitation
- Intercostal nerve block
Non-Iatrogenic: (Due to external trauma)
- Penetrating or blunt trauma
- Rib fracture
- Diving or flying
Causes of tension pneumothorax:
All the above causes can further cause tension pneumothorax as well as:
- Idiopathic spontaneous pneumothorax
- Open pneumothorax
- Conversion of spontaneous pneumothorax to tension
Epidemiology
Traumatic and tension pneumothoraces are more common than spontaneous pneumothoraces. Transthoracic needle aspiration and central venous catheters are usually the most common causes of iatrogenic pneumothorax. The rate of iatrogenic pneumothoraces is increasing in US hospitals as intensive care modalities have increasingly dependant on positive pressure ventilation and central venous catheters. Central venous catheterization increases the risk of pneumothoraces when placed in the internal jugular or subclavian. The incidence is about 1 to 13% but increases to 40% if multiple attempts are made. These numbers are lower if procedures are done under ultrasound. Iatrogenic pneumothorax usually causes substantial morbidity but rarely death. The incidence is 5 to 7 per 10,000 hospital admissions.
Tension pneumothoraces can develop in 1 to 2% of cases initially presenting with idiopathic spontaneous pneumothoraces. It is difficult to determine the actual incidence of tension pneumothorax as by the time trauma patients are transported to trauma centers, they have already received decompressive needle thoracotomies. Patients with trauma tend to have an associated pneumothorax or tension pneumothorax 20% of the time. In cases of severe chest trauma, there is an associated pneumothorax 50% of the time. The incidence of traumatic pneumothorax depends on the size and mechanism of the injury. A review of military deaths from thoracic trauma suggests that up to 5% of combat casualties with thoracic trauma have tension pneumothorax at the time of death.[3][4][5][6][7][6]
Pathophysiology
Before understanding the pathophysiology of tension and traumatic pneumothoraces, it is essential to understand the normal lung physiology. Pleural cavity (or intrapleural) pressure is negative as compared to the lung pressure and atmospheric pressure. There is a tendency of the lung to recoil inward and the chest wall to recoil outward. That pressure gradient between the lung and pleural space prevents the lung from collapsing. During a pneumothorax, a communication develops between the pleural space and the lung, resulting in air movement from the lung into the pleural space. This takes away the pressure gradient that is usually present and causes a progressive rise in the intrapleural pressure. This rise in pressure further compresses the lung and decreases its volume. The ipsilateral lung is unable to function at its normal capacity, and ventilation is then reduced, resulting in hypoxemia.[2][8]
Tension pneumothorax is common in ICU ventilated patients. Tension pneumothorax occurs when the air enters into the pleural space but is not able to fully exit, similar to a one-way valve mechanism through the disrupted pleura or tracheobronchial tree. During inspiration, a sizeable high-pressure air collection accumulates in the intrapleural space and is not able to completely exit during expiration. This will cause the lung to collapse on the ipsilateral side. As the pressure increases, it will cause the mediastinum to shift towards the contralateral side, contributing further to hypoxemia. In severe cases, the increased pressure can also compress the heart, the contralateral lung, and the vasculature leading to hemodynamic instability. This is due to impaired cardiac filling and reduced venous return. Hypoxemia also triggers pulmonary vasoconstriction and increases pulmonary vascular resistance. As a result, hypoxemia, acidosis, and decreased cardiac output can lead to cardiac arrest and, ultimately, death if the tension pneumothorax is not managed in a timely fashion.[2][8]
Traumatic pneumothorax occurs secondary to a penetrating (e.g., gunshot wounds, stab wounds) or blunt chest trauma. Depending on the depth of a penetrating chest wound, the air will flow into the pleural space either through the chest wall or from the visceral pleural of the tracheobronchial tree. With a blunt force trauma, a pneumothorax can occur if a rib fracture or dislocation lacerates the visceral pleura. An alternative mechanism is through blunt thoracic trauma, where the increased alveolar pressure can cause the alveoli to rupture, which results in the air entering the pleural cavity.[2]
History and Physical
Patients with pneumothoraces can be either asymptomatic or symptomatic. In a small pneumothorax, many patients may present without symptoms.
Symptomatic patients will present with sharp pleuritic pain that can radiate to the ipsilateral back or shoulder. The severely symptomatic patients will present with shortness of breath. Upon history taking, it is essential to note whether the patient previously had a pneumothorax as recurrence is seen in more than15% of cases on either the ipsilateral or contralateral side.
