Anatomy, Back, Posterior Longitudinal Ligament
- Article Author:
- Vinayak Aryal
- Article Editor:
- Andreea Jimenez
- Updated:
- 8/14/2020 6:11:16 PM
- For CME on this topic:
- Anatomy, Back, Posterior Longitudinal Ligament CME
- PubMed Link:
- Anatomy, Back, Posterior Longitudinal Ligament
Introduction
The posterior longitudinal ligament is one of the three more important ligaments that contribute to stability in the spine. It runs along the posterior aspect of the vertebral body inside the vertebral canal from the body of the axis to the sacrum.[1] The ligament is composed of longitudinal fibers that are denser than the anterior longitudinal ligament. However, like the anterior longitudinal ligament, the denser fibers are deeper and span one vertebra while the superficial fibers span three to four. The superficial layer is a continuation of the tectorial membrane at the axis, and the deep layer is a continuation of the cruciform ligament at the atlas.[2]
The fibers are wider at the intervertebral spaces and are more adherent to the annulus fibrosus of the intervertebral discs than at the vertebral body where they are thinner. This phenomenon is more visible in the posterior ligament than the anterior. Therefore, the posterior longitudinal ligament is much thinner than the anterior longitudinal ligament, which is significant for the pathophysiology of disc herniations occurring posterolateral.[1]
Structure and Function
The PLL comprises superficial and deep connective tissue layers, which can generally be distinguished by their morphology and fiber arrangement. The superficial layer is the more posterior, with its distinction from the dura mater often being difficult to determine.[1] It consists of a central band of fibers 8 to 10 mm wide extending over several vertebral segments. Due to its broad attachment to the intervertebral disc, it has been described as being ‘‘fanlike’’, giving it a denticulate appearance over each vertebral body. This denticulate appearance becomes more apparent in the lower thoracic and lumbar regions, where the superficial layer is of more uniform width.[3]
Nevertheless, there is considerable morphological variation even within the lumbar region, where both the central fibers and the ‘‘fanlike’’ portion appear to decrease in width between L1 and L5.[4] The deep layer, which is adherent to the superficial layer in the midline, is of more uniform diameter throughout its length, being 2 to 3 mm wide at its narrowest point.[5] It also has a denticulate appearance.
In the cervical region, the PLL is a wide bandlike structure of similar width over both the intervertebral disc and vertebral body, however more inferiorly, it becomes increasingly denticulate, with its widest part being over the IVD. The separate fibers of the superficial and deep layers were difficult to identify at the level of the IVD, but their attachment to the margins of the vertebral bodies and intervening annulus fibrosus was clear.[6]
The fibers of each layer appeared to merge, forming a common attachment. Both superficial and deep layers attached to a midline bony septum on the posterior surface of the vertebral body between the superior and inferior margins. This attachment was not always continuous because of deficiencies in the septum in the central third of the vertebral body. The orientation of fibers within the PLL was consistent at all levels, with those in the central portion of the superficial layer being more vertical than those of the ‘‘fanlike’’ portion. Although the deep layer was visible through the superficial layer, its fiber orientation could not be established.[1]
The posterior longitudinal ligament has a more protective than a supportive role. The observed pattern of migrations of foreign materials like masses and bony fragments following a vertebral fracture into the vertebral canal confirm that PLL acts to protect the spinal cord and from displaced disc material.[5]
Fibers of the superficial layer will limit forward flexion, while the oblique fibers of the deep layer will limit lateral flexion and rotation. However, research has suggested that fibers from both layers are involved in all movements, with an increasing number of fibers recruited with increasing load.[2] The more denticulate appearance of the PLL in the lower thoracic and lumbar regions may be due to the increased rotational and lateral flexion forces generated in the lower region compared with the upper regions of the vertebral column. The presence of elastin in the PLL supports the idea that it has a role in the dynamic motion of the spine.[7] Observed patterns of disc fragment migration following vertebral burst fractures suggest that the PLL also protects the contents of the vertebral canal.[8]
Embryology
During the first six weeks of gestation, the vertebral column consists of a light zone and a dark zone. A hypocellular light zone represents the vertebral body, and a hypercellular dark zone represents the intervertebral disk.[9] At seven weeks, the light zone and dark zone become distinct, but the ligament is unclear. During the eighth week, the longitudinal arrangement of cells and collagen fibers appear at the location of the adult anterior longitudinal ligament.[10]
On the other hand, no longitudinal cell arrangement is identifiable at the location of the posterior longitudinal ligament. At ten weeks, the dark zone decrease in width, and the origin of the posterior longitudinal ligament appears. It is unclear at the level of the vertebral body and but clear at the level of the disc.[9]
Blood Supply and Lymphatics
The primary source of blood supply to the spinal cord is from a single anterior spinal artery and the two posterior spinal arteries. These two arteries are the branches of the vertebral artery. Posterior arteries supply the posterior part of the spinal cord, and the anterior portion receives supply by the anterior spinal artery.[11] Besides these arteries, there are other arteries at each spinal segment called radicular spinal arteries, which derive from the body wall arteries. The small penetrating arteries given off by both anterior and posterior spinal arteries form anastomose in the spinal cord.
