Prurigo Nodularis
- Article Author:
- Tessa Mullins
- Article Author:
- Poonam Sharma
- Article Author:
- Christopher Riley
- Article Editor:
- Sidharth Sonthalia
- Updated:
- 9/15/2020 7:41:32 PM
- For CME on this topic:
- Prurigo Nodularis CME
- PubMed Link:
- Prurigo Nodularis
Introduction
Prurigo nodularis (PN) is a chronic disorder of the skin that is classically seen as multiple, firm, flesh to pink colored nodules commonly located on the extensor surfaces of the extremities. The lesions are very pruritic and the condition may occur in any age group. It is commonly associated with another disorder of cutaneous hypersensitivity such as atopic dermatitis or chronic pruritus of diverse origins. The diagnosis is mainly clinical; although certain conditions may simulate it clinically warranting differentiation. The condition is associated with significant physical and psychological morbidity and often refractory to treatments. A whole range of general measures, pharmacological approaches and psychological therapies may be needed in a patient with advanced PN. [1][2][3][4]
Etiology
The exact etiology of prurigo nodularis remains poorly understood. Although the role of unimpeded itch-scratch cycle is uncontested, the exact sequence of events leading to the final clinical picture remain conjectural. Prurigo nodularis is accompanied by long-standing pruritus and thought to develop as a reaction to repeated scratching in patients with chronic prurigo of various etiologies including dermatological, systemic, infectious, and neuropsychiatric[5][6].
Anecdotal data suggests causative role or association of infectious agents such as hepatitis C, Helicobacter pylori, Strongyloides stercoralis, mycobacteria and HIV in PN [7] [8].
Increase in the number of sensory structures of the epidermis (merkel cells) and dermis (papillary dermal nerves) is encountered in PN lesions [9]. This neural alteration is typical of PN and not seen in lichen simplex chronicus or neurodermatitis.
The density of mast cells and neutrophils is increased in PN although there seems to be no increase in their degranulation products. In contrast while the number of eosinophils remains maintained, their products such as the major basic protein and eosinophil-derived neurotoxin show higher than normal levels.
The pruritus in PN seems to be a result of cutaneous neurogenic inflammation mediated by various neuropeptides especially substance P, calcitonin gene–related peptide (CGRP) [10], and vanilloid receptor subtype 1 (VR-1). The latter binds to capsaicin, rendering it a potential therapeutic topical agent.
Individuals with PN also show elevated levels of Interleukin 31(IL-31), a T-cell–derived highly prurigogenic cytokine [11].
Epidemiology
The exact incidence of PN is not known. A majority of patients with PN present between the ages of 51 and 65 years, although several cases in other age groups have also been described [5][12]. While the disease afflicts both genders, it seems to be more frequent and more intense in females[13]. Multiple studies have shown that individuals with an atopic predisposition have an earlier age of onset[5][14][15]. Ethnicity and genetic predisposition seem to play a role since individuals belonging to the African-American ethnic group are 3.4 times more likely to have prurigo nodularis than white patients[12]. Other conditions that have been reported to induce prurigo nodularis include internal malignancy, renal failure, and psychiatric conditions. In HIV positive patients, PN has been reported to be predictive of advanced immunosuppression[16].
Pathophysiology
The pathophysiology of PN has been controversial [vide supra]. Chronic and/or recurrent mechanical trauma or vigorous frictional assault to the skin induced epidermal hyperplasia with resultant thickening of the skin. Repetitive mechanical rubbing/scratching not only result in the formation of plaques and nodules, often with lichenification; but also give rise to dyschromic changes, typically hyperpigmentation. The itching of PN is typically episodic, severe, and uncontrollable and tends to occur at discrete points that eventually transform into hyperpigmented noduloplaques with excoriations, crusting and sometimes secondary bacterial infection.
Immunohistochemical studies have shown an increased number of dermal nerve fibres in the papillary dermis. It has been postulated that the thin, unmyelinated epidermal nerves are the transmitters of the severe prurigo. Nerve growth factor (NGF) and its receptor, tyrosine receptor kinase A (TrkA), are overexpressed in PN lesions. They may also be associated with the increased release and accumulation of neuropeptides, such as substance P and calcitonin gene-related peptide [17]. Interestingly, skin biopsies taken from lesions of PN tend to show significantly decreased intraepidermal (not dermal) nerve fiber density. Although this finding raised the doubt of some subclinical small nerve fibre neuropathy contributing to the pathophysiology, recent studies have suggested that this reduction may actually be secondary to chronic scratching. This was confirmed on observing restoration of the intraepidermal nerve fiber density on complete healing of lesions [18].