On examination, it is essential to assess for signs of respiratory distress, including increased respiratory rate, dyspnea, and retractions. On lung auscultation, decreased or absent breath sounds on the ipsilateral side, reduced tactile fremitus, hyper-resonant percussion sounds, and possible asymmetrical lung expansion are suggestive of pneumothorax. Symptoms of tension pneumothorax are more severe. With tension pneumothorax, patients will have signs of hemodynamic instability with hypotension and tachycardia. Cyanosis and jugular venous distension can also be present. In severe cases or if the diagnosis was missed, patients can develop acute respiratory failure, and possibly cardiac arrest. In some instances, subcutaneous emphysema can also be seen. The diagnosis of tension pneumothorax must be made immediately through clinical assessment as waiting for imaging, if not readily available, may delay management and increase mortality.[2][8][9]
Evaluation
Initial assessment to determine whether the patient is stable or unstable dictates further evaluation. If the patient is hemodynamically unstable and in acute respiratory failure, bedside ultrasound should be performed to confirm the diagnosis if it is available for immediate use. Concurrently, patients should be stabilized, and a complete assessment of airway, breathing, and circulation should be performed. Emergent needle decompression or chest tube thoracotomy must be performed immediately if the diagnosis is highly suspected.
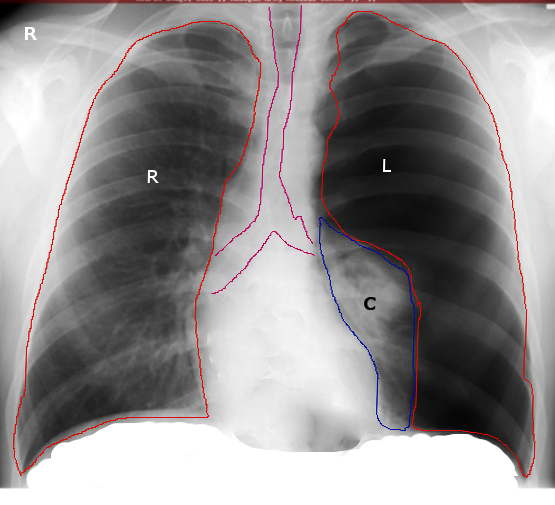
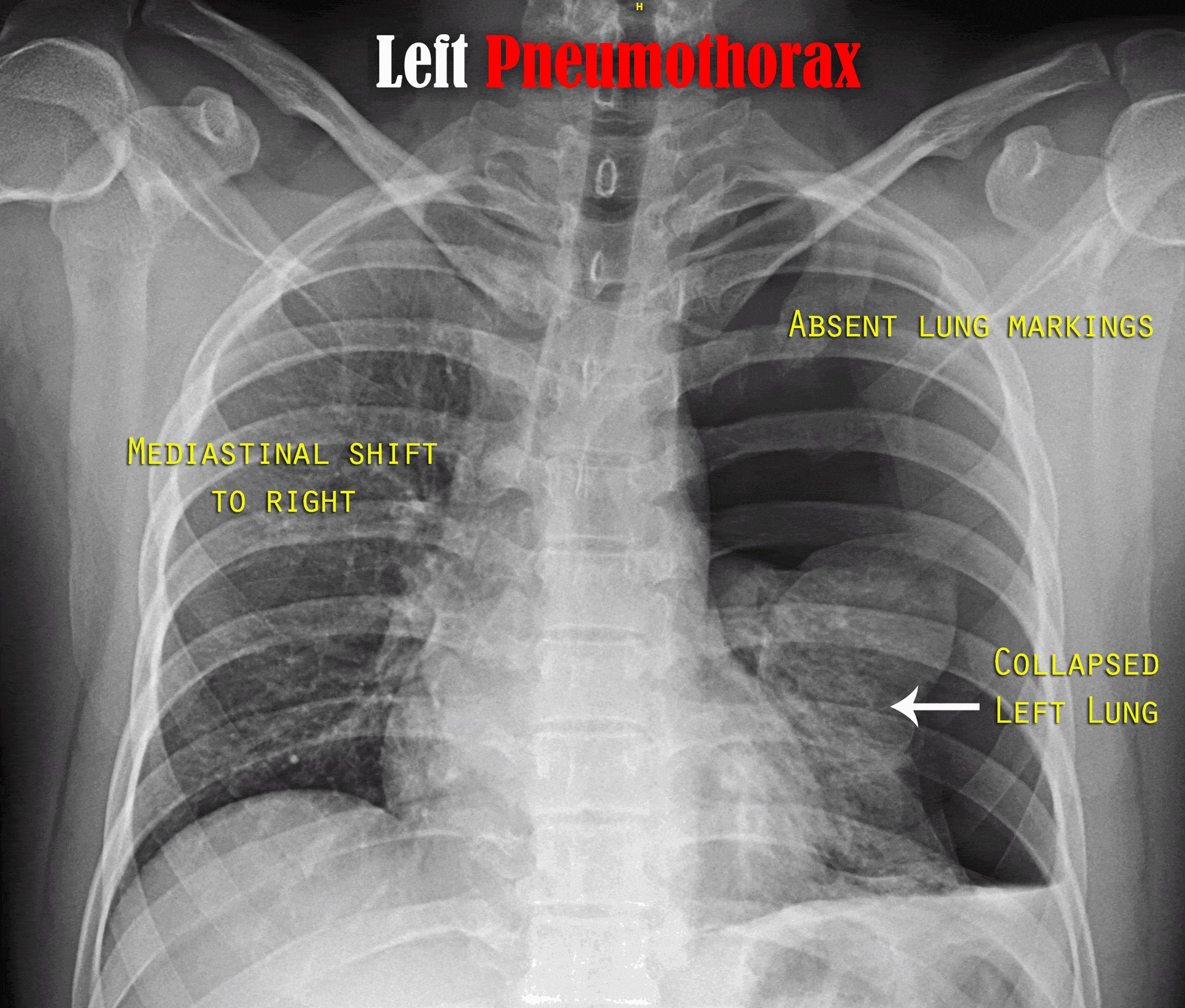
When a patient is hemodynamically stable, radiographic evaluation is recommended. The initial assessment is with a chest radiograph (CXR) to confirm the diagnosis.
CXR can demonstrate one or more of the following:
- A thin line representing the edge of the visceral pleura
- Effacement of lung markings distally to this line
- Complete ipsilateral lung collapse
- Mediastinum shift away from the pneumothorax in tension pneumothorax
- Subcutaneous emphysema
- Tracheal deviation to the contralateral side of tension pneumothorax
- Flattening of the hemidiaphragm on the ipsilateral side (tension pneumothorax)
