Pulmonary Hypertension
- Article Author:
- Sean Oldroyd
- Article Editor:
- Abhishek Bhardwaj
- Updated:
- 8/10/2020 4:18:52 PM
- For CME on this topic:
- Pulmonary Hypertension CME
- PubMed Link:
- Pulmonary Hypertension
Introduction
Pulmonary hypertension encompasses a heterogeneous group of disorders with the common feature of elevated pulmonary vascular resistance. Patients often present with nonspecific symptoms of worsening weakness and dyspnea on exertion. Pulmonary hypertension is a progressive disease with treatment focused on management of symptoms and treatment of underlying diseases.[1]
Etiology
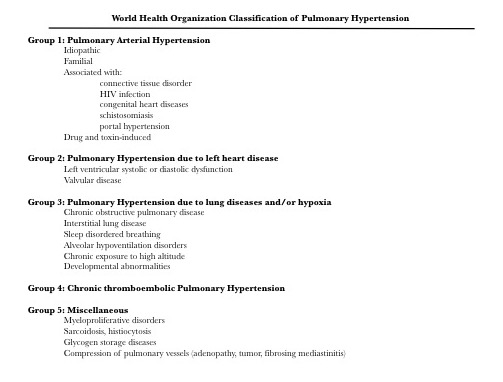
Pulmonary hypertension (PH) arises from many etiologies. In 1998, the World Health Organization (WHO) organized PH into 5 classifications according to the cause, and these classifications were updated in 2013 (figure 1). Group 1 can be thought of as primary pulmonary hypertension, or pulmonary arterial hypertension (PAH). Among this group, idiopathic PAH is the most common condition, with other causes such as toxin-induced, connective tissue disorders, and other related conditions being less prevalent. Group 2 involves PH due to left heart disease, which is the most common cause of PH. Group 3 PH is due to lung diseases such as chronic obstructive pulmonary disease and interstitial lung disease. Chronic pulmonary thromboembolism causes group 4 PH, and group 5 PH is due to unclear or multifactorial causes, as noted in the figure.[1][2][3][4]
Epidemiology
PAH is a rare disease. The estimated prevalence is between 15 and 50 cases per million individuals. Among those with PAH, idiopathic PAH is the most common and is more common in women than men. Pulmonary hypertension due to other diseases, such as chronic heart or lung diseases, reflects epidemiology similar to the associated disease.[5][6]
Pathophysiology
PAH is most-commonly idiopathic and is characterized by increased vascular resistance and blood vessel narrowing within the pulmonary vasculature. Restricted flow through pulmonary arteries, as found in PAH, is thought to have molecular and genetic causes which lead to hypertrophy of smooth muscle, endothelial cells, and adventitia. In response to the increased resistance, the right ventricle will increase filling and stroke volume, which further increases pulmonary arterial pressure. Over time, right ventricular hypertrophy develops. In the other groups of PH, increased pulmonary vascular resistance is similarly due to restricted flow, but it is typically secondary to another process such as left heart disease, chronic lung disease or chronic pulmonary thromboembolism.[1]
Histopathology
In idiopathic PAH, arterial walls show medial hypertrophy, with the proliferation of endothelial cells, smooth muscle cells, fibroblasts, and myofibroblasts, as well as the transition of endothelial cells in the pulmonary arteries to smooth muscle-like mesenchymal cells. Additionally, there may be an inflammatory component of PAH, as affected vessels display increased macrophages and lymphocytes.
History and Physical
The presenting symptoms of PH will reflect the underlying cause of hypertension, but PH patients will typically complain of dyspnea, fatigue, angina, and they may present after a syncopal episode. Group one PH patients will often complain about steadily worsening dyspnea on exertion.[1] Similarly, the physical exam may be nonspecific, but symptoms typically reflect the degree of right ventricular (RV) dysfunction. As RV function decreases, blood pressure may be normal to low, and jugular venous pulsations may be noted. Murmurs may be auscultated and reflect the underlying cause. Right-sided murmurs, such as tricuspid regurgitation, may develop as right heart strain and dilation increased. An aortic or mitral stenosis murmur points to left heart disease as a contributing factor in the patient’s PH. The remainder of the exam may reflect signs of right heart failure, such as hepatomegaly, peripheral edema, and ascites.
