Pure Red Cell Aplasia
- Article Author:
- Ankit Mangla
- Article Editor:
- Hussein Hamad
- Updated:
- 10/7/2020 2:22:37 PM
- For CME on this topic:
- Pure Red Cell Aplasia CME
- PubMed Link:
- Pure Red Cell Aplasia
Introduction
Pure red cell aplasia (PRCA) is a rare disorder that presents with anemia secondary to the failure of erythropoiesis. It is characterized by normocytic, normochromic anemia, associated with reticulocytopenia in the peripheral blood and absent or infrequent erythroblasts in the bone marrow.[1][2][3] It is distinct from aplastic anemia in having intact precursors for platelets and leukocytes, which are normal in number and morphology in the peripheral blood. Kaznelson first described PRCA in 1922.[1][4] The congenital (or inherited) form of PRCA, also called Diamond-Blackfan syndrome, was first described by Joseph in 1936 and subsequently by Diamond and Blackfan in 1938.[4][5] The association of PRCA with thymoma led to the discovery of the autoimmune mechanisms involved in the pathogenesis of this rare disease. PRCA has been the object of much laboratory research not only due to the immune mechanisms involved in the destruction of the red blood cells but also because of its association with parvovirus B19 in patients with sickle cell disease. However, due to the rarity of the disease, PRCA can never be evaluated in large controlled clinical trials. As a result, the majority of recommendations have their basis on retrospective trials or anecdotal case reports.
Etiology
Pure red cell aplasia can either be inherited or acquired.
- Congenital PRCA
- Diamond-Blackfan or Blackfan-Diamond syndrome
- Acquired PRCA
- Autoimmune/ Collagen disorders - systemic lupus erythematosus, rheumatoid arthritis, inflammatory bowel disease.
- Leukemias
- Lymphoproliferative disorders[6][7]:
- Chronic lymphocytic leukemia (CLL) (common)
- Large granular lymphocytic leukemia (LGL)(common)
- Hodgkin disease
- Non-Hodgkin lymphoma
- Multiple myeloma
- Castleman disease
- Waldenstrom macroglobulinemia
- ABO-incompatible stem cell transplant
- Solid tumors[1][4]:
- Thymoma is strongly associated
- Breast
- Biliary
- Gastric
- Lung
- Thyroid
- Renal cell
- Carcinoma of unknown origin
- Virus[1][4]:
- Parvovirus B19 (most common) - can lead to transient aplastic crises
- Human immunodeficiency virus (HIV)
- T-cell leukemia-lymphoma virus, Epstein-Barr virus (EBV)
- Hepatitis A, B, C, and E
- Cytomegalovirus
- Bacterial infections - group C streptococcus, tuberculosis, bacterial sepsis
- Drugs - recombinant erythropoietin (rhEPO) is most common.
- Pregnancy
- Riboflavin deficiency
Epidemiology
Pathophysiology
PRCA is an extremely heterogeneous disease both clinically and pathologically. The pathophysiology is discussed here based on the classification.
Congenital PRCA or Diamond Blackfan anemia (DBA)
- The congenital PRCA (also known as inherited PRCA) or DBA, is now recognized as a disease of ribosomal biogenesis[5]. The initial theories about DBA being a T-cell mediated or a humoral mediated disease, or being secondary to a defective microenvironment were discarded with the discovery of defective ribosomal genes and success of allogeneic stem cell transplants in patients with congenital PRCA, respectively.[5][9] Sporadic cases are most common (55 to 60%), followed by autosomal dominant inheritance in up to 40 to 50% patients. Rarely, autosomal recessive inheritance may occur in DBA siblings from unaffected consanguineous parents.[10] The first gene identified was in a Swedish patient who carried a balanced translocation between chromosome X and 19.[11] Since the disease is prevalent in both sexes in a 1 to 1 ratio (essentially ruling out the role of sex-linked chromosome X), chromosome 19 was deducted to be the affected chromosome.[5] Multiple European families were studied, and linkage analysis mapped to a site on chromosome 19q13.[12] In 1999, the first mutation in DBA was identified in the ribosomal protein (RP) S19 (RPS19), which is responsible for encoding a protein that assists in ribosome assembly.[13] The mutations, most of them being whole gene mutations, translocations, or truncations, lead to haploinsufficiency, which leads to RPS19 behaving like a dominant gene. Subsequently, 19 other mutations were identified in RP genes using whole exome/genome sequencing and comparative genomic hybridization/single nucleotide polymorphism array. Out of 80 RP genes, mutations in 20 genes have been identified, which can lead to congenital PRCA.[5] However, RPS19, RPL5, RPS26, RPL11, RPL35a, and RPS 24 account for 70% of the mutations.[5] Some non-RP genes like TSR-2, GATA1, and EPO genes have also been identified; however, it is still open to debate whether they lead to DBA or a DBA-like disease.[14][15][16]
Transient Aplastic Crisis and Parvovirus B19 infection
- The transient aplastic crisis occurs when the concentration of parvovirus B19 is very high in the blood. The virus has an affinity for the progenitor erythroid cells because of their P antigen, which acts as a receptor for the entry of the virus into the cell.[17] Both in vitro and in vivo experiments have demonstrated the ability of the virus to target and lyse, especially the late progenitor cells, and inhibit erythropoiesis.[18] The arrest of differentiation at the pronormoblast stage is characteristic.
