Pudendal Nerve Block
- Article Author:
- Shirin Ghanavatian
- Article Editor:
- Armen Derian
- Updated:
- 7/31/2020 2:27:11 PM
- For CME on this topic:
- Pudendal Nerve Block CME
- PubMed Link:
- Pudendal Nerve Block
Introduction
Pudendal nerve block (PNB) is the method of choice utilized for diagnosis and management of chronic pelvic pain caused by pudendal neuralgia, commonly due to pudendal nerve entrapment. Additionally, a pudendal nerve block is a widely used regional anesthesia technique performed for gynecology, obstetrics, and anorectal procedures.
Anatomy and Physiology
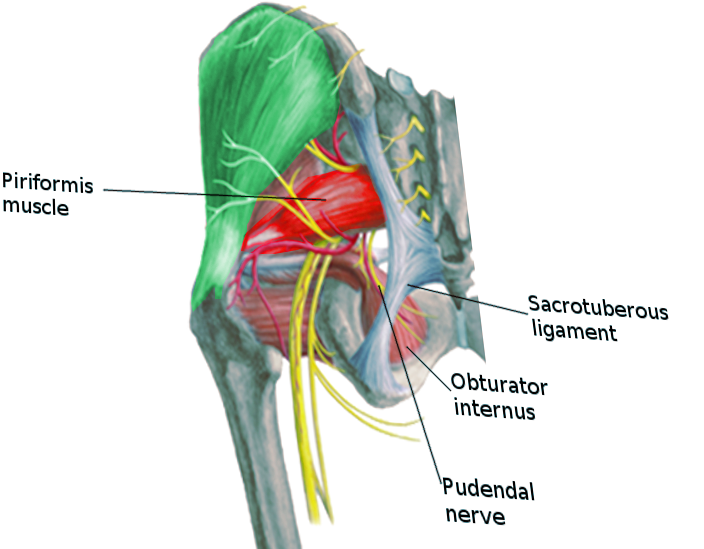
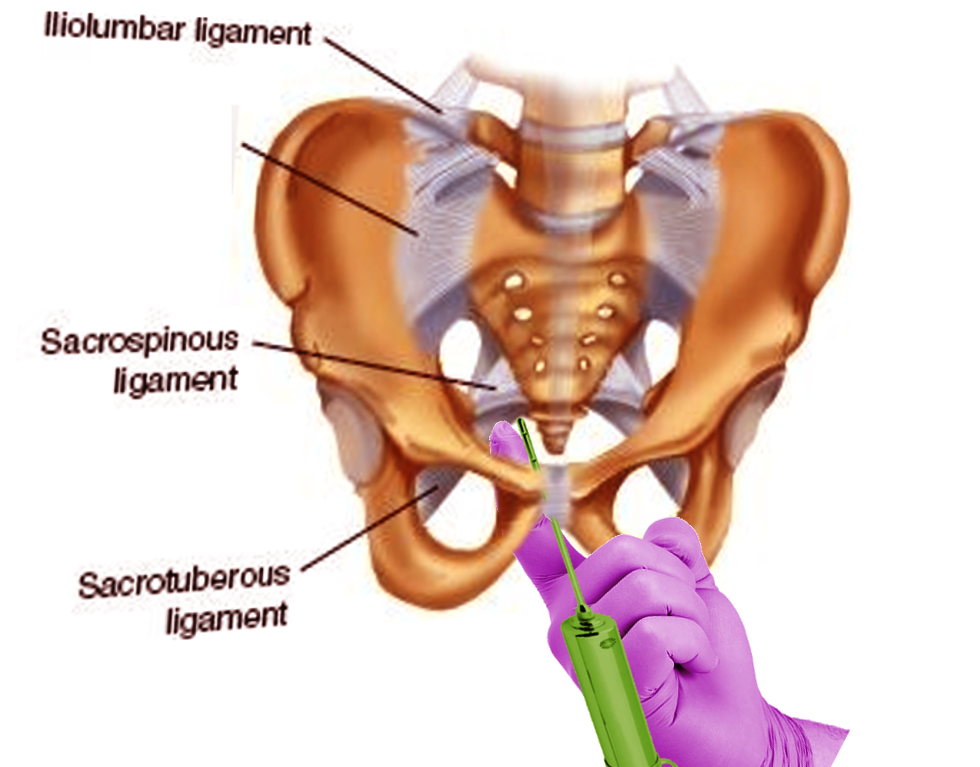
The pudendal nerve is a sensory and motor nerve arising from the sacral plexus and forms from spinal nerve roots S2-S4. The pudendal nerve passes through the greater sciatic foramen, where it transverses through the sacrospinous and sacrotuberous ligaments. It then reenters the perineum through the lesser sciatic foramen and accompanies the internal pudendal artery and vein. The pudendal nerve courses through the ischiorectal fossa and then through Alcock’s canal, also known as the pudendal canal.[1] Inside the pudendal canal, the nerve initially divides into the inferior rectal nerve and then gives off the perineal nerve. Ultimately, the nerve continues as the dorsal nerve innervating penis and clitoris. The inferior rectal nerve innervates the external anal sphincter and the perianal skin. The perineal nerve innervates the bulbospongiosus, ischiocavernosus, and levator ani muscles and sends sensory branches to the skin of the labia majora and scrotum. The dorsal nerve branch is a sensory nerve ending supplying the skin of the clitoris and penis.
Indications
A pudendal nerve block is historically a common regional anesthesia technique to provide perineal anesthesia during obstetric procedures, including vaginal birth during the second stage of labor, vaginal repairs, and anorectal surgeries such as hemorrhoidectomies. PNB is less commonly utilized to provide anesthesia for urological procedures. However, the literature describes it as a safe and effective local analgesia for patients undergoing trans-rectal ultrasound-guided prostate biopsy, transurethral prostatectomy, and for patients with catheter-related bladder discomfort.[1][2]
