Popliteal Artery Aneurysm
- Article Author:
- Mohammed Kassem
- Article Editor:
- Lorena Gonzalez
- Updated:
- 8/24/2020 9:05:06 AM
- For CME on this topic:
- Popliteal Artery Aneurysm CME
- PubMed Link:
- Popliteal Artery Aneurysm
Introduction
The popliteal artery is defined as aneurysmal when focal dilation in its diameter is more than 50% of the normal vessel diameter. The normal diameter of the popliteal artery varies from 0.7 to 1.1 cm. These focal dilations classify as fusiform (diffuse dilation) or saccular (asymmetrical). Popliteal artery aneurysms (PAAs) account for 85% of all peripheral aneurysms. Popliteal artery aneurysms are associated with abdominal aortic aneurysms 40% to 50% of the time.[1][2][3]
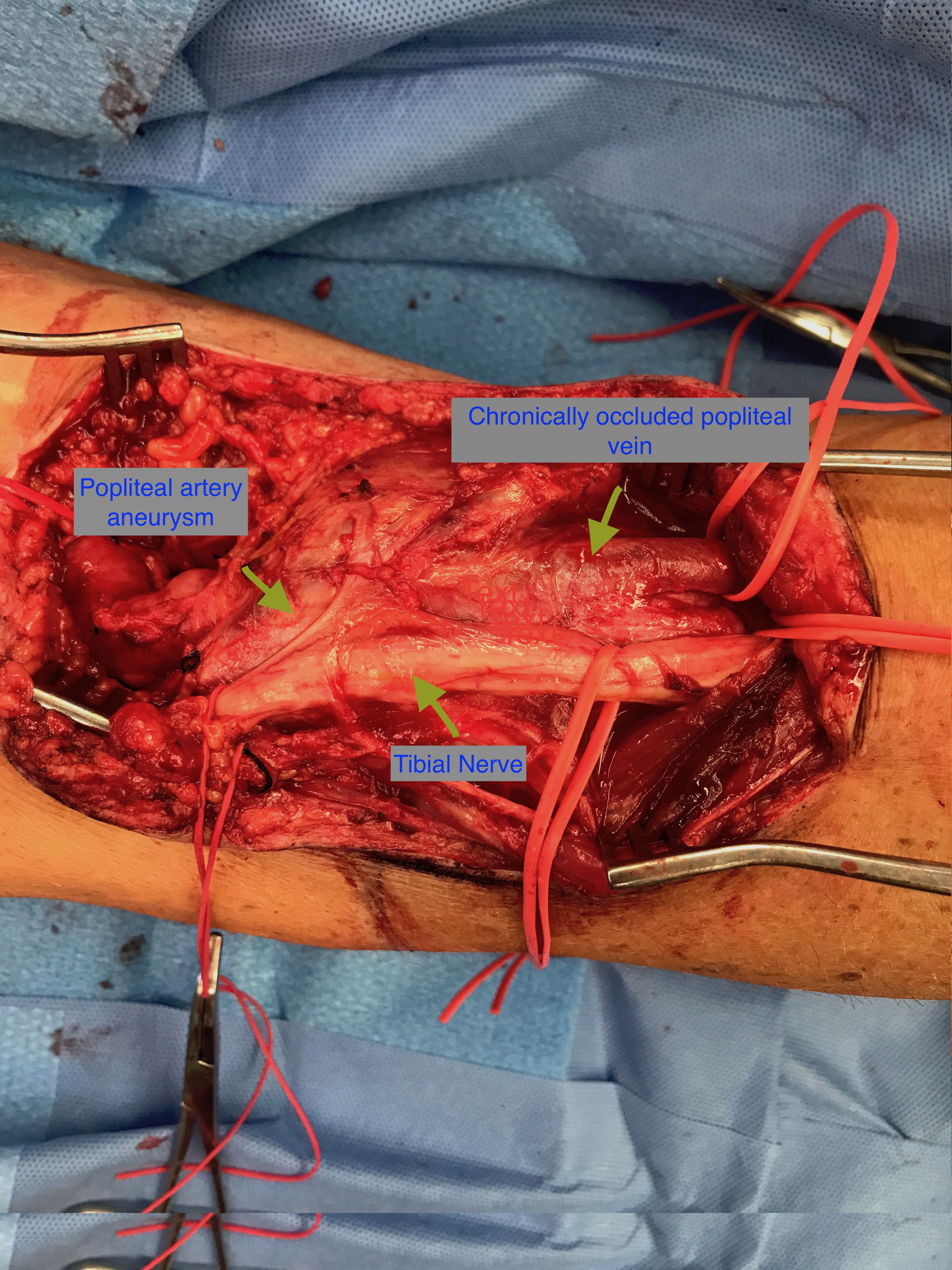
The popliteal artery is considered a continuation of the superficial femoral artery after it passes through the adductor magnus hiatus. It lies in the popliteal fossa accompanying its vein and terminates at the bifurcation into the anterior tibial artery and tibioperoneal trunk, which is located at the lower border of the popliteus muscle at the level of the tibial tuberosity.