- Typically, in a patient with acute infection, neutralizing antibodies (IgG) develop quickly. Although a phase of reticulocytopenia may occur, anemia does not manifest unless RBC survival becomes reduced. In patients with inherited hematological disorders (like thalassemia, sickle cell disease, hereditary spherocytosis, etc.), an infection with parvovirus B19 can induce a transient aplastic crisis. Thrombocytopenia and neutropenia are also well documented in such patients. However, due to the development of humoral immunity, the aplastic crisis occurs only once in life.[18]
- In children with sickle cell disease, transient aplastic crisis increases the frequency of fever, acute chest syndrome, pain, and acute sequestration crises.[19] The viral levels are very high in such patients, and no antibody is detected (which essentially differentiates this from the fifth disease). Up to 75% of patients with sickle cells are infected with parvovirus by the age of 20 years. However, most patients with sickle cell disease are completely asymptomatic despite infection with parvovirus.[19]
- It is worth noting that this transient presentation is separate from the fifth disease, which is characterized by IgM antibodies against the parvovirus. The viral levels are low to undetectable, and the symptoms of arthritis, arthralgia, and ‘slapped cheek appearance’ occur due to the antibody-virus immune complex.[18]
Transient erythroblastopenia of childhood (TEC)
- TEC is a poorly understood entity. Parvovirus B19 is the most commonly implicated virus in TEC.[20] Reports exist pointing to other viruses, but these reports do not demonstrate consistency in causation.[21] An immune-mediated mechanism is implicated in the pathophysiology of TEC, where both IgG and T-cell mediated mechanisms appear to play a role. In one study, a reduction in the number of T-cells led to a dramatic increase in the number of colony-forming units for erythroid cells.[22]
- The drugs which carry implications in PRCA can also cause TEC via a hapten based mechanism. The serum antibody can act against the erythroid precursors only in the presence of the offending medication.[23][24]
Secondary acquired PRCA
- PRCA with autoimmune disorders.
- Immune-mediated erythropoietic failure is central to PRCA seen in patients with autoimmune diseases like RA, SLE, myasthenia gravis, auto-immune hemolytic anemia, acquired hypogammaglobulinemia, autoimmune polyglandular syndrome, and thymoma. Laboratory evidence has clearly shown the existence of both ‘antibody-mediated and cell-mediated mechanisms of inhibition of red cell erythropoiesis.[4] Immunoglobulin fractions from patients have been shown to inhibit heme synthesis and red cell progenitors in vitro.[25] Further credence to autoimmune-mediated mechanisms comes from the fact that secondary acquired PRCA responds to treatments like plasmapheresis and anti-CD20 therapies.
- Erythropoietin (EPO) associated antibodies causing PRCA.
- Around the turn of the 21st century, new reports of EPO associated PRCA were published in the literature.[26][27][28] The administration of the recombinant EPO (rhEPO) to patients on renal dialysis was the most frequent link between antibodies against EPO and the development of PRCA. The peak incidence was in 2011 was associated with a change in the formulation of a specific epoetin alfa product. In the past, epidemiological studies showed that the leachates in the rubber-stop of pre-filled syringes and particular stabilizers caused the antibody formation. After addressing these issues, the cases of PRCA have become rare.[29] Although the glycosylation of rhEPO is different from native EPO, the antibody gets directed against the conformational epitopes of protein moiety and not the sugar moiety. Research has identified a few HLA types which correlate with increased immunogenicity against EPO.[30][31]
- ABO-incompatible transplant-associated PRCA.