The role of helper T cytokines, T helper 1 and T helper 2, have also been studied in the pathogenesis of prurigo nodularis using the signal transducers and activators of transcription (STAT) 1, 3, and 6. In every case examined but three, the entire epidermis stained with anti-pSTAT 6, a marker for the Th2 cytokines interleukin (IL)-4, IL-5, and IL-13. These findings suggest that Th2 cytokines play a principal role in the pathogenesis of prurigo nodularis.[19]
Histopathology
Lesions of prurigo nodularis under histopathology can show thick, orthohyperkeratosis, irregular epidermal hyperplasia, and pseudoepitheliomatous hyperplasia. Focal parakeratosis with irregular acanthosis diminished nerve fiber density and a nonspecific dermal infiltrate containing lymphocytes, macrophages, eosinophils, and neutrophils may also be seen on histology for prurigo nodularis lesions. Histology can play an important role in diagnosing prurigo nodularis vs. lichen simplex and hypertrophic lichen planus. Lesions of lichen simplex are less likely to have pseudoepitheliomatous hyperplasia or nerve fiber thickening; however, it does not rule out the histological diagnosis of PN. It is necessary to correlate clinical and histological findings together to reliably distinguish between PN and LS[20]. HLP and PN both demonstrate epidermal hyperplasia, hypergranulosis, and compact hyperkeratosis. Vertically arranged collagen fibers and an increased number of fibroblasts and capillaries in the dermis are found in both conditions. However, basal cell degeneration is limited to the tips of rete ridges, and no band-like inflammation will be seen in HLP vs. PN[21]
History and Physical
Patients with prurigo nodularis present with a characteristic firm, dome-shaped, pruritic nodules that vary in size from a few millimeters to centimeters. The nodules can be flesh-colored, erythematous, pink, and brown/black. Initially, the lesions can begin as normal skin or areas of xerosis. Due to pruritus, the patients will begin and continue to scratch the lesions until the dome-shaped nodule forms. Typically, the lesions are found symmetrically on the patient’s extensor surfaces of the arm and legs[22]. Lesions can also be found in the occipital region of the scalp. The upper back, abdomen, and sacrum also can be involved. Usually, areas that are difficult to reach such as the upper mid-back are spared. This finding is called the “butterfly sign.” The palms, soles, face, and flexural areas are usually spared. There is associated with severe pruritus that can be very distressing for the patients with prurigo nodularis. It can be sporadic or continuous and can increase with sweating, clothing irritation, or heat. Patients experience a combination of pruritic sensations including burning, stinging, and alterations in lesional temperature.[5] It has been reported that in some cases, atopic dermatitis and xerosis are found in conjunction with prurigo nodularis and may be the initiating factor. Lesions can often appear excoriated due to the pruritus involved with PN. Excoriated lesions are at increased risk of secondary infection and can appear crusted, erythematous or painful if infected. Prurigo nodularis can also be localized in the setting of an underlying local dermatosis such as venous stasis, postherpetic neuralgia, or brachioradial pruritus. [23]
Evaluation
Prurigo nodularis is a clinical diagnosis. Prurigo nodularis patients will likely have a history of chronic severe pruritus with excoriations and flesh-colored, pink nodular lesions on extensor surfaces. Dermoscopy can be a helpful tool when diagnosing PN vs. HLP. In one study, dermoscopy of HLP demonstrated pearly white areas and peripheral striations, gray-blue globules comedo-like openings, red dots and globules, brownish-black globules and yellowish structures. In PN, red dots and globules and pearly white areas with peripheral striations were observed under dermoscopy[24]. A skin biopsy may be warranted for lesions that are bleeding, have formed ulcers or are resistant to first-line therapies. If patients with prurigo nodularis and severe pruritus do not have a cause of the pruritus, causes of chronic pruritus should be evaluated. Causes of severe pruritus can include renal disease, liver disease, thyroid disease, HIV infection, malignancy or parasitic infection[25]. Evaluation of these causes includes a complete blood cell count (CBC), complete metabolic panel, thyroid studies including TSH and free T4, urinalysis, stool exam, HIV antibodies, and chest x-ray. Serum IgE levels can also be elevated in patients with PN and atopic dermatitis[26].
Treatment / Management
Management of prurigo nodularis requires a multifaceted approach. Patients need to be educated on practices to reduce scratching of lesions, assurance and diagnosing of underlying causes of pruritus and diagnosis and treatment of any psychological disorder associated with scratching and picking at skin. Treatments, both topical and systemic, are targeted at disrupting the itch-scratch cycle.