Etiology
Epidemiology
The exact incidence of popliteal artery aneurysm is not known as no population-based study has been published; however, a few series studies issued by different institutions suggest that popliteal artery aneurysm prevalence increases with age and peaks in the sixth or seventh decades of life. The incidence of femoral and popliteal aneurysms in persons with abdominal aortic aneurysms (AAA) appears higher than the general population. In one study of 225 patients, 28% (n=63) had a popliteal artery aneurysm greater than or equal to 10.5 mm, 19% (n=43) had a popliteal artery aneurysm greater than or equal to 12mm and 11% (n=25) had a popliteal artery aneurysm greater than or equal to 15 mm.
Pathophysiology
The etiology of popliteal artery aneurysms, and aneurysms in general, is unknown. Molecular studies suggest that a combination of genetic defects and inflammatory processes may be responsible. Atherosclerosis tends to increase flow turbulence distal to a stenosis, leading to a pathological dilation of the artery. Decreased wall strength associated with inflammatory cell infiltration is believed to result in aneurysm formation.[5]
History and Physical
Most commonly, popliteal artery aneurysms are asymptomatic. If patients exhibit chronic symptoms, these are usually secondary to mass effect and compression of adjacent structures, such as the tibial nerve, which causes leg pain or paresthesias. The popliteal vein also may be compressed, which causes calf swelling. Progressive luminal narrowing of the popliteal artery from thrombus formation may cause an insidious onset of claudication. Approximately 50% of the patients present with bilateral aneurysms.
When an aneurysm acutely thromboses, the most common symptoms are acute lower extremity ischemia resulting in the acute onset of pain, paresthesias, paresis, pallor, and poikilothermia due to either aneurysmal intraluminal thrombosis or distal embolization of thrombus. Distal embolization can manifest as blue toe syndrome and/or acral cyanosis.
Approximately 30% of untreated patients experience acute thrombosis and distal embolization with the risk of possible limb loss. Patients who develop acute thrombosis or embolism have a relatively poor prognosis with a 15% amputation rate due to occlusion of runoff vessels.
The popliteal fossa should be examined bilaterally with the knee in a semi-flexed position. About 60% of patients with popliteal aneurysms have a palpable pulsatile mass at the level of the knee joint.
Evaluation
Duplex ultrasonography (US) is the ideal screening and diagnostic imaging modality to detect a popliteal artery aneurysm and estimate its diameter. The US also provides detailed information regarding vessel patency, development of mural thrombus, and the status of outflow vessels. CT or magnetic resonance (MR) angiography are other alternatives to duplex ultrasonography and can accurately measure true lumen diameters as well as assist in the planning of operative repair. Conventional angiography is reserved for either elective endovascular repair of an aneurysm or in cases of threatening acute limb ischemia for initiation of thrombolytic therapy.[6][7][8]
Treatment / Management
All symptomatic popliteal artery aneurysms require repair because of an increased incidence of thrombosis or limb loss. Asymptomatic aneurysms with a diameter greater than 2 cm are considered an indication for an elective operation to avoid complications such as limb-threatening ischemia. Greater than 45 angulation in asymptomatic aneurysms warrants surgical intervention because they can produce acute limb ischemia secondary to kinking of the vessel.[9][10][6]
Conservative Management
Asymptomatic aneurysms less than 2 cm are safely manageable via duplex surveillance.