- Using donors mismatched at the major ABO locus leads to the development of ‘target-specific’ antibodies and leads to delayed engraftment of the erythroid precursors or even PRCA later in life. Specific targets are still not recognized in such patients.
- PRCA associated with lymphoproliferative disorders.
- CLL is the most common lymphoproliferative disease associated with PRCA. A T-cell mediated mechanism is more commonly associated with suppression of erythropoiesis rather than an antibody-mediated mechanism. Mutation in the signal transducer and activator of transcription three-gene (STAT3), which leads to activation of clonal cytotoxic CD8+ cells and suppression of erythropoiesis, have been identified in patients with PRCA.[32][33] Research has also shown that lymphocytes from patients diagnosed with idiopathic PRCA and PRCA secondary to CLL, LGL, thymoma, lymphoid malignancies, EBV, and human T-cell leukemia virus-1; suppress erythropoiesis in colony assays. Researchers have suggested several mechanisms where T-cells can reduce erythropoiesis via T-helper cell-mediated antibody production, major histocompatibility complex (MHC) restricted, or unrestricted recognition of red cell progenitors; or via MHC-unrestricted cytotoxicity.[4] T-cells are also shown to downregulate inhibitory responses of natural killer cells and cause lysis of erythroid colony-forming units.[34]
- Persistent Parvovirus B19 infection:
- The intrinsic humoral immunity clears the parvovirus B19 infection within 1 to 2 weeks. Patients with immunodeficiency secondary to viruses (HIV), drugs (chemotherapy, immunosuppressive drugs), or congenital immunodeficiency cannot mount an antibody response against the parvovirus. This immunodeficiency leads to a persistent infection that is toxic to the erythroid progenitor cells and leads to chronic red cell aplasia. In pregnant mothers, the parvovirus can be transmitted to the fetus in the mid-trimester and is toxic to the erythroid progenitors in the fetal liver leading to severe red cell aplasia and hydrops fetalis. In the rare instance, when such an infant was rescued with timely red cell infusions, they still had persistent congenital PRCA or dyserythropoietic anemia.[18]
- PRCA as a manifestation of myelodysplasia
- Drugs causing PRCA:
- Many drugs have implications for involvement in PRCA; however, there is limited evidence from case reports. Drugs like diphenylhydantoin, sulfa and sulfonamide drugs, azathioprine, allopurinol, isoniazid, procainamide, ticlopidine, ribavirin, and penicillamine are implicated in etiology of drug-induced PRCA. An IgG-mediated mechanism appears to be the cause in patients receiving diphenylhydantoin and rifampin.[3]
Histopathology
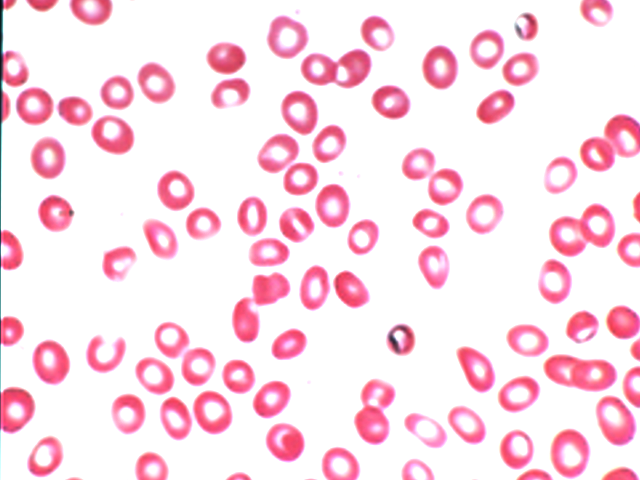
The peripheral smear demonstrates normocytic normochromic anemia with reticulocytopenia. The white cell count and platelet count are normal in number and morphology. The histological picture seen on bone marrow examination depends on the cause of PRCA. Complete absence or near absence of erythroblasts (less than 1% erythroblasts on marrow differential count) from an otherwise normal marrow is a characteristic of autoimmune PRCA. Rarely, a few erythroblasts or basophilic erythroblasts are present, but their number never exceeds 5% of the differential count.[3] In patients with B19 parvovirus infection, large proerythroblasts with vacuolated cytoplasm and pseudopodia (giant pronormoblasts) appear on the marrow exam; however, this is not a diagnostic finding.[18] Lymphoid aggregates along with plasmacytosis and lymphocytes point to an inflammatory reaction. Any signs of hypercellularity, presence of ringed sideroblasts, or dysplastic features that extend beyond one cell line are suggestive of a myelodysplastic variant of PRCA or MDS itself.