If the diagnosis is unclear on X-ray, then a chest computed tomography can be done. It is the most reliable imaging study for the diagnosis of pneumothorax, but it is not recommended for routine use.
Ultrasound is about 94% sensitive and 100% specific with a skilled operator. This can be used as bedside technique to detect pneumothorax, which may be useful in unstable patients. Ultrasound findings include the absence of lung sliding and the presence of a lung point.[2][10][11][12][13][14][13]
Treatment / Management
Tension and traumatic pneumothoraces are usually managed in the emergency department or the intensive care unit. Management strategies depend on the hemodynamic stability of the patient. In any patient presenting with chest trauma, airway, breathing, and circulation should be assessed. Penetrating chest wounds must be covered with an airtight occlusive bandage and a clean plastic sheeting. Administration of 100% supplemental oxygen can help reduce the size of the pneumothorax by decreasing the alveolar nitrogen partial pressure. This creates a diffusion gradient for nitrogen, thus accelerating the resolution of the pneumothorax. Without oxygen, only 1.25% of the air is absorbed in 24 hours. Positive pressure ventilation should be avoided initially, as it will contribute to increasing the size of the tension pneumothorax. Patients can be placed on positive pressure ventilation after a chest tube is placed.[2][15][16]
If the patient is hemodynamically unstable and clinical suspicion is high for pneumothorax, then immediate needle decompression must be performed without delay. Needle decompression is done at the second intercostal space in the midclavicular line above the rib with an angio-catheter. It results in re-expansion of the collapsed lung. However, the risk of lung re-expanding quickly increases the risk of pulmonary edema. Following needle decompression, a chest tube is usually placed, and an immediate CXR is done to assess the resolution of the pneumothorax.
Assessment of pneumothorax resolution is usually done with serial chest X-rays. When the patient has improved, the lung has fully expanded, and no air leaks are visible, the chest tube is ready to be removed.
