Poikilocytosis
- Article Author:
- Sai Samyuktha Bandaru
- Article Editor:
- Vikas Gupta
- Updated:
- 10/5/2020 10:04:06 AM
- For CME on this topic:
- Poikilocytosis CME
- PubMed Link:
- Poikilocytosis
Introduction
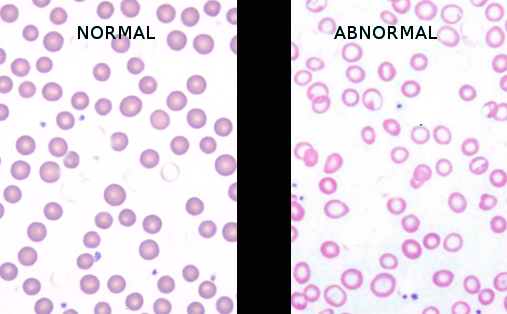
Poikilocytosis is the term used for abnormal shaped red blood cells (RBCs) in the blood. Normal RBCs (also called erythrocytes) are typically disk-shaped, which are thinner in the middle than in the edges, with a diameter of 6.2 to 8.2 micrometers, a thickness at the thickest point of 2 to 2.5 micrometers, and a thickness in the center of 0.8 to 1 micrometers. Poikilocytosis generally refers to an increase in abnormal shaped red blood cells that make up to 10% or more of the total red blood cells. Poikilocytes may be flat, elongated, teardrop, crescent-shaped, or they may have point-like or thorn-like projections, or may have any other abnormal feature.
Etiology
Poikilocytosis is the result of another medical condition. Poikilocytosis causes can be inherited or acquired. Inherited conditions can be caused by genetic abnormalities or mutations. Acquired conditions usually develop later in life.
Inherited causes of poikilocytosis include:
- Sickle cell anemia,[1] RBCs are an abnormal crescent, an elongated spiculated shape known as sickle cells or drepanocytes.
- Thalassemia, a genetic disorder in which abnormal hemoglobin is made, it contains target cells or codocytes.
- Hereditary spherocytosis contains spherocytes.[2]
- Pyruvate kinase deficiency contains echinocytes or burr cells.
- Hereditary elliptocytosis contains elliptocytes.[3]
- McLeod syndrome, a rare genetic disorder that contains acanthocytes.
Acquired causes of poikilocytosis include:
- Iron deficiency anemia, a common type of anemia that is seen when there is insufficient iron in the body, contains elliptocytes (ovalocytes).
- Megaloblastic anemia caused by a deficiency of either folate or vitamin B-12 contains dacrocytes (teardrop cells), elliptocytes.[4][5]
- Autoimmune hemolytic anemia, usually contains schistocytes, spherocytes.
- Liver and kidney disease contain echinocytes or burr cells.
- Alcohol-related liver disease
- Myelofibrosis
- Lead poisoning, chemotherapy treatment, severe infections, cancer, etc.
Causes based on the type of poikilocytosis:
- Spherocytes: Seen in hereditary spherocytosis, autoimmune hemolytic disorders, red cell fragmentation disorders, hemolytic transfusion reactions, ABO hemolytic diseases of newborn/Rh hemolytic disease of the newborn, hypophosphatemia, bartonellosis, snakebites, hyposplenism.
- Codocytes (target cells): Seen in thalassemia, liver disease (cholestatic type), hemoglobin C disorder, recently splenectomy, autosplenectomy in sickle cell disease, iron deficiency disorder.
- Sickle cells (drepanocytes): Seen in sickle cell disease.
- Dacrocytes (teardrop cells): Seen in beta-thalassemia, leukemia, hemolytic anemia, myelofibrosis, megaloblastic anemia.