Pudendal nerve blocks are also being used to comfort the pain associated with pudendal neuralgia. Patients describe the pain as a burning sensation and hyperalgesia in the external genital and perineal region. It is related to urinary urgency, constipation, and sexual dysfunction.[3] The etiology for pudendal neuralgia is multifactorial and it can be caused by a traumatic insult to the nerve such as a fracture of the ischial spine,[4] compression along with its distribution, infectious agents such as herpes simplex,[5] mechanical insult such as chronic constipation,[6] tumors, and endometriosis[7] as well as iatrogenic damage. The most common injury to the pudendal nerve is reported to be obstetrical.[8] The majority of pudendal neuralgia is unilateral; however, there are reports of bilateral neuralgia in bicyclists.[9] A pudendal nerve block is performed to diagnose pudendal neuralgia as the cause of chronic pelvic pain and is also performed for long-term pain control if the test block is positive.
Contraindications
Allergic reaction to the local anesthetic used, skin, and soft tissue infections at the site of injection are absolute contraindications to undergo pudendal nerve block.
Coagulopathies and prior surgery in the area with altered local anatomy are relative contraindications to undergo pudendal nerve block.
Equipment
The equipment required for pudendal nerve block consists of chlorhexidine or povidone-iodine based solution, disposable sterile drapes, sterile gloves, sterile gauze swab, sterile syringes and needles, and local anesthetic solution of choice. Lidocaine 1% or bupivacaine 0.25% are the most commonly used solutions. Based on the physician’s preferences, ultrasound or fluoroscopy are options. Equipment for monitoring a patient’s hemodynamic status should also be available.
Personnel
Staff typically consists of a nurse and a physician trained in performing PNB. Depending on the imaging modality used, a technician should be present as well.
Preparation
The first step is to obtain the patient’s consent to perform the procedure. The equipment and medications required for the procedure must be ready and present in the room prior to starting the procedure. After conducting the time-out, the patient gets placed in the desired position. The targeted area is appropriately cleaned and covered by sterile drapes. Depending on the imaging modality of choice, the room should be equipped with that device.
Technique
A pudendal nerve block aims to block the nerve as it enters the lesser sciatic foramen, 1 cm inferior and medial relative to the attachment of the sacrospinous ligament to the ischial spine. Different anatomical approaches are utilized to achieve successful PNB.
