Retinal Detachment
- Article Author:
- Kyle Blair
- Article Editor:
- Craig Czyz
- Updated:
- 8/8/2020 8:20:03 PM
- For CME on this topic:
- Retinal Detachment CME
- PubMed Link:
- Retinal Detachment
Introduction
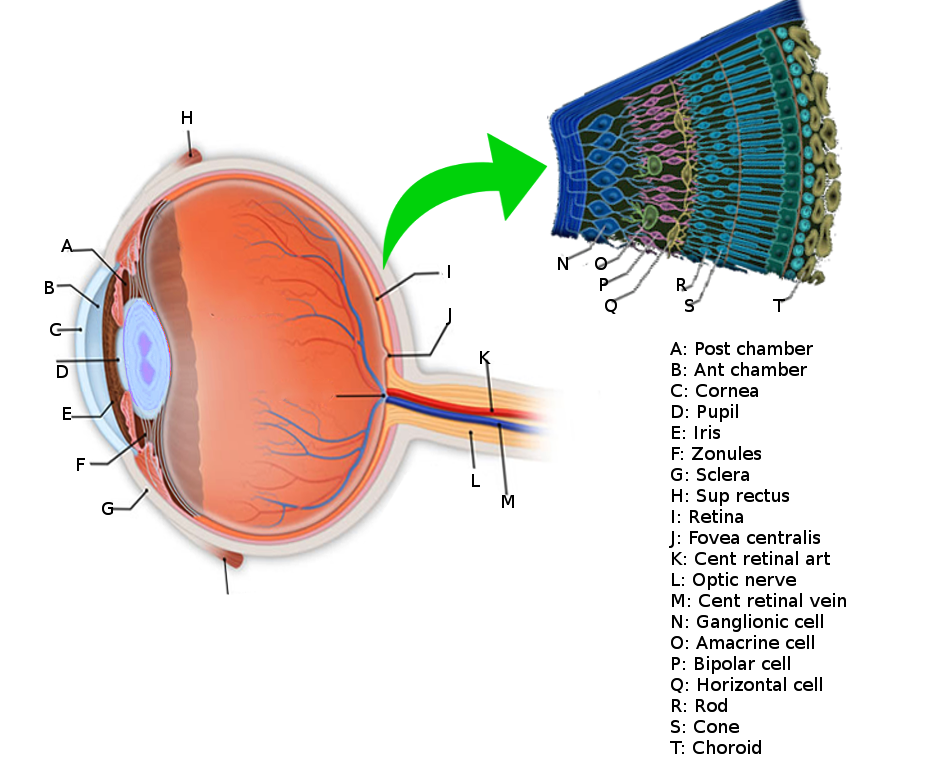
The retina is the innermost layer of tissue of the posterior portion of the eye. It is composed of multiple cellular layers. The outermost layer abuts the vitreal cavity and the innermost layer, the choroid. Retinal detachment is when the neurosensory retina loses adherence to the underlying retinal pigment epithelium (RPE). The outer portion of the neurosensory retina is where the photoreceptors lie. The choroid supplies the oxygen and nutrition for the photoreceptors. Within the fovea, there are no retinal blood vessels, and retinal tissue within this area depends entirely on the choroid for its oxygen requirements. A detachment of the macula can lead to permanent damage to the photoreceptors in this location. Vision is potentially retainable if the macula remains attached, and the retina gets appropriately reattached. However, if the macula comes off, vision may remain poor despite surgical intervention.
There are three categories of retinal detachment: rhegmatogenous, tractional, and exudative. Rhegmatogenous retinal detachments are the most common and are caused by fluid passing from the vitreous cavity via a retinal tear or break into the potential space between the sensory retina and the RPE. Tractional detachments occur when proliferative membranes contract and elevate the retina. Components of rhegmatogenous and tractional etiologies may also lead to retinal detachment. Exudative detachments result from fluid accumulation beneath the sensory retina caused by retinal or choroidal diseases.