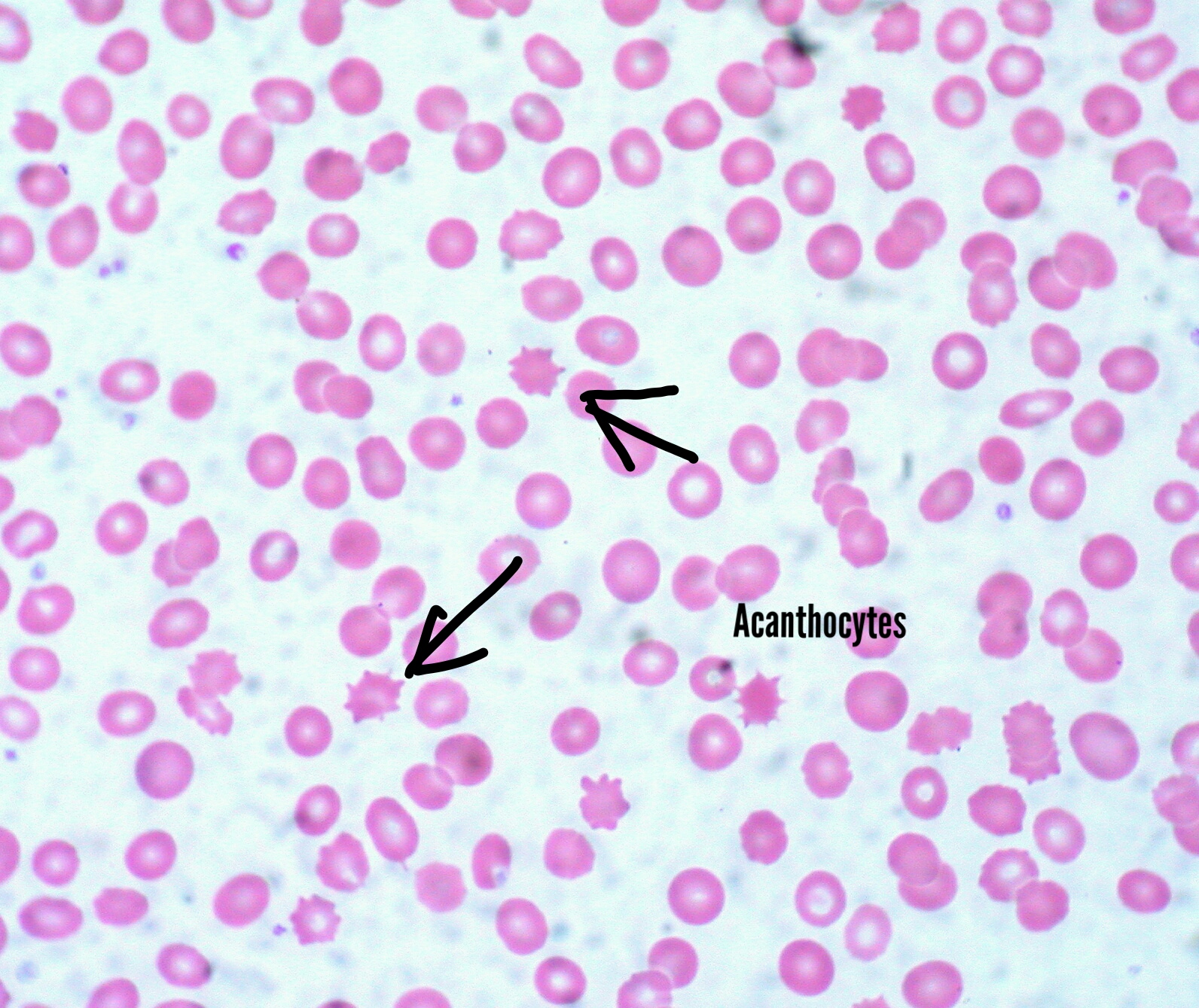
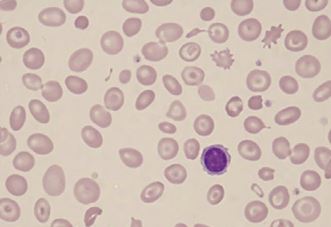
- Acanthocytes (spur cells)[6]: Seen in liver disease, thalassemia, abetalipoproteinemia, splenectomized patients, autoimmune hemolytic anemia, kidney disease, Mcleod syndrome.
- Schistocytes: Seen in hemolytic anemias, sepsis, burns, disseminated intravascular coagulation, platelet disorders like thrombotic thrombocytopenic purpura and hemolytic uremic syndrome.
- Elliptocytes(ovalocytes): Seen in iron deficiency anemia, thalassemia, megaloblastic anemia, myelofibrosis.
- Echinocytes (burr cells): Seen in pyruvate kinase deficiency, kidney disease, cancer.
- Other nonspecific types are leukocytes, stomatocytes (mouth shaped cells), and degmacytes (bite cells).