Open Surgical Approach
Traditional open surgery involves ligation of the popliteal artery proximal (above the knee) and distal (below the knee) below the aneurysmal sac and bypassing the excluded segment using either reversed autologous vein graft (saphenous vein) or prosthetic graft. An alternative surgical approach is aneurysmectomy, followed by an interposition bypass with a prosthetic graft between the proximal and distal normal segments of the popliteal artery. However, the former method is more common.
Endovascular Approach
Recently, endovascular techniques have gained popularity in popliteal artery aneurysm, repair as an alternative to the open surgical approach. This technique excludes the aneurysmal sac with stent-graft implantation. Recent studies show that popliteal artery stenting is a safe alternative technique for the treatment of popliteal artery aneurysms, especially in high-risk patients. The advantages of endovascular technique include a shorter hospital stay and an abbreviated operative time when compared to open surgical intervention. Disadvantages include higher 30-day graft thrombosis rates (9% in the endovascular treatment group versus 2% in the open surgical treatment group) and higher 30-day re-intervention rates (9% in the endovascular treatment group versus 4% in the open surgical treatment group). There is no significant difference regarding the incidence of mortality or limb loss rates between the two repair groups.
Management of Acutely Thrombosed Aneurysms
Management of this will vary according to the presentation. Asymptomatic patients with completely thrombosed popliteal artery aneurysms and those who are non-ambulatory patients or have acutely thrombosed aneurysms with a poor runoff despite thrombolysis are not candidates for surgical intervention. Only patients with disabling symptoms or critical limb ischemia are treated with surgical bypass as the first line of therapy. Patients presenting with acute limb-threatening ischemia should receive urgent bypass. Acute thrombosis should be treated with intravenous heparin and continuous heparin infusion to limit the extension of thrombus. However, some surgeons advise that threatening ischemia is better treated with thrombectomy, followed by bypass surgery.
Intra-arterial Thrombolytic Therapy
This method is indicated when angiography demonstrates no target vessel, or there are multiple distal thrombi noted.
Differential Diagnosis
- Baker cyst
- Lymph node
- Varicosity
- Cystic adventitial disease
Complications
Limb loss
Pearls and Other Issues
The differential diagnosis of popliteal fossa masses includes both arterial and non-arterial pathologies as well as popliteal artery aneurysms. Rare popliteal artery pathology most commonly located in the behind the knee includes cystic adventitial disease and the popliteal entrapment syndrome. Both conditions usually present with chronic symptoms of claudication. However, the most common cause of a popliteal fossa mass is the Baker cyst, which is a benign swelling of the semimembranosus, or, more rarely, some other synovial bursa, found behind the knee joint. Orthopedic causes include prepatellar bursitis and meniscal cysts.
Enhancing Healthcare Team Outcomes
Popliteal artery aneurysms are usually managed by an interprofessional team of healthcare professionals that include a vascular surgeon, an interventional radiologist, an endocrinologist, an internist, and a critical care specialist. While elective management of these aneurysms yields good results, patients who present with a rupture, frequently end up losing their limb. Given the very high risk of losing a limb following the rupture of a popliteal artery aneurysm, patient education is vital. The nurse plays a vital role in monitoring and educating patients with a popliteal artery aneurysm. The patient must understand that once they receive a diagnosis of an aneurysm, they should follow up with a vascular surgeon and undergo elective surgery or have an endovascular procedure performed. More importantly, the patient must stop smoking, manage the high blood pressure, and control blood sugars; these are areas where the clinician can enlist the assistance of pharmacists. Finally, it is important to examine the patient for a popliteal artery aneurysm in the contralateral leg and abdomen. All patients with a pulsatile mass behind the knee should get referred to the radiologist for an ultrasound.[11][12][13] An interprofessional approach to diagnosis and management will yield superior outcomes and reduce morbidity. [Level 5]
Outcomes
For patients who have the popliteal artery aneurysm repaired electively, the prognosis is good. Outcomes with both surgery and an endovascular procedure appear to be similar in the short term. However, the long-term outcome of an endovascular procedure on the popliteal artery aneurysm remains unknown. In patients who present with rupture of a popliteal artery aneurysm, the outcome is usually poor. Limb loss is common. The amputations may be above or below the knee. The only way to reduce these poor outcomes and is by thoroughly examining the pulses in all patients.[14][15][16] [Level 3]