Etiology
Risk factors for breaks or tear in the neurosensory retina that can lead to a rhegmatogenous retinal detachment:[1][2][3]
- Lattice degeneration
- Peripheral retinal excavations
- Meridional folds
- Enclosed ora bays
- Pathologic myopia
- Previous intraocular surgery
- Trauma
- Previous retinal detachment in the other eye
- Family history
Risk factors for the formation of proliferative membranes that cause tractional retinal detachments:[4][5]
- Proliferative diabetic retinopathy
- Proliferative vitreoretinopathy
- Sickling hemoglobinopathies
- Trauma
- Retinal vein occlusion
- Retinopathy of prematurity
Risk factors or causes for fluid entering the subretinal space and thus causing an exudative or serous retinal detachment:[6][7][8][9][10][11][12][13][14][15][16]
- Primary ocular tumors
- Ocular metastases
- Sarcoidosis
- Syphilis
- Toxoplasmosis
- Sympathetic ophthalmia
- Central serous chorioretinopathy
- Polypoidal choroidal vasculopathy
- Tuberculosis
- Corticosteroid therapy
- Vogt-Koyanagi-Harada syndrome
- Pre-eclampsia, eclampsia
- Organ transplantation
- Optic nerve pit
- Acute retinal necrosis
- Coats disease
Epidemiology
The incidence of rhegmatogenous retinal detachment varies between studies from 1 in 10000, and another showing the annual risk of rhegmatogenous retinal detachment to be between 6.3 and 17.9 per 100000.[17] Males may be at a slightly higher risk than females of getting a rhegmatogenous retinal detachment.[18] There may be a higher risk of rhegmatogenous retinal detachments in Southeastern Asians compared to European White race persons, confounded by the fact that Southeastern Asians tended to have a higher risk of myopia and a longer axial length.[19] Another study did not find a significant difference in risk factors in patients with retinal detachments between Indians, Malays, and Chinese in Singapore.
Pathophysiology
There are three classifications of retinal detachments: rhegmatogenous retinal detachment, tractional retinal detachment, and exudative retinal detachment.
A rhegmatogenous retinal detachment is when a tear, break, or hole occurs in the retina. When a break occurs, this may allow vitreous to enter the space underneath the neurosensory retina, causing a detachment from the RPE. The fluid continues to enter underneath the retina so that it peels off from the RPE until the entire posterior retina is detached. This detachment can occur over hours to months, depending on the location of the detachment. A detachment of the retina can lead to severe vision loss, and often without surgical intervention, it can be a permanently blinding condition.
Tractional retinal detachments do not include a break in the neurosensory retina. When there are proliferative membranes in the vitreous or on the retinal surface, these membranes can pull on the neurosensory retina. When the force is strong enough, it can separate the neurosensory retina from the underlying RPE.[20]
Exudative or serous retinal detachments also do not involve a break in the neurosensory retina. In these detachments, subretinal fluid accumulates due to fluid exudation from a large lesion, such as a tumor or inflammatory mediators.[21]
History and Physical
Patients with a rhegmatogenous retinal detachment may present with a history of a large number of new-onset floaters. They may also have significant photopsia (flashes of light) in their vision.[22] The patient often presents with slowly progressive or fixed visual field loss, typically starting in the periphery and then moving centrally. Other essential aspects of the history include the timing of the onset of the symptoms, if the patient has the same visual loss symptoms in the fellow eye, whether central visual acuity is affected, prior surgery, or previous trauma. The clinician should obtain a complete review of systems and past medical history.
Essential aspects of the physical exam include getting the patient's best-corrected visual acuity of each eye, checking the pupillary reaction of each eye and ensuring that there is no relative afferent pupillary defect,[23] and confrontational visual field testing. Checking the intraocular pressure is also helpful.
The practitioner should complete a slit lamp examination of the anterior segment to look for any abnormalities. A dilated fundoscopic examination should then follow. Important findings include pigment in the anterior vitreous (Schaffer sign) or vitreous hemorrhage. An ophthalmologist or optometrist should repeat the fundoscopic examination with indirect ophthalmoscopy with scleral depression so that the entire retina is visualizable up to the ora Serrata and the examiner can identify any breaks or tears.[24][25] If areas of the posterior pole cannot be visualized or the entire view is obstructed, a B-scan ultrasound should be used to evaluate for detachment.