Epidemiology
Epidemiology depends on the cause of poikilocytosis. In the case of sickle cell disease, it is autosomal recessive in inheritance and has many variants. Heterozygotes are prevalent in Africa, Meditteranean, the middle east, and India. Thalassemias are of two types: alpha and beta, alpha thalassemia is common in sub-Saharan Africa, the Meditteranean, and generally tropical regions. Beta thalassemia is common in the Mediterranean.[7] Hereditary spherocytosis is common in European and North American ancestry.[2][8] Pyruvate kinase deficiency is most commonly seen in northern Europe and Japan.
Pathophysiology
Pathophysiology varies depending on the cause.
- Sickle cells: Seen is sickle cell disease, which is due to hemoglobin S (HbS) by substitution of valine in place of glutamic acid at position 6 of beta-globin of HbA. It has an autosomal recessive inheritance. There are many variants like homozygous, heterozygous, hemoglobin SC disease, hemoglobin S beta thalassemia disease, etc.[9]
- Spherocytes: Seen most commonly in hereditary spherocytosis due to mutations in genes that code for the red blood cell membrane proteins spectrin (alpha and beta), ankyrin, band 3 protein, protein 4.2, and other red blood cell membrane proteins that cause erythrocytes to change shape.[3]
- Target cells (codocytes): Most commonly seen in thalassemia, which are due to impaired production of hemoglobin (Hb). Normal Hb has two alpha, and two beta chains, a decrease in alpha chains is alpha thalassemia, a decrease in beta chains is beta-thalassemia.[10]
- Schistocytes are fragmented RBCs seen most commonly in hemolytic anemias, hemolytic disorders, and platelet disorders like thrombotic thrombocytopenic purpura and hemolytic uremic syndrome.[11]
- Echinocytes and acanthocytes have many causes.
Histopathology
On blood smear examination, different shapes of RBC are seen. Spherocytes are small round cells that lack the flat, light-colored center of regular RBCs. The stomatocyte central part is slit-like, or elliptical, which is different from the regular round shape of RBCs. Stomatocytes are mouth-shaped. Codocytes are also known as target cells as they resemble a bulls-eye. Sickle cells, also known as drepanocytes, are crescent-shaped and elongated RBCs.
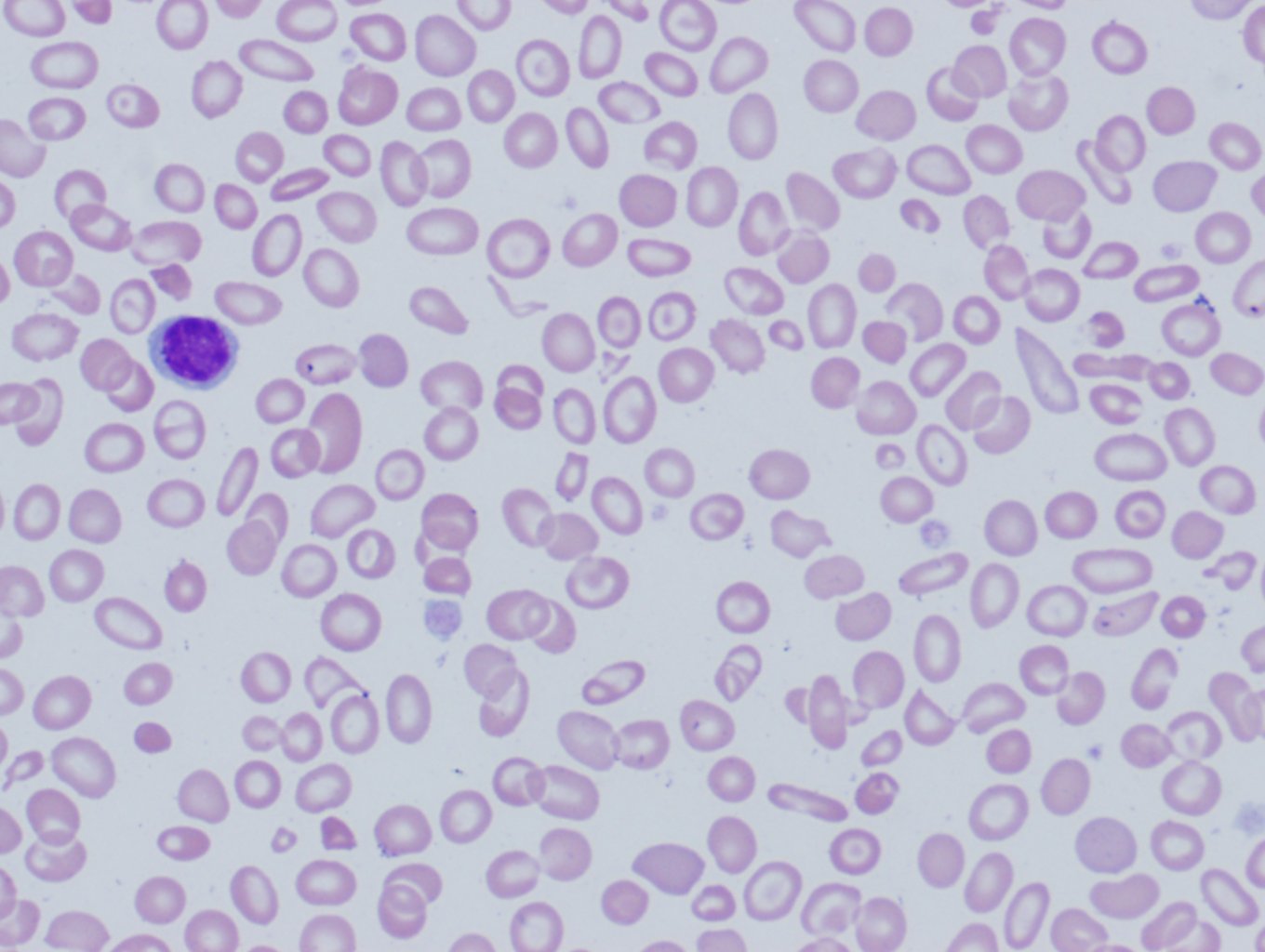
Elliptocytes, also are known as ovalocytes, are oval or cigar-shaped cells with blunt ends. Teardrop cells, or dacryocytes, are abnormal RBCs that have one round and one pointy end. Acanthocytes are the RBCs that have abnormal thorn-like projections (spicules) present on the cell membrane. Echinocytes similar to acanthocytes, also have projections (spicules) on the cell membrane similar to acanthocytes, but the projections in echinocytes are evenly spaced, and more frequently present. Schistocytes are fragmented RBCs.