History and Physical
There are no specific signs or symptoms associated with PRCA. The most common presentation is the same as that of anemia. Generalized fatigue, decreased exercise tolerance, palpitations, and in extreme cases, presyncope or syncope (when associated with cardiac stress due to increased work of function). The physical exam is also non-specific. Pallor is a feature in all patients. A thorough skin exam is necessary to look for erythema infectiosum, which correlates with parvovirus B19. A prodromal rash is sometimes present in children where a reticular and lacy body eruption is visible. The systemic examination should look for swollen lymph nodes, hepatomegaly, and splenomegaly. None of these signs or symptoms are definitively diagnostic of PRCA by themselves but will provide vital clues in establishing etiology.[1][3]
Diamond-Blackfan syndrome is associated with physical anomalies in up to a third of all patients.[36] Craniofacial dysmorphism and thumb abnormalities are classic in DBA.[37] Short stature, urogenital abnormalities, web neck, skeletal, and cardiac defects can also present in patients with DBA.[38] A classic description is that of Cathie: “tow-colored hair, snub nose, wide-set eyes, thick upper lips, and an intelligent expression.”[39] Likewise, Aase and Smith described the triphalangeal thumb abnormality along with anemia seen in DBA.[40]
Evaluation
Isolated anemia and reticulocytopenia in the presence of normal white cell count and platelet count are suggestive of PRCA. A review of the peripheral smear is the first step in the evaluation of PRCA. Further evaluation is pursued to determine the degree of anemia and the etiology of PRCA and rule out other diagnoses.[1][5][3]
- Tests for evaluating the degree of anemia:
- Complete blood count with differential (Anemia along with a normal white count, platelet count, and a markedly reduced reticulocyte count strongly support the diagnosis of PRCA)
- Erythropoietin level (A high level supports the diagnosis)
- Type and Cross (for pure red blood cell transfusion)
- Peripheral blood to determine the etiology of PRCA:
- Autoimmune conditions
- Antinuclear antibody
- Antineutrophil cytoplasmic antibody
- Rheumatoid arthritis antibody
- Viral studies
- Parvovirus B19
- Viral hepatitis A, B, C and E
- Human immunodeficiency virus (HIV)
- Epstein-Barr Virus (EBV)
- Cytomegalovirus (CMV)
- Human T-cell leukemia-lymphoma virus (HTLV-1)
- Flow cytometry (of peripheral blood cells) to rule out malignant clonal cells
- T-cell gene rearrangement
- Plasma cell disorder
- Quantitative immunoglobulins
- Free light chains (Kappa and Lambda)
- Serum electrophoresis and Immunofixation
- Pregnancy test (in case of women)
- Autoimmune conditions
- Bone marrow should have testing for the following:
- Cytogenetics
- Flow cytometry
- T-cell gene rearrangement
- Tests to determine iron overload[41]:
- Ferritin level- increases as the number of transfusions increase
- Iron level
- Total iron-binding capacity
- Hepatic and Renal panel (Useful in monitoring the liver and kidney function and in choosing iron chelator)
- MRI Liver to determine the liver iron concentration
- Diamond Blackfan syndrome is associated with increased activity of erythrocyte adenosine deaminase. Critical challenges exist in performing this test.[5][42][5]
- Very few labs perform this test all over the world (In the US, only one lab performs this test)
- The test must be performed only in patients who have not received red cell transfusions.
- The test must be done only on a fresh blood sample or on a blood sample stored at 4 degrees C only for a few days.
Treatment / Management
Inherited PRCA
Untreated inherited PRCA results in severe anemia, which leads to congestive heart failure and death. Glucocorticoid use, blood transfusion, and allogeneic stem cell transplant (ASCT) is the mainstay of treatment in children.