Evaluation
Any patient with suspected retinal detachment should undergo a dilated fundoscopic examination by an ophthalmologist or optometrist. Other modalities to assist in the diagnosis of a retinal detachment include ultrasound,[26] CT scan, and MRI.[27] Point-of-care ultrasound in the hands of an experienced provider can be an effective way of diagnosing a retinal detachment, with one meta-analysis showing a sensitivity of 94.2% and specificity of 96.3%.[28] If available, optical coherence tomography (OCT) can be an effective way to assess all three types of retinal detachments and differentiate a detachment from other retinal pathology.[29]
If a patient has a retinal detachment that is likely rhegmatogenous, Linkoff's rules, as outlined below, should be followed to find the retinal break.
- In detachments located superior temporally or superior nasally, the main break is located within 1.5 clock-hours of the highest border 98% of the time.
- In total or superior detachments that fall across the 12:00 meridian, there are two likely possibilities. The first is that the main break is located at 12:00. The second is that the break is a triangle, with the apex of the triangle at the ora serrata, and the sides extend one half clock hours to either side of 12:00. One of these options occurs 93% of the time.
- For inferior detachments, 95% of the time, the higher side of the attachment indicates which side of the optic nerve at the inferior break lies. For example, if the detachment is higher nasally, then the break is likely nasal, as well.
- Detachments that form inferior bullae originate from a break superiorly.
Treatment / Management
Management of rhegmatogenous and tractional retinal detachments is typically surgical. Exudative macular detachments usually have nonsurgical management. The recommendation is that the patient work with a retinal specialist, an ophthalmologist with additional training in evaluation and surgical treatment of the posterior portion of the eye.
If the patient has a rhegmatogenous retinal detachment, the surgeon should identify and seal all retinal breaks or tears. Three main techniques can be used to achieve closure: pars plana vitrectomy, scleral buckle, or pneumatic retinopexy. These techniques can also be combined. Factors that play into the decision of which technique to use include the patient's presentation, surgeon's training, and cost.[30] There are varying opinions on which procedure is the most effective, although there are situations where a specific procedure may be more advantageous to use than another.[31][32][33][34]
A vitrectomy is the mechanical removal of the vitreous gel with a vitrectomy machine. The retinal surgeon typically puts three ports through the pars plana portion of the eye. One port is for the lighting, one port is for the vitreous cutter, and one port is for the infusion cannula. The surgeon then can remove vitreous tractioning on the retina and uses cryotherapy or laser around retinal breaks or tears to prevent the worsening of the detachment.[35]
A scleral buckle is a silicone band wrapped around the globe permanently, sliding under the extraocular rectus muscles causing scleral indentation, which closes retinal breaks. Often a retina surgeon combines this with a retinopexy procedure (reattachment of the retina), typically cryopexy.
In pneumatic retinopexy, an intraocular gas bubble is injected into the eye to allow the subretinal fluid to reabsorb and a chorioretinal adhesion to form around the causative break or tear. A variety of intraocular gases are useful for tamponade, with the most common being air, SF6, or C3F8. Once the gas is in place, and retinal apposition occurs, the surgeon will perform transconjunctival retinopexy. This procedure often can be done in a clinic setting with a compliant patient. Following the procedure, patients may need to position their face down so that the gas bubble can tamponade the retinal tear. Typically, pneumatic retinopexy is only used in retinal detachments with a single break less than one clock hour in size with the break localizing to the superior eight clock hours, absence of proliferative vitreoretinopathy, and confidence that all retina breaks or tears have been identified.
In tractional detachments, tractional elements (usually epiretinal or subretinal membranes) must be relieved, which typically takes place with pars plana vitrectomy, but may be combined with scleral buckling as an adjunct.[36]
For serous detachments, management is nonsurgical. The underlying retinal or choroidal disease or mass should be identified and treated.