History and Physical
Red blood cells usually carry oxygen and many nutrients to tissues and organs. In poikilocytosis, RBCs are irregularly shaped and may be unable to carry enough oxygen. Poikilocytosis is caused by another medical condition like anemia, red blood cell membrane defects like hereditary spherocytosis, many genetic causes like sickle cell disease, thalassemia, nutritional disorders like iron deficiency anemia, megaloblastic anemia, and other causes like renal and liver disease.
The main feature of poikilocytosis is having 10 percent or more abnormally-shaped RBCs.
The symptoms and presentations of poikilocytosis vary depending on the underlying condition. Common symptoms of some of the conditions like anemia include
- Fatigue
- Pale skin
- Shortness of breath
- Palpitations
- Weakness
Sickle cell disease commonly presents as (when exposed to cold, dehydration, hypoxia) sickle cell crisis (hemolytic, aplastic, sequestration), acute chest syndrome, vaso-occlusive crisis, and autosplenectomy, etc.
These symptoms are a result of not enough oxygen being delivered to the body’s tissues and organs.
Evaluation
Poikilocytosis is diagnosed with a blood smear examination.[12] This test can be done as part of a routine physical exam, or if the patient is experiencing symptoms of anemia or any unexplained symptoms.
Not all the RBCs will take on an abnormal shape. Patients with poikilocytosis have some normally shaped cells RBCs mixed with abnormally shaped poikilocytes. Sometimes, there are many different types of poikilocytes present in one patient's blood smear in conditions like iron deficiency anemia, and megaloblastic anemia, etc.
In addition to the blood smear, other tests are done to find out the etiology of abnormally shaped RBCs. Examples of other commonly used diagnostic tests include serum iron levels (iron studies), complete blood count (CBC), vitamin B-12, folate, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), and liver function tests.
Treatment / Management
The treatment of poikilocytosis is based on the underlying cause of the poikilocytosis. In conditions where poikilocytosis is caused by iron deficiency anemia,[13] megaloblastic anemia due to low levels of iron, vitamin B12, or folate respectively is usually treated by taking supplements and increasing the levels of these vitamins in the diet and/or by treating the underlying disease (such as celiac disease or alcoholism) that have caused the deficiency.