Chest tubes are usually managed by experienced nurses, respiratory therapists, surgeons, and ICU physicians. In 90% of the cases, a chest tube is sufficient; however, there are certain cases where surgical interventions are required, and that can either be video-assisted thoracoscopic surgery (VATS) or thoracotomy.[17][18][19][20]
Patients that require surgical intervention are usually patients with bilateral pneumothoraces, recurrent ipsilateral pneumothoraces, first presentation in patients with high-risk professions like pilots and drivers, and patients who have persistent air leak (for more than seven days). During video-assisted thoracic surgery (VATS), pneumothorax is treated with pleurodesis. There are two types of pleurodesis: mechanical or chemical. With mechanical pleurodesis, there is a less than 5% chance of recurrence of pneumothorax. Some options are abrasive scratchpad, dry gauze, or stripping of parietal pleura. Chemical pleurodesis options include talc, minocycline, doxycycline, or tetracycline. Chemical pleurodesis is an alternative if the patient cannot tolerate mechanical pleurodesis. Recent studies have shown that pleurodesis can decrease the rate of recurrence.[21][18][22]
Differential Diagnosis
Differential diagnoses of pneumothorax include:
- Pulmonary embolism
- Acute coronary syndrome
- Acute aortic dissection
- Myocardial infarction
- Pneumonia
- Acute pericarditis
- Rib fracture
- Diaphragmatic injuries
- Esophageal spasm
- Costochondritis
Prognosis
Tension and traumatic pneumothoraces must be treated immediately to avoid further associated morbidity and mortality. Delay in diagnosis and management is associated with poor prognosis. Tension pneumothorax arises from many causes and rapidly progresses to respiratory insufficiency, cardiovascular collapse, and ultimately death if not recognized and treated. In uncomplicated pneumothoraces, recurrence can happen within six months to three years. Recurrences are more common in smokers, COPD, and AIDS patients.[23][24]
Complications
Pneumothorax especially tension pneumothorax is fatal, complications that can occur due to pneumothorax and due to tube thoracostomy are as follow
- Respiratory failure or arrest
- Cardiac arrest
- Pneumopericardium
- Pneumoperitoneum
- Hemothorax
- Bronchopulmonary fistula
- Damage to the neurovascular bundle during tube thoracostomy
- Pain and skin infection at the site of tube thoracotomy
- Empyema
- Pyopneumothorax
Consultations
The diagnosis and management of traumatic and iatrogenic pneumothoraces require multidisciplinary coordination and teamwork. Following specialties should be on board while managing such patients
- Thoracic surgeon
- Pulmonologist
- Interventional radiologist
- Intensivist
Deterrence and Patient Education
Following a pneumothorax, patients need to be educated to avoid air travel until complete resolution or for a minimum of two weeks after surgical intervention. Scuba divers and pilots must be advised not to dive or fly until complete resolution of the pneumothorax by pleurodesis or thoracotomy.[24] Smoking cessation is advised to all patients.
Pearls and Other Issues
If a patient is hemodynamically unstable with a high clinical suspicion for pneumothorax, needle decompression or thoracotomy tube must be placed immediately.
If the patient is stable, then diagnostic imaging, ( i.e CXR) can be done prior to treatment.
Cardiac tamponade can clinically mimic tension pneumothorax.
Patients with high peak inspiratory pressure are at greater risk of tension pneumothorax.
If patients become hemodynamically unstable or have a cardiac arrest, there is high suspicion for tension pneumothorax.
If a chest tube is malpositioning or becomes plugged, it can cease to function and the pneumothorax can recur.
In stable patients, local anesthesia or adequate analgesia/sedation should be administered.
Enhancing Healthcare Team Outcomes
Diagnosis and management of traumatic and tension pneumothoraces require a high level of cooperation among multidisciplinary care providers. The timely and accurate evaluation leads to early interventions decreasing mortality and morbidity. In these situations, care coordination is vital, and having different team members trained and ready to act promptly is life-saving. The first line responders when a patient develops a traumatic or tension pneumothorax vary depending on the situation and underlying etiology. In the case of trauma, this usually happens outside the hospital or in the emergency department (ED). In these cases, emergency medical technicians (EMT), ED nurses, and providers have a role in recognizing this entity promptly and initiating early interventions.
In the case of iatrogenic or tension pneumothoraces happening in the hospital, this is usually in the ICU settings, the operating room, or a procedure suite. Thus, having personnel trained in emergency assessment of pneumothoraces, and having an emergency kit for thoracotomies, intubation, and patient stabilization is essential. Once the patient is stabilized, this condition is managed by a multidisciplinary team, and input from each member is detrimental for successful patient outcomes. This includes ICU team members, surgeons, nurses, respiratory therapists, radiology team, and pulmonologists.