GENERAL CARE
- Patients are encouraged to keep their nails short, wear protective clothing such as long sleeves and gloves, and to keep the nodules covered with bandages.
- Using gentle cleansers to bathe and applying emollients multiple times a day to keep skin moisturized should be encouraged.
- Calamine lotions and lotions containing menthol and camphor can provide relief from the pruritus.
- Stay in a cool comfortable environment.
- Reduce stress.
SPECIFIC CARE
TOPICAL AND INTRALESIONAL THERAPY
- Although none have been examined in randomized trials, topical treatments for prurigo nodularis include class one topical corticosteroids, intralesional corticosteroids, topical calcineurin inhibitors, topical capsaicin, and topical vitamin D analogs.
- First-line therapy is suggested to be topical corticosteroids, such as clobetasol dipropionate 0.05% ointment applied under occlusion with plastic wrap once at nighttime for at least two to four weeks.
- Triamcinolone acetonide in concentrations of 10 mg/mL to 20 mg/mL injected intralesionally has been shown to flatten lesions and provide relief from pruritus. [27][28][29][30][31]
- Pimecrolimus 1% is as effective as hydrocortisone and can be implemented in a long-term regimen.[32]
- Calcipotriol ointment shows greater efficacy as compared to betamethasone valerate 0.1%.[33]
- The menthol in low concentration ( less than 5% ) alleviates pruritus by heightening the threshold for pruritic stimuli.[34]
ANTIHISTAMINES AND LEUKOTRINE INHIBITORS
- High dose non sedating antihistamines for daytime followed by First-generation sedating antihistamines at bedtime. A combination of fexofenadine and montelukast gives good results.[35]Common adverse reactions to antihistamines are drowsiness, dizziness, and weakness.
PHOTOTHERAPY/EXCIMER
- Phototherapy with PUVA, including bath/topical PUVA, long-wavelength ultraviolet A, narrowband ultraviolet B, and monochromatic excimer light of 308 nm, have been used and shown improvement of prurigo nodularis nodules in patients.
- Narrow Band UVB phototherapy results in significant improvement in prurigo nodularis at an average dose of 23.88- 26.00 j/cm2.[36]
- An excimer laser is more beneficial than topical clobetasol.[37]
ORAL IMMUNOSUPPRESSIVES
- As with topical therapies, no randomized trials have been reported involving the use of these systemic therapies and the benefits versus risks of the drugs must be considered before beginning treatment[13]
- Oral immunosuppressive therapy should be considered for patients with severe, recalcitrant prurigo nodularis.
- A single-institution retrospective study demonstrated clinical improvement and a decrease in pruritus with Cyclosporine at a mean dose of 3.1 mg/kg dose.[38]
- Methotrexate in a dose of 5-20mg/kg weekly demonstrated complete or partial remission of 2.4 months. These patients showed a mean duration of response of 19 months.[39]
- Treatment with azathioprine and cyclophosphamide has also been reported to be successful.[40][41]
- Oral tacrolimus therapy dramatically reduced pruritus in a patient who was previously treated with cyclosporine for prurigo nodularis.[42]
- Combination therapy of three cycles of intravenous immunoglobulin followed by methotrexate and topical steroid was effective in prurigo nodularis associated with atopic dermatitis.[43]
NOVEL TREATMENTS
- Thalidomide and Lenalidomide. Thalidomide is an immunomodulatory agent, which also acts as a central and peripheral depressant, and inhibits tumor necrosis factor-alpha.[43] The therapeutic effect against prurigo nodularis is thought to derive from its neurotoxic effects.[44] Lenalidomide, a more potent molecular form of thalidomide, is effective in prurigo nodularis and has a lower frequency of peripheral neuropathy.[45]
- Both selective serotonin reuptake inhibitors and tricyclic antidepressants can also be considered for chronic pruritus. It is important for patients to also be seen in conjunction with mental health professionals.
- Naloxone and naltrexone exert antipruritic effect through inhibition of Mu-opioid receptors on nociceptive neurons and interneurons resulting in suppression of itch.[46]
- NK1r antagonists, aprepitant and serlopitant, could prevent substance P mediated signaling in the pathogenesis of prurigo nodularis[47]. Significant relief of itch was achieved in prurigo nodularis patients on aprepitant monotherapy.
- IL 31 receptor antibody, Nemolizumab, provided significant improvement in pruritus scores in patients with moderate to severe atopic dermatitis. However, its role in prurigo nodularis remains unclear.