- Glucocorticoids:
- Corticosteroids were the first drugs proved to be efficacious in children with DBA.[41][38][36] Children who present at an older age, have a normal platelet count, and have a family history of PRCA, respond better to steroids. Those children who are born prematurely or present at a younger age are poor responders.[43] Typically, prednisone is started at 2 mg/kg daily in three to four divided doses. A response occurs in approximately two-thirds of the patients who receive steroids. Reticulocyte recovery is noted within 1 to 4 weeks, followed by a rise in hemoglobin. An adequate response is a goal Hb of above 9 g/dL without the need for transfusion. A meaningful response should occur within a few weeks of starting high dose steroids. If even a partial response does not take place by four weeks of starting steroids, then it should be deemed as steroid failure. The weaning of steroids starts upon achieving a partial response. A low-dose maintenance regimen (0.5 to 1 mg/kg every day or on alternate days) can be used to maintain remission if it does not compromise growth. Eventually, patients may only need very low doses of prednisone, sometimes only 2 to 3 times a week.[41][38][44]
- Various patterns are possible, ranging from patients having a prompt recovery and apparent cure to treatment-refractoriness long after an initial response to being completely unresponsive to steroids. Those who do not respond to steroids should restart on chronic transfusions. A second attempt at steroids can be made 12 to 18 months after initial unresponsiveness.[41][45]
- Long term use of steroids is associated with toxicity, which includes growth retardation, cushingoid facies, hypertension, diabetes, and cataract. Patients treated with high dose steroids must receive prophylaxis for Pneumocystis jirovecii. All attempts should be made to give live vaccines before starting steroid therapy; however, once the therapy starts, live vaccines should not be administered.[41]
- Red cell transfusions:
- This is mostly used in acutely symptomatic patients and in those who are refractory to steroids. Chronic red cell transfusion is preferable to long term use of high dose steroids. On the other hand, frequent transfusions not only results in hemosiderosis but also leads to alloimmunization and antibody formation.[46] Iron chelation should start early in patients requiring frequent blood transfusions (usually before two years of age or those requiring more than 10 to 20 transfusions). The goal of hemoglobin is 7 to 9 g/dL, which should be maintained to allow for normal growth and sexual development. The median life expectancy of children compliant with red cell transfusions and iron chelation is 30 to 40 years, and even less for those who are not compliant.[41]
- Stem cell transplant (SCT):
- Transfusion dependence remains the number one indication for pursuing stem cell transplant in patients with DBA.[47] Either HLA-matched related donor or alternative donor transplant can be an offer made to patients with DBA.[41][47] Younger patients who receive matched sibling donor allogeneic SCT for DBA have a survival rate of more than 90%. Since the year 2000, registry data show an 80% survival with allogeneic unrelated donor SCT.[38][41] Reduced-intensity and non-myeloablative regimens are options for adult patients with iron-overload or those patients who have significant organ toxicity. A history of chronic transfusion reduces the success of SCT in patients due to underlying iron overload. An aggressive approach to reducing iron overload after SCT must be adopted.[41]
- Other therapies:
- Treatment with interleukin-3, high-dose methylprednisolone, cyclosporine, and other immunosuppressive agents, prolactin induction by metoclopramide have not gained much success.[48][41] Gene transfer in vitro, which has the potential to correct RSP19 has shown promise but remains in the experimental stage.[49]
Transient PRCA
- Parvovirus B19
- The effect of the viral infection cedes with the development of humoral immunity, which happens within a couple of weeks. This is a lifelong immunity that prevents re-infection. In patients with persistent parvovirus infection, a course of intravenous immunoglobulin (IVIG) (2 g/kg divided over five days) corrects parvovirus induced PRCA in 93% patients, but up to 50% relapse within 4 to 5 months.[50][51] The prescribing physician should be mindful of the small yet important risk of renal tubular acidosis and thrombosis with the use of IVIG.[52][50]
- Transient erythroblastopenia of infancy (TEBI):
- TEBI resolves within a few weeks, but anemia may persist for months. Any drug which suspected of causing TEBI should be withdrawn. Transfusion support may be necessary for a brief period.