The transvaginal approach to pudendal nerve block is a common approach for obstetric procedures. The female patient positioning is in the lithotomy position. Through the lateral vaginal wall, the clinician will identify the ischial spine. Through a long injection needle with a guide, the sacrospinous ligament gets punctured, and the needle is passed 1 cm caudal from the ischial spine until noticing a loss of resistance.[10] Using a needle guide such as the Iowa Trumpet is recommended to limit the depth of penetration and minimize tissue injury. Upon negative aspiration, the local anesthetic is injected posteriorly to the ischial spine at the attachment of the sacrospinous ligament. The injection can also be performed medial to the ischial spine to minimize the risk of anatomical damage.[11] Pinprick test in the anogenital area is performed to assure adequate anesthesia in the region.
The other method is the transperineal approach. This method is also useful in anorectal and urological procedures. The male or female patient will be placed in the lithotomy position. After identifying the ischial spine, the needle will puncture the skin transperineally, medial to the ischial tuberosity. The needle is advanced in the posterolateral direction until it touches the ischial spine. The needle is then advanced through the sacrospinous ligament and 1 cm in the medial inferior direction to the ischial spine. After negative aspiration, the local anesthetic of choice is injected.
A pudendal nerve block can also be performed via a perirectal approach using a nerve stimulator to elicit contractions of the external anal sphincter. Patient positioning is recumbent. The clinician’s index finger will be inserted into the anus to palpate the ischial spine. The needle is advanced lateral to the rectum towards the ischial spine.[12] Similar to the other methods, the needle is advanced 1 cm inferior and medial to the attachment of the sacrospinous ligament to the ischial spine. After negative aspiration, the local anesthetic of choice is injected.
The effect of the block is usually immediate. Depending on the clinical symptoms and type of procedure, a pudendal nerve block is either unilaterally or bilaterally. PNB can take place with or without ultrasound guidance in females. However, in male patients, PNB is typically performed using ultrasound guidance due to challenges in identifying the anatomical landmarks.[13] PNB under MRI, fluoroscopy, or CT guidance have also been described, but are less common methods.
Complications
The most common side effect of pudendal nerve block is discomfort at the injection site. The risk of bleeding and infection are less common. The more serious side effects occur rarely and include pudendal nerve damage or structural injury of the organs in the proximity of the pudendal nerve, such as the bladder and rectum. Pudendal artery puncture intravascular injection of local anesthetics can cause systemic local anesthetic toxicity and potentially be fatal.
Clinical Significance
A pudendal nerve block can serve as a diagnostic method to reveal underlying pudendal neuralgia and is performed primarily with local anesthetics for the test block. Patients who report significant pain relief are candidates for PNB performed with corticosteroids and local anesthetics for potential long term pain relief. The effect of the block is variable and reported from weeks to months.
Compared to general anesthesia or neuraxial anesthetic methods, PNB has shown to achieve a high level of pain control, and patients require less systemic analgesics.[14] PNB, in line with other regional anesthesia techniques, will minimize the risk of developing complications associated with general anesthesia, such as cardiopulmonary depression, as well as complications associated with neuraxial anesthesia such as urinary retention.
However, due to patient discomfort associated with the local injections as well as the risk of injuring critical structures, PNB is underused, especially in male patients.[13]
Enhancing Healthcare Team Outcomes
The provider should educate the patient before the procedure. A pudendal nerve block is a safe and cost-effective method of obtaining regional anesthesia in the targeted area; however, patients require counsel that the response to the block is unpredictable, and they might not experience pain relief. When using a pudendal nerve block, the nursing staff will play a vital role in the entire process, from preparing the patient for the procedure, monitoring them during the block while assisting the clinician, and providing post-procedural care. With an interprofessional team approach, PNB can achieve a higher rate of successful patient outcomes. [Level 5]
Nursing, Allied Health, and Interprofessional Team Interventions
- Obtain consent
- Educate the patient about the procedure
- Act as a chaperone
- Have all monitoring equipment in the room
- Drape and prep the patient
Nursing, Allied Health, and Interprofessional Team Monitoring
- Monitor the patient during the procedure
- Comfort the patient
(Click Image to Enlarge)