Poikilocytocis due to inherited causes like thalassemia or sickle cell anemia may require treatment for a long duration, depending on their clinical variants (homozygous or heterozygous). These cases may require blood transfusions, or in some causes of poikilocytosis, bone marrow transplant may be required to treat their condition. People with other causes of poikilocytosis like liver disease (with target cells or acanthocytes) should be treated accordingly. Some may require a liver transplant, while patients with sepsis or serious infections (may have schistocytes) may need antibiotics.
Differential Diagnosis
Poikilocytosis should be differentiated from the following:
- Anisocytosis is the abnormal size of RBCs, including microcytic cells seen in iron deficiency anemia, and macrocytic cells seen in megaloblastic anemia.
- Howell Jolly bodies, which are RBCs with inclusions, are seen in conditions like asplenia.
- Anisochromia is variability in the color density of erythrocytes due to unequal hemoglobin, including hypochromic cells seen in iron deficiency anemia.
- Rouleaux are aggregations of RBCs seen when the erythrocyte sedimentation rate is increased in infections, cancers, and inflammatory conditions.
Prognosis
Prognosis depends on the cause of poikilocytosis. Some diseases like iron deficiency anemia and megaloblastic anemias have a good prognosis as the disease is resolved by correction of the underlying nutritional defect. However, some causes like sickle cell disease may have poor prognosis depending on presentation and complications, including infections, and vaso-occlusive crises and they require life long treatments.
Complications
Complications also depend on the cause of poikilocytosis. The following are some of the complications associated with common etiologies of poikilocytosis:
Sickle cell disease complications include:
- Infections
- Osteomyelitis
- Stroke, priapism
- Acute chest syndrome
- Hemolytic crisis
- Aplastic crisis
- Autosplenectomy, etc. seen in sickle cell disease[14]
Hereditary spherocytosis complications include:
- Folate deficiency
- Hemolysis
- Pigmented gall stones
- Aplastic crisis, etc.
Anemia complications include palpitations, heart failure, pregnancy complications, and delayed growth in infants and children.
Deterrence and Patient Education
Poikilocytosis is caused by another medical condition. The patients should be educated about the cause of their poikilocytosis, prognosis, and treatment options. Conditions like anemia caused by iron deficiency are treatable and have a very good prognosis, but can be dangerous if not managed properly. Anemia during pregnancy can cause complications, including serious birth defects such as neural tube defects caused by megaloblastic anemia due to folate deficiency. Other complications of anemia during pregnancy include preeclampsia, preterm birth, etc. Anemia caused by a genetic disorder such as sickle cell anemia and thalassemia will require lifelong treatment.
Pearls and Other Issues
- Poikilocytosis is a term for abnormal shaped red blood cells in the blood.
- Poikilocytosis refers to an increase in abnormal red blood cells of any shape that makes up to 10% or more of the total population. Poikilocytes can be flat, elongated, teardrop-shaped, crescent-shaped, sickle-shaped, or can have pointy or thorn-like projections, or may have other abnormal feature.
- Poikilocytosis can be due to inherited or acquired causes. Inherited conditions can be due to a genetic mutation. Acquired conditions usually develop later in life.
- The most common etiologies of poikilocytosis are sickle cell disease, thalassemia, hereditary spherocytosis, iron deficiency anemia, megaloblastic anemia, and liver disease.
- The most common types of poikilocytosis are sickle cells, target cell, spherocytes, elliptocytes, ovalocytes, echinocytes, and acanthocytes.
- They are usually identified on the blood smear and play an important role in diagnosing the underlying cause and its management.
- Treatment and prognosis vary depending on the cause of the poikilocytosis.
Enhancing Healthcare Team Outcomes
The outcome for poikilocytosis depends on the type of poikilocytosis and its cause and how quickly they are diagnosed and managed. It requires a well planned interprofessional approach with a primary clinician, a hematologist, a hematopathologist, a pharmacist, and a nurse, all working together as a health care team to bring the best outcome to the patients. The patients should be educated about the cause, prognosis, and different treatment options available. It is very important to identify and diagnose the condition early. Blood smear examination showing poikilocytosis helps in early identification of the cause and can guide the diagnosis and treatment.
(Click Image to Enlarge)
(Click Image to Enlarge)