Acquired PRCA
- Immune-mediated PRCA in adults
- Cyclosporine has emerged as the first choice of treatment with a response rate as high as 75%.[3] It is even effective in patients who have failed many other lines of treatment. It is a natural cyclic polypeptide immunosuppressant that can be used either alone or in combination with prednisone for a patient with PRCA. A reasonable starting dose is 6 mg/kg daily (with or without prednisone at 30 mg/day) to target a trough level of 150 to 250 ng/mL.[3] Once hemoglobin normalizes, a slow taper of cyclosporine can be a consideration; however, maintenance doses may be necessary.[3] In patients treated with cyclosporine, the relapse of PRCA occurred in those who did not taper off the medication.[53] Maintenance doses of cyclosporine may be required to maintain remission.[54]
- Corticosteroids were the therapy in an era before the discovery of cyclosporine. The first series of patients with PRCA who received treatment with steroids reported a response rate of 37% with a median duration of response at 2.5 weeks. Since then, other reports have recorded a response rate between 30 to 60%. The rate of relapse was as high as 80% in patients who were being tapered off steroids.[1][55] Most of the patients who relapsed after the withdrawal of steroids responded again to immunosuppressive therapy. The best response occurred in patients who received cytotoxic agents along with corticosteroids.[55]
- Cytotoxic agents have been used primarily in patients who are refractory to cyclosporine. Cyclophosphamide has been the most researched cytotoxic agent compared to other drugs.[1] It is particularly effective in patients with LGL induced PRCA. Either cyclophosphamide or methotrexate can be used in combination with steroids. Upon achieving a hematologic response, the tapering of the cytotoxic drug starts. The treatment with cyclophosphamide does not extend beyond six months due to the high risk of secondary malignancy from the cumulative effect of the alkylator. Although cyclophosphamide can induce longer remissions compared to cyclosporine, the relapse rates are high following its withdrawal. A crossover to cyclosporine as a maintenance regimen after achieving hematological response with cytotoxic drugs has been suggested but never tested in a trial.[1][3]
- Tacrolimus provides effective immunosuppression, which can be useful in the management of PRCA; however, few reports have identified tacrolimus as the drug causing PRCA.[56]
- Antithymocyte globulin, used in the same dose as aplastic anemia, has a 50% response rate in PRCA.[56]
- Rituximab (anti-CD20) and alemtuzumab (anti-CD52) have demonstrated efficacy in patients with PRCA.[57] Rituximab is primarily used in patients with the lymphoproliferative disorder and has shown efficacy in resolving PRCA associated with an underlying lymphoproliferative disorder.[1][3]
- Daclizumab, a monoclonal antibody against the IL-2 receptor is effective in approximately 40 percent of patients.[58]
- Intravenous immunoglobulins, plasma exchange, and allogeneic stem cell transplant are some other modalities of treatments for immune-mediated PRCA in adults.[3]
- Despite a few case reports describing success with splenectomy, androgens, and the use of erythropoietin, these modalities are not recommended.
- Thymoma associated PRCA:
- Although resection of thymoma is mandatory in patients with thymoma associated PRCA, the utility of this is not clear. Only a third of patients experience remission after surgery, and most of them would continue to have some degree of anemia throughout their lives. Many patients develop PRCA after resection of the thymoma, which raises questions regarding the utility of resecting the gland. Cyclosporine is the treatment of choice in patients with thymoma associated PRCA.[59][60]
- PRCA associated with incompatible stem cell transplants.
- The persistence of anti-donor isohemagglutinins directed against donor RBC and erythroid precursors beyond two months is an ominous sign. The likelihood of spontaneous remission decreases beyond this period.[61] Adjusting immunosuppressive regimen, donor-leukocyte infusion, plasma exchange, and use of anti-CD20 therapy (rituximab) has been used.[61]
- PRCA due to rhEPO antibodies
- It is rare to develop PRCA due to antibodies against rhEPO; however, a few cases remain. A few reports have suggested rechallenging with rhEPO (subcutaneous or intravenous) once no antibodies are detectable in the blood. However, this approach should be considered high risk and has resulted in the recurrence of PRCA.[62] Immunosuppression with cyclosporine A (with or without corticosteroids) is the first choice. The emergence of biosimilars in the European and US market may be able to circumvent this issue.[63]
Iron overload from chronic transfusions[41]:
- Deferoxamine: Used at a dose of 40 to 60 mg/kg/day subcutaneously over 8 to 12 hours/night and 4 to 7 nights/week. This is not as frequent an option due to the availability of oral formulations. It can still be used IV over 24 hours in patients with severe cardiac iron overload and cardiomyopathy.