The radicular spinal arteries supply the dorsal and ventral part of the spinal cord. The drainage of blood from the spinal cord takes place with the help of anterior and posterior spinal veins. These veins drain into internal and external venous plexus. Through these plexus, the blood drains into the main venous system with the help of azygous veins, lumbar veins, and hemizygous veins.[12]
Nerves
The primary source of innervation of the posterior longitudinal ligament is the meningeal branch derived from the spinal nerve. It gives ascending and descending branches in the vertebral column.[13] There are transverse branches formed by the fusion of ascending and descending branches. The fusion of the transverse branches from the opposite side forms a network of nerve fibers superficially, which innervates the posterior longitudinal ligament in the vertebral segment. The posterior part of the annulus fibrosus is traversed by the nerve fibers forming a network deep in the intervertebral part of the posterior longitudinal ligament.[14]
There is no innervation of the deep layer of the nucleus pulposus or annulus fibrosus because they lack nerve fibers and nerve terminals. Few nerve terminals are present in the central part of the nucleus pulposus, but in the peripheral zone, there are abundant nerve fibers. These nerve fibers in the peripheral zone play an important role in the regulation of movement and posture in the vertebral column.[13]
Muscles
There are three groups of muscle in the back; superficial, intermediate, and the deep muscle layers. The superficial layer consists of two muscles; splenius cervicis and splenius capitis. They play an important role in the extension of the neck and the movement of the shoulder.
The intermediate muscle group contains longissimus, iliocostalis, and spinalis muscles. All three muscles of the intermediate group have the same tendinous origin. These groups of muscle help in the flexion of the head and upper vertebral column and the movement of the thoracic cage. The deep layer consists of semispinalis, rotatores, and multifidus. The main function of this muscle group is the stabilization of the vertebral column and maintaining the posture. They also help in balance and proprioception.[15]
Physiologic Variants
In comparison to the anterior longitudinal ligament, the posterior longitudinal ligament is narrower and weaker. It has an oval structure that varies from 2 to 2.25 mm in width at the level of L5-S1. From L5 upwards, the ligament forms a narrow band, which widens symmetrically at the level of each disc. The fibers of the annulus fibrosus and the edge of the vertebral body are the sites of attachment of the ligament, but in some cases, not all, it is attached to the posterior aspect of the vertebra. The widths of the ligament at the different levels are as follows.[13]
L5 1.4 cm, L3 1.5 " L2 1.1" L5 0.7 cm, vertebral body level L3 0.8 L2 0.6 "
The thickness of the ligaments at different levels are as follows:
L5 1.3 mm L3 1.4 " L2 0.9 "
The posterior longitudinal ligament seems to be most developed at the level of L3 and L4, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker middle portion approximately about 2.5-4 mm in width throughout the whole length of the ligament. The ligament in the mid-portion of each vertebral body covers the vascular foramina.[5]
Surgical Considerations
The pharmacologic management of the ossification of the longitudinal ligament is still not established. Standard treatment is surgical decompression of the spinal cord. The surgical management is done either by anterior decompression or by posterior decompression in modern medical practices.[16] In the anterior surgical decompression, the ossified lesion is removed from the anterior side of the spine. Technically, this surgical procedure is difficult because of the anterior location of the posterior longitudinal ligament in the vertebral canal. Thus, the posterior decompression is the choice of surgical procedure in the treatment of the ossification of the posterior longitudinal ligament. Although it is the surgical procedure of choice, there are chances of complications, and the poor surgical outcomes are due to the following reasons.[17]
- Physiological kyphosis in the thoracic region
- The thoracic region of the spinal cord is the watershed region, which predisposes to ischemic change.
Even after the surgical treatment, there may be chances of re-progression of ossification. So for young patients without any neurological deficits, strict radiological follow up is recommended. For those with progressive deficits, surgery is the only way of treatment.[16]
Clinical Significance
Ossification of the posterior longitudinal ligament is an ectopic calcification in the tissue of the spinal ligament. About 70% of the cases OPLL developed in the cervical spine, but it may be seen in the thoracic and lumbar spine as well. Predominantly, it occurs in males than in females. The symptoms commonly present in the 40s and 50s.[16]
Clinical Presentation [17]
- Mild pain and discomfort in the early stage
- Clumsiness, dysesthesia, and tingling sensation in hands
- Lower extremity symptoms like gait disturbances may appear as the disease progresses, and suddenly or even quadriplegia may appear by mild injuries.