Differential Diagnosis
- Lichen simplex chronicus
- Hypertrophic lichen planus
- Pemphigoid nodularis
- Nodular scabies
- Keloids
- Dermatofibroma
- Foreign body reactions
Treatment Planning
Treatment of prurigo nodularis should be tailored to the patient's age, comorbidities, the severity of prurigo, quality of life and expected side effects.
First Line
- Class 1 topical steroids ( Clobetasol propionate 0.05%, halobetasol propionate 0.05%) Long term applications can lead to adverse effects like skin atrophy, folliculitis, miliaria, delayed wound healing, tachyphylaxis.
- Intralesional injections of triamcinolone acetonide (40mg/ml). This may be accompanied by cryotherapy.[48][49]
- Topical menthol solution in a concentration of less than 5%.
- Systemic antihistamines: fexofenadine 180mg, levocetirizine 5mg or desloratadine 5mg during daytime and sedating antihistamines like hydroxizine25mg at night time. The first generation antihistamines cause side effects like sedation, hyperexcitability, impaired cognitive function, dry mouth, constipation, dysuria, tachycardia, and arrhythmias.
Second-line
- Phototherapy: PUVA, long-wavelength UVA, Narrowband UVB, monochromatic excimer light of 308nm
- Systemic immunosuppressives: Cyclosporine 3mg/kg daily. Adverse effects include nephrotoxicity, hypertension, hyperlipidemia, hyperkalemia, hyperuricemia. Methotrexate 5-20mg/week. Common adverse effects are nausea, gastrointestinal symptoms, and transaminitis.
- Thalidomide 300-400 mg daily yields good response within 3 months, followed by tapering the dose to 50mg daily. However, complete cessation of the drug leads to recurrences. Adverse effects are teratogenicity and peripheral neuropathy. Lenalidomide 5-10mg daily is less neurotoxic than thalidomide.
- Opioid receptor antagonists : Naltrexone 50mg daily. Adverse effects are restricted to the first 2 weeks of treatment and include nausea, fatigue, dizziness, heartburn, and diarrhea.
Prognosis
Prurigo nodularis is a benign condition with a good prognosis. It is a chronic condition, typically preceded by an underlying cause of pruritus. However, prurigo nodularis is a distinct entity from these underlying causes and can persist despite the resolution of the predisposing condition.
Complications
Lesions of prurigo nodularis can become secondarily infected due to scratching of the lesions. It is important to monitor for clinical signs of infection such as erythema, pain, warmth and fever. If secondary infection is suspected, it is important to begin appropriate topical or systemic antibiotic therapy to cover for skin flora.
Deterrence and Patient Education
The deterrents in prurigo nodularis treatment are the severe intensity of the itch which can lead to psychological distress, chronic nature of the condition, the long duration of the therapy and the potential side effects of the medication.
Discussion with the patient should include advantages and disadvantages of the therapy, side effects and possible use of off-label medications. Patient education can thus promote treatment adherence. The potential length of therapy should also be discussed as prurigo nodularis is difficult to treat and the patient may become frustrated with lack of improvement.
Pearls and Other Issues
Prurigo nodularis is a chronic skin disease that can cause a significant impact on a patients quality of life. Breaking the itch-scratch cycle requires a multifaceted approach and patients should be encouraged to continue with therapy to reduce scratching and picking at the lesions. It may be necessary to involve behavioral therapy if required. It is important to explain to patients that prurigo nodularis lesions may be chronic and very difficult to improve completely.
Enhancing Healthcare Team Outcomes
Management of prurigo nodularis requires an interprofessional team that includes the primary caregiver, nurse practitioner, dermatologist, and a mental health nurse. Patients need to be educated on practices to reduce scratching of lesions, assurance and diagnosing of underlying causes of pruritus and diagnosis and treatment of any psychological disorder associated with scratching and picking at skin. Treatments, both topical and systemic, are targeted at disrupting the itch-scratch cycle. Patients are encouraged to keep their nails short, wear protective clothing such as long sleeves and gloves, and to keep the nodules covered with bandages. Using gentle cleansers to bathe and applying emollients multiple times a day to keep skin moisturized should be encouraged. Calamine lotions and lotions containing menthol and camphor-like Sarna can provide relief from the pruritus. First-generation sedating antihistamines such as hydroxyzine administered at bedtime may be useful in controlling nocturnal pruritus. Both selective serotonin reuptake inhibitors and tricyclic antidepressants can also be considered for chronic pruritus. [12]
Finally, the pharmacist should educate the patient on potential adverse reactions of the medications and report back to the clinical team if there are complications.