- Deferasirox: Dosed at 20 to 30 mg/kg/day orally.
- Deferiprone: 80 to 100 mg/kg/day orally. Agranulocytosis is a major adverse effect. This treatment is very effective for patients with cardiac iron deposition.
Differential Diagnosis
Any patient presenting with anemia and reticulocytopenia requires evaluation for PRCA. The low reticulocyte count helps differentiate PRCA from hemolytic anemia (which can also have isolated anemia, albeit with reticulocytosis).
Within PRCA, a differentiation should be made between inherited, acquired, and transient PRCA.[1][3]
- Inherited PRCA is usually present since birth, but can present in older age as well.[64]
- Diamond Blackfan syndrome is associated with craniofacial and thumb abnormalities in the majority of patients; however, it is not a universal presentation. Elevated fetal hemoglobin (HgF) levels, elevated erythrocyte adenosine deaminase (very difficult to obtain), and ribosomal mutation analysis helps in establishing a diagnosis.
- Fanconi anemia must be ruled out with the use of cytogenetic analysis and clastogenic stress.
- Transient PRCA of infancy demonstrates self-recovery
- It is hard to differentiate inherited PRCA from acquired PRCA when the patient presents in adulthood. A thorough history, including family history, physical exam to look for anomalies, bone marrow examination, and cytogenetic analysis, would aid in establishing a diagnosis.
- Transient PRCA
- It is hard to distinguish transient PRCA from inherited PRCA. Spontaneous recovery gives a clue towards the diagnosis.
- When concomitant neutropenia is present, then aplastic anemia and acute lymphoblastic leukemia should be ruled out. A bone marrow exam will help in ruling this out.
- A thorough medication and drug exposure history is a must. Treatment with the offending medication must stop.
- Evaluate for parvovirus infection, which is treatable.
- Acquired PRCA
- Look for secondary causes, as listed in the etiology section above.
- Bone marrow should be examined thoroughly to rule out MDS, which can present with isolated anemia and reticulocytopenia.
- It is crucial to establish whether the PRCA is inherited or acquired, using the same tests listed.
Prognosis
The prognosis depends on the etiology of PRCA.
1. Inherited PRCA
- Patients who respond to and can get weaned off steroids can have a normal life span.
- Patients who do not respond to steroids and are dependent on chronic transfusions suffer from organ toxicity secondary to iron overload. Their median life expectancy is 30 to 40 years.[65]
- Those who receive stem cell transplant (SCT) at a younger age have better outcomes compared to those who receive SCT at an older age and after chronic transfusions.[41]
2. Acquired PRCA:
Japanese consortium reported the long term follow-up results of patients with PRCA in their cohort of patients, which gave some insight into the long term prognosis of patients with acquired PRCA.[54]
- The life span of patients with acquired PRCA is significantly shorter than the general population.