Evaluation
Biomarkers that are commonly evaluated in the context of heart diseases, such as brain natriuretic peptide (BNP) and troponin, are commonly measured in patients suspected of having PH, but there is no clearly-established role for these tests in the diagnosis of PH. The 6-minute walk test is useful to establish a baseline of functional performance as well as to monitor the progression of the disease. A chest radiograph may be useful to evaluate for signs of cardiomegaly, increased right ventricular size, or pulmonary vascular congestion which may be seen in left heart disease. [1] [7]
Electrocardiogram (ECG) may show signs of left heart disease such as left ventricular hypertrophy in group two PH. Right axis deviation as well as upright R waves in V1-V2 with deeper S waves in V5-V6 may represent right ventricular hypertrophy or right heart strain and can be seen in PAH. Similar to chronic lung diseases such as chronic obstructive pulmonary disease, frequent premature atrial contractions, and multifocal atrial tachycardia may be present on ECG.[1]
The noninvasive screening test of choice is a transthoracic echocardiogram. Pulmonary artery systolic pressure greater than 40 mm Hg or mean pulmonary artery pressure (PAP) of 25 mm Hg should indicate further evaluation for pulmonary hypertension. Other noninvasive measures may be used as indirect markers of PH, such as the Tei myocardial performance index, which measures the efficiency of the RV, and the tricuspid annular plane systolic excursion (TAPSE), which will decrease as the RV dilates and function declines.[1]
Right heart catheterization allows for measurement of mean PAP as well as pulmonary capillary wedge pressure (PCWP). Mean PAP greater than 25 mm Hg with associated PCWP less than 15 mm Hg is diagnostic of PAH, while elevated mean PAP and PCWP greater than 15 mm Hg is typical in patients with PH due to left heart disease. Vasoreactivity testing may be done during right heart catheterization, in which nitric oxide or another vasodilator is administered during the procedure. A reduction of 10 mmHg or more in mean PAP without a reduction in cardiac output is considered a positive vasoreactivity test.[1] [7]
Treatment / Management
Treatment of pulmonary hypertension secondary to other diseases (groups 2 to 4) should focus on treatment of the underlying disease, and there is no established role for the medications indicated for PAH in these patients.[1] Group one PH treatment can be considered a stepwise progression, and typically requires referral to a center equipped to diagnosis, treat, and monitor PAH. Calcium channel blockers such as nifedipine, diltiazem, and amlodipine are useful in patients with a positive vasoreactivity test. For patients with a negative vasoreactivity test or who have an inadequate response to calcium channel blockers. Treatment is focused on decreasing pulmonary vascular resistance and PAP but is not curative.[8][9][10][11]
Endothelin receptor antagonists such as ambrisentan, bosentan, and macitentan bind to endothelin and inhibit vasoconstriction that is typically caused by endothelin. These can be given orally and are recommended for mild and moderate disease, NYHA class II and III. Phosphodiesterase 5 (PDE-5) inhibitors (tadalafil, sildenafil, vardenafil) inhibit enzymatic processes and result in increased cyclic guanosine monophosphate, causing pulmonary and systemic vasodilation. Prostaglandin analogs replete the decreased prostaglandin that is decreased in pulmonary hypertension. These activate the prostacyclin receptor which will ultimately lead to pulmonary vasodilation. Epoprostenol is given as a continuous intravenous infusion, and treprostinil may be given intravenously, subcutaneously, orally, and via inhalation. [12][13]
Patients with PH due to chronic thromboembolism should be referred for evaluation for endovascular thrombectomy. The final treatment option for patients who fail aggressive medical treatment is heart-lung transplantation.[1] [14]
Differential Diagnosis
Diagnosis of PH is commonly delayed as the presenting symptoms overlap other disease processes. Other conditions to be considered in the differential diagnosis include, but are not limited to, congestive heart failure, coronary artery disease, pulmonary fibrosis, chronic obstructive pulmonary disease, valvular heart disease, hypothyroidism, and pulmonary embolism.[1]
Enhancing Healthcare Team Outcomes
Pulmonary hypertension has many causes and without treatment, it carries high morbidity and mortality. The condition is best managed by an interprofessional team that includes a pulmonologist, cardiologist, thoracic surgeon, radiologist, pathologist, specialty nurses and an internist. The key is to treat the primary condition causing pulmonary hypertension. The majority of causes of secondary pulmonary hypertension are cardiac and lung disorders with a minor contribution from other vasculitic syndromes. Without treatment, premature death is common. Those who are treated do have a longer life expectany but lack of medication compliance/treatment can lead to a poor quality of life.[15][16][17] (Level V)