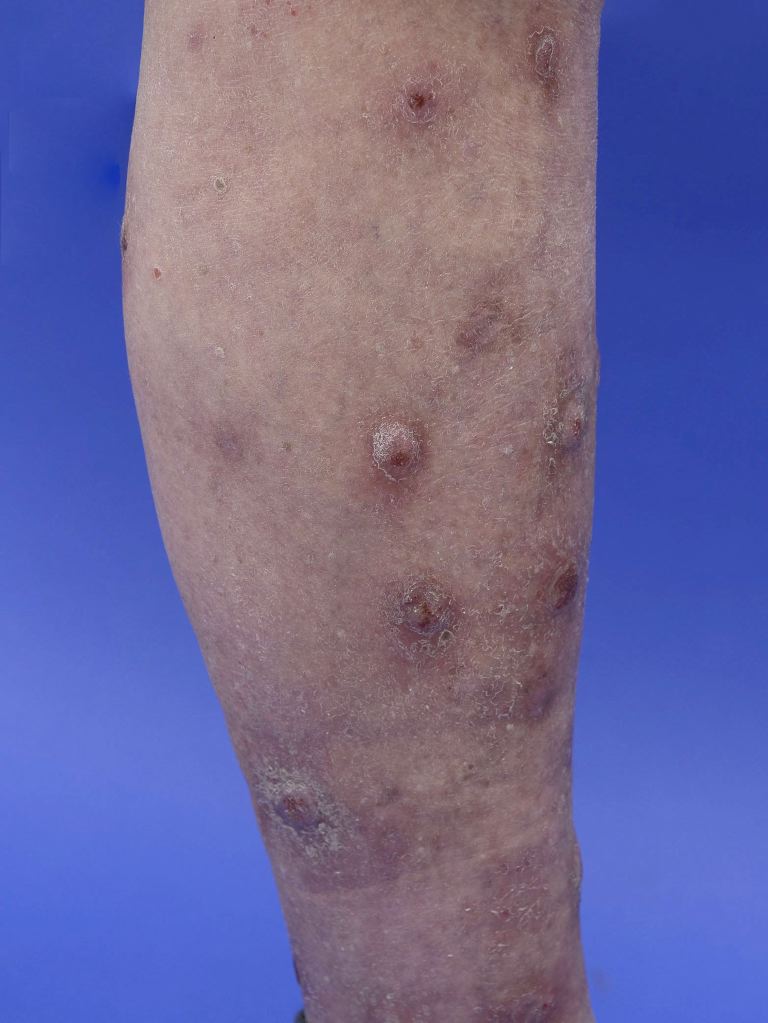
(Click Image to Enlarge)
![Figure 1 PRURIGO NODULARIS involving the limbs of a 65-year old lady: A, Clinical Image showing the typical hyperpigmented papules and nodules over the right upper extremity with excoriations; B, Polarized dermoscopic image from a papule showing an irregularly-shaped large reddish-brown clod with localized white structureless area (white arc), with interspersed red and brown colored dots and pigmented granules [Escope, USB Videodermoscope, 30X; Timpac Healthcare Pvt. Ltd., New Delhi]; and C, On histopathology from a nodule the epidermis is showing marked compact orthokeratosis, thickened granular layer, and irregular epidermal hyperplasia. The papillary dermis is thickened with papillomatosis and thickened bundles of collagen in vertical array, with increased number of thick walled capillaries and sparse superficial perivascular lymphocytic infiltrate [Hematoxylin & eosin, 400X]](../pictures/11160.jpg)
Figure 1 PRURIGO NODULARIS involving the limbs of a 65-year old lady: A, Clinical Image showing the typical hyperpigmented papules and nodules over the right upper extremity with excoriations; B, Polarized dermoscopic image from a papule showing an irregularly-shaped large reddish-brown clod with localized white structureless area (white arc), with interspersed red and brown colored dots and pigmented granules [Escope, USB Videodermoscope, 30X; Timpac Healthcare Pvt. Ltd., New Delhi]; and C, On histopathology from a nodule the epidermis is showing marked compact orthokeratosis, thickened granular layer, and irregular epidermal hyperplasia. The papillary dermis is thickened with papillomatosis and thickened bundles of collagen in vertical array, with increased number of thick walled capillaries and sparse superficial perivascular lymphocytic infiltrate [Hematoxylin & eosin, 400X]
Contributed by Dr Sidharth Sonthalia, MD, DNB, MNAMS