Neuroanatomy, Recurrent Artery of Heubner
- Article Author:
- Sunil Munakomi
- Article Editor:
- Joe M Das
- Updated:
- 7/31/2020 3:56:59 PM
- For CME on this topic:
- Neuroanatomy, Recurrent Artery of Heubner CME
- PubMed Link:
- Neuroanatomy, Recurrent Artery of Heubner
Introduction
First described by the German pediatrician Johann Otto Leonhard Heubner (1872), H.F. Aitken (an artist at the Massachusetts General Hospital) later labeled it as ‘Heubner’s artery’ (1909). Joseph Shellshear, an anatomist at St. Bartholomew’s Hospital in London, later termed the more appropriate and the current term ‘recurrent artery of Heubner’ for the same, pertaining to its characteristic course along the A1 portion of the anterior cerebral artery (ACA) subsequent to its origin (1920).[1]
Structure and Function
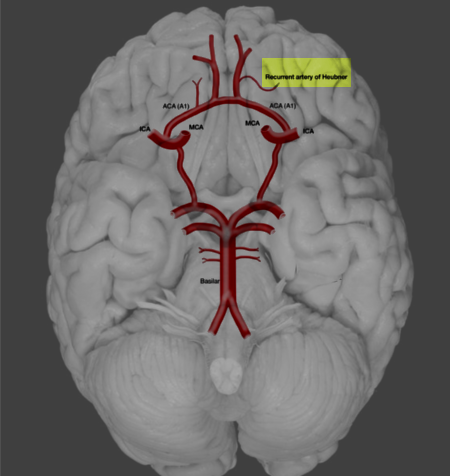
The recurrent artery of Heubner (RAH) is typically the largest of the perforating medial lenticulostriate arteries arising from ACA. The recurrent artery of Heubner can arise from A1, from A2, or at the junction of the ACA-ACoA (anterior communicating artery) of the ACA. Later the artery characteristically turns posteriorly and runs in close relation to the gyrus rectus to reach the anterior perforating substance.[1]
The recurrent artery of Heubner showed a mean diameter of 0.8 +/- 0.04, with a mean length of 23.4 +/- 1.1 mm in one study.[2]
The recurrent artery of Heubner has vascular supply mainly to[1]:
- The head of the caudate nucleus
- The medial portion of globus pallidus
- Anterior crus of the internal capsule
- Anterior hypothalamus
- Nucleus accumbens, a connection between caudate and the putamen
- Parts of the uncinate fasciculus connecting the limbic system with the frontal lobe
- Diagonal band of Broca connecting the septal area to the amygdala and
- The basal nucleus of Meynert located in the substantia innominata
Embryology
With the continued growth and development of the telencephalic vesicles, a vascular system develops from the rostral division of the internal cerebral artery. This vascular channel later gives origins to all the lenticulostriate vessels, including the recurrent artery of Heubner, and then also forms the adult middle cerebral artery (MCA). This embryological origin accounts for the formation of rete communication among branches of the recurrent artery of Heubner and the lenticulostriate branches from the ACA and the MCA.
Physiologic Variants
The most common origin of the recurrent artery of Heubner was from the A2, followed by the ACA-ACoA junction (43.4%) in one study.[1]
However, in other studies, the recurrent artery of Heubner most commonly originated from the junction of the A1 (origin of the ACA to the junction of the anterior communicating artery) and A2 (junction of the ACoA to the anterior border of the corpus callosum) segment of the ACA in 76.2% followed by A2 segment in 16.3% of cases.[3]
It was either absent or duplicated in around 6% of the cases in the series.[1]
It was triple in number in 0.14 % of cases in one study.[3]
The pattern of recurrent course of the recurrent artery of Heubner in its relation with A1 while moving towards the anterior perforated substance divide into[4][5]:
- Type I or the superior course (63%)
- Type II or anterior course (34%)
- Type III or posterior course (3%)
The intracerebral course of the recurrent artery of Heubner is uni-vectorial, thereby heading towards the head of the caudate nucleus. The recurrent artery of Heubner, during the extra- and intracerebral course, may join with the middle group of the lenticulostriate arteries or directly with the middle cerebral artery to form a rete.[4]
Surgical Considerations
The central concern during the clipping of the ACOM aneurysm is to safely clip the neck of the aneurysm following complete preservation and assuring patency of the recurrent artery of Heubner and other perforators. Intraoperatively, the surgeon can confirm this is the case with the visualization of the flow of the indocyanine green (ICG) dye within the recurrent artery of Heubner following permanent clipping of the aneurysm.