- The life expectancy amongst patients with different causes of PRCA (LGL versus thymoma versus idiopathic PRCA) was not different
- Infection and organ failure were the most common causes of death rather than the progression of the underlying disease. This finding further stresses on close monitoring and prompt management of infection (in patients on immunosuppressive therapy) and iron overload (in patients who receive chronic transfusions). Iron chelation in a cohort of patients with aplastic anemia showed improvement in hematopoiesis.[66]
- Maintenance with cyclosporine is essential for most patients to prevent relapses.[1]
- Patients who respond to steroids have a median survival of 12 years. Those who respond to cyclosporine A, their median survival has not been reached, and 95% of patients were alive at 14-year follow up.[1]
Complications
Children diagnosed with Diamond Blackfan anemia are predisposed to cancer. Although the risk of developing cancer is lower in patients with DBA compared to those diagnosed with Fanconi anemia, the risk is still higher than the general population belonging to the same age group. Reports exist of both solid and liquid malignancies with DBA in international registries. Acute myeloid leukemia is the most common hematologic malignancy, and osteogenic sarcoma is the most common solid organ malignancy diagnosed in children in DBA.[38]
Chronic anemia can lead to growth retardation and poor psychomotor development in children. Severe anemia can also lead to a hyperdynamic circulation, which increases the work of heart and hence, the risk of cardiac failure, especially in those with pre-existing heart disease and the elderly. In pregnancy, it can prompt premature labor, abnormally low birth weight. In pregnant patients with severe anemia, there are reports of increased maternal and fetal mortality. Overall, anemia can cause low energy, constant fatigue, and in general, a poor quality of life.[67]
Patients with PRCA who receive chronic transfusions eventually develop iron overload and related toxicities. Immunosuppressive therapy with cyclosporine or chronic steroid therapy can lead to myelosuppression and, eventually, opportunistic infections. The use of corticosteroids, whether short term high dose therapy or long term maintenance therapy, correlates with multiple adverse events.[68]
Deterrence and Patient Education
Patients and physicians should understand the recurrent nature of the disease, the need for long term therapy, repeated blood transfusions, and iron chelation therapy. Any patient diagnosed with inherited PRCA should be evaluated for stem cell transplant at an early age, rather than performing it later, when the comorbidities from additional therapies have increased exponentially. A close follow-up of the affected patients should be kept to prevent complications from both the underlying disease as well as the treatment.
Pearls and Other Issues
Pure red cell aplasia is a rare pathology that either presents as an inherited disease or that the patient acquires secondary to other conditions. Few pearls are listed here:
- The most common presentation is isolated anemia with reticulocytopenia. Bone marrow exam shows under 1% erythroblasts
- Diamond Blackfan anemia is the most common inherited PRCA. Craniofacial and thumb abnormalities are common, but not present in all patients.
- Steroids, chronic transfusion therapy, and stem cell transplant are the most effective modalities of managing patients with Diamond-Blackfan syndrome.
- Transient PRCA most commonly results from parvovirus B19 infection. Recovery is spontaneous, and immunity to parvovirus is lifelong. One must remember that parvovirus infection-related PRCA is different from the fifth disease, where the IgM antibody against the virus is at play.
- In immunocompromised patients, no humoral immunity may develop against parvovirus, and this may lead to chronic infection and relapsing course of PRCA.
- Acquired PRCA is both antibody-mediated as well as T-cell mediated.
- The most common lymphoproliferative diseases associated with PRCA is chronic lymphocytic leukemia and large granular lymphocytic leukemia.
- Many drugs are associated with acquired PRCA, which the clinician should stop before starting therapy for PRCA.
- Cyclosporine is the most effective drug for PRCA with the highest response rates. A maintenance dose of cyclosporine is needed to prevent relapse of PRCA, which usually occurs when stopping the medication completely.
- Steroids are an effective alternative to cyclosporine, albeit with low response rates. They are usually used along with cyclosporine.
- Chronic red cell transfusions correlate with iron overload and hemosiderosis. Iron chelation should start early in the course of treatment.
Enhancing Healthcare Team Outcomes
Pure red cell aplasia is a rare disorder. The inherited form is usually detected at birth, although many patients can also present in adolescent age or as young adults. It is imperative to maintain a broad outlook of the disease and investigate thoroughly starting with obtaining a good history, performing a thorough physical exam, and using appropriate clinical and genetic tests to determine the etiology.
Nurses, transfusion medicine, hematology, bone marrow transplant unit, and geneticist should work in close harmony with all clinicians as an interprofessional team to maximize the benefit to the patient. Patients managed with corticosteroids should be followed by the pharmacist to ensure that they are not developing complications. If there is any suspicion of osteoporosis, a bone scan is necessary. A pharmacist should examine the patient's medication record to look for drugs that may cause PCRA, as well as assist the clinician in any medication therapy undertaken in the management of the condition. These patients should also be followed by an infectious disease nurse, as they are prone to infections due to steroid therapy; the nurse can also monitor patient compliance and assess the effectiveness of the current treatment. The chronic blood transfusions can also result in iron overload, and hence the patient requires vigilant monitoring by the hematologist. These are examples of the interprofessional team approach to case management that optimizes positive patient outcomes. [Level V]
Due to the rarity of the pathology, no large randomized trials are possible, and the evidence of treatment comes from case series, retrospective studies of international registries, and few small prospective trials. [Level III to Level IV]