Pathogenesis
- The cause of the ossification of the posterior longitudinal ligament is still unknown. It is said to be a multifactorial disease. The genetic and non-genetic factors such as diet, obesity, age, diabetes mellitus, physical strain on the posterior longitudinal ligament play an important role in the development of the disease.[18]
- Hypertrophic changes in the ligament itself are said to be one of the mechanisms of ossification of the posterior longitudinal ligament.[19]
Diagnosis
A diagnosis of ossification of the posterior longitudinal ligament is based on radiological findings and clinical presentation. Since plain radiological exams have limitations, a CT scan or MRI is useful in the diagnosis. CT scan shows the accurate shape and size of the ossified mass and also helps to classify the type of OPLL. Three dimensional CT is sometimes used to quantify the volume of OPLL. MRI is used to detect the compression from OPLL and also helps to detect the extent of spinal cord compression.[20]
Other Issues
The displacement of the nucleus pulposus of the intervertebral disc into the dural sac is termed as intradural disc herniation.[21] An intradural herniation is the rare, occurring pathology that mostly occurs in the lumbar spine (92%), about 5% in the thoracic spine, and about 3% in the cervical region. The exact cause of intradural herniation is still unknown, but the calcification of the posterior spinal longitudinal ligament is said to be the most likely cause of the herniation.[22]
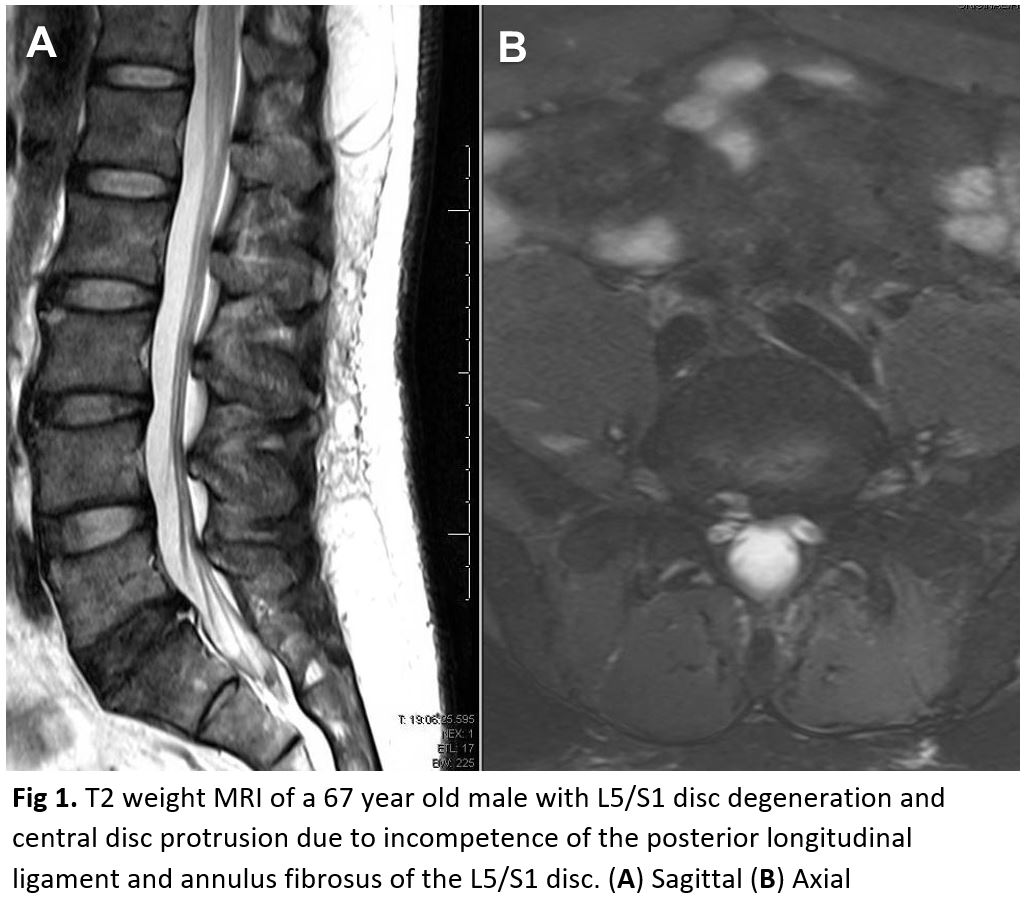
(Click Image to Enlarge)
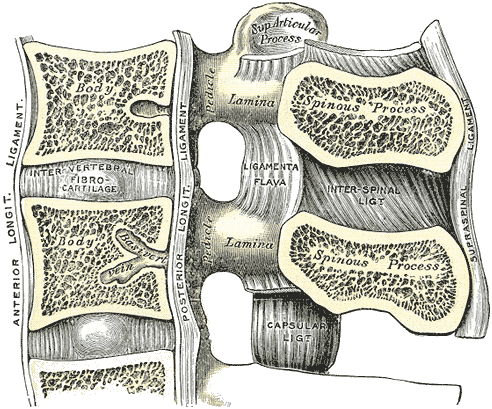
Vertebrae, Lumbar, Ligament, Medial Sagittal Section, Anterior Longitudinal Ligament, Inter vertebral Fibrocartilage, Posterior Longitudinal Ligament, Lamina, Ligamenta Flava, Pedicle, Spinous Process, Interspinal Ligament, Capsular ligament, Supraspinal Ligament,
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)
(Click Image to Enlarge)