The blind areas can be visualized, and minimizing the inadvertent clipping or kinking of the recurrent artery of Heubner is possible with the newer armamentarium, such as intraoperative angiography, adjuvant usage of endoscopy and doppler vascular flow assessment. Vascular mapping is another option wherein the flow assessment within the perforators, as well as the parent and branching vessels, can be both visually and quantitatively analyzed, thereby safeguarding the risk of post-operative vasospasm. Moreover, this study can help dichotomize high-risk patients with decreased absorption intensity (AI) and increased time to appearance of the dye; for early initiation of anti-spasmodic therapy like "Triple-H" and calcium channel blockers.[6]
During the initial retraction of the frontal lobe, the recurrent artery of Heubner is usually the first artery to be noted even before the A1 segment, since it courses anterior to the A1 in 60% of cases.[7] During aneurysm surgeries, the surgeon may find it challenging to differentiate the recurrent artery of Heubner from the orbitofrontal artery (OFA). The most straightforward way to distinguish between them is to observe their course. The recurrent artery of Heubner will usually follow the path of the A1 segment, whereas the orbitofrontal artery typically courses perpendicularly over the gyrus rectus and across the olfactory tract.[8]
Clinical Significance
The recurrent artery of Heubner can be affected by various pathologies such as:
- Large artery disease due to greater than 50% stenosis of large vessels such as the carotid artery
- Small vessel disease secondary to hypertension, diabetes, and hypercholesterolemia
- Cardiac emboli following atrial fibrillation, cardiac hypokinesis, mural thrombus, and dilated cardiomyopathies
- Trauma predisposing to the dissection of the vessel as well as the microthrombi formation
- Vasospasm following a ruptured aneurysm
- Inadvertent clipping during microsurgical clipping of anterior communicating artery aneurysm
- Dissecting aneurysm of the recurrent artery of Heubner (e.g., in a patient with osteogenesis imperfecta)[9]
- Vascular malformations like cavernoma
There are varied clinical spectra of presentation ina patient following diminished blood supply owing to damage to the recurrent artery of Heubner and are categorizable into:
- Hemiparesis with fasciobrachiocrural predominance
- Dysarthria due to the involvement of the corticolingual and the corticostriatocerebellar pathways
- Choreoathetosis
- Behavioral changes like abulia or hyperactivity due to interruptions between the associative cortex with the deep cortical regions
- Aphasia in left-sided involvement
- Left visual neglect in right-sided involvement
The neurological abnormalities analyzed in one study following vascular lesions in the caudate region, in the decreasing order of frequency in one study were[10]:
- Abulia
- Frontal lobe abnormalities
- Speech deficits in patients with left-sided lesions and
- Neglect syndromes in those with right-sided lesions
The diagnosis of the involvement of the recurrent artery of Heubner is diagnosable with the aid of plain computerized tomography of head revealing hypodensity in the caudate region in cases of infarction and hyperdensity in cases with hemorrhage. The ultra-early diagnosis of the infarction in the caudate region due to the involvement of the recurrent artery of Heubner can be facilitated with magnetic resonance imaging (MRI) of the brain with special sequences such as diffusion-weighted images (DWI) and apparent diffusion coefficient (ADC).
The endovascular approach has a dual advantage in that it can diagnose the vasospasm in the selected vessels as well have the benefits of simultaneous therapeutic benefits through the application of stents and vasodilators.
Other Issues
Differential diagnosis of the involvement of the head of the caudate nucleus includes the involvement of the following[10]:
- Recurrent artery of Heubner supplying the inferior part of the head of the caudate nucleus and the anterior limb of the internal capsule
- Anterior lenticulostriate arteries originating from the A1 segment of ACA and supplying the anterior area of the head of the caudate nucleus and
- Lateral lenticulostriate arteries originating from the MCA and supplying a significant portion of the head of the caudate nucleus, anterior internal capsule, and putamen.