Differential Diagnosis
The differential for suspected retinal detachment includes:
- Retinoschisis[37]
- Choroidal effusion
- Choroidal mass
- Suprachoroidal hemorrhage
The clinician can differentiate these with a dilated fundoscopic exam and appropriate imaging techniques. If the patient has a quadrantanopia or hemianopia in both eyes, a cerebrovascular event should be in the differential.[38] Rhegmatogenous retinal detachment should be on the differential for anyone who has a tractional retinal detachment.[39]
Prognosis
The prognosis of a retinal detachment varies greatly on the type of detachment and patient presentation. For a rhegmatogenous retinal detachment, one of the most important prognosticating factors is whether or not the macula remains attached. If the macula is attached, one study showed that 83% of patients had a best-corrected visual acuity of 20/40 or better.[40] If the macula remains attached, the time to surgery does not change the final visual outcome.[41] If the macula is detached, however, the visual prognosis is relatively poor. A study reported that 37% of patients recovered to 20/50 or better visual acuity with surgical intervention within the first week. Surgical intervention in individuals with a macula-off detachment should occur within the first week. However, it does not have to take place as an emergent case in the first 24 hours. The patient likely will have a worse visual outcome if there is submacular fluid on OCT. The phakic status of a patient does not seem to play a role in visual prognosis after a retinal detachment.[42]
Tractional retinal detachments have a varied visual prognosis. The final visual outcome depends on the underlying cause of the tractional detachment and if there are confounding issues affecting the vision. Exudative retinal detachments also have variable visual prognosis based on the underlying condition.[43][44]
Complications
Proliferative retinopathy (PVR) occurs in around 8-10% of patients with a primary retinal detachment repair, and it constitutes the most common cause of repair failure. Retinal pigment epithelium, glial, and other cells form membranes after they migrate and grow onto the outer and inner surfaces of the retina and vitreous. These membranes often contract, causing equatorial traction, detachment of the non-pigmented epithelium from the pars plana, generalized retinal shrinkage, and fixed retinal folds. The patient may be at higher risk for PVR if they are older, have giant retinal tears, retinal detachments involving more than two quadrants, vitreous hemorrhage, a choroidal detachment, had a previous retinal detachment repair, or if using cryotherapy.
Deterrence and Patient Education
Patients should be educated not to wait to be seen by an ophthalmologist or optometrist if they are having changes in their vision. Vision loss from a retinal detachment can be permanent, and patients should be made aware of this. If patients receive a diagnosis of rhegmatogenous retinal detachment, surgery will likely be necessary. Thorough education about the surgical process can help alleviate fears about having surgery. Educating patients may help improve compliance with the treatment and result in an optimal surgical outcome; this may be especially important following a pneumatic retinopexy, where they may have to remain in a face-down position so that the gas bubble can tamponade the retinal detachment effectively.[45]
Enhancing Healthcare Team Outcomes
Excellent communication among allied health professionals working as an interprofessional team is essential to treating patients with retinal detachments, especially since patient outcomes can be time-sensitive. A careful medical history is necessary during the evaluation of a retinal detachment. As with any acute loss of vision, ophthalmology should be consulted as soon as possible. A rhegmatogenous retinal detachment constitutes an ocular emergency, and clinicians should make the consult to ophthalmology in a timely fashion.[46] The medical provider should assess the best-corrected visual acuity, pupil reactivity, and confrontational visual fields of both eyes. An ophthalmologist with retinal surgical training should ultimately direct treatment. Patients often make the referral to receive treatment for a retinal detachment faster if they have a macula on retinal detachment.[47]
It is important to refer patients to a retinal specialist or tertiary care center as soon as possible, as a referral from optometrists via general practitioners and local ophthalmic clinics can delay treatment leading to reduced outcomes.[48] [Level III]
Following with diagnosis and treatment of a retinal detachment, the care of the patient may involve a multitude of medical disciplines. Disabling decreased vision may require the involvement of physical and occupational therapy. Depending on the underlying etiology of the retinal detachments, specialists including but not limited to endocrinology, neurology, infectious disease, rheumatology, or hematology/oncology may need to evaluate the patient. Specific ophthalmologic subspecialties that may be necessary for consult include the retina, uveitis, ocular oncology, pediatric ophthalmology, neuro-ophthalmology, and glaucoma. Regardless of the underlying cause, it is crucial that the patient follow-up with her or his regular ophthalmologist and/or vitreoretinal surgeon to prevent future complications and help control risk factors. Opthalmology specialty-trained nurses can assist in both surgical and non-surgical treatment. They will help with surgical prep and post-operative care, as well as counseling patients and acting as a point of contact and bridge between the clinician and patient, along with monitoring treatment progress in all cases, and reporting to the treating clinician. Open and transparent interprofessional communication between team members can lessen the morbidity of retinal detachment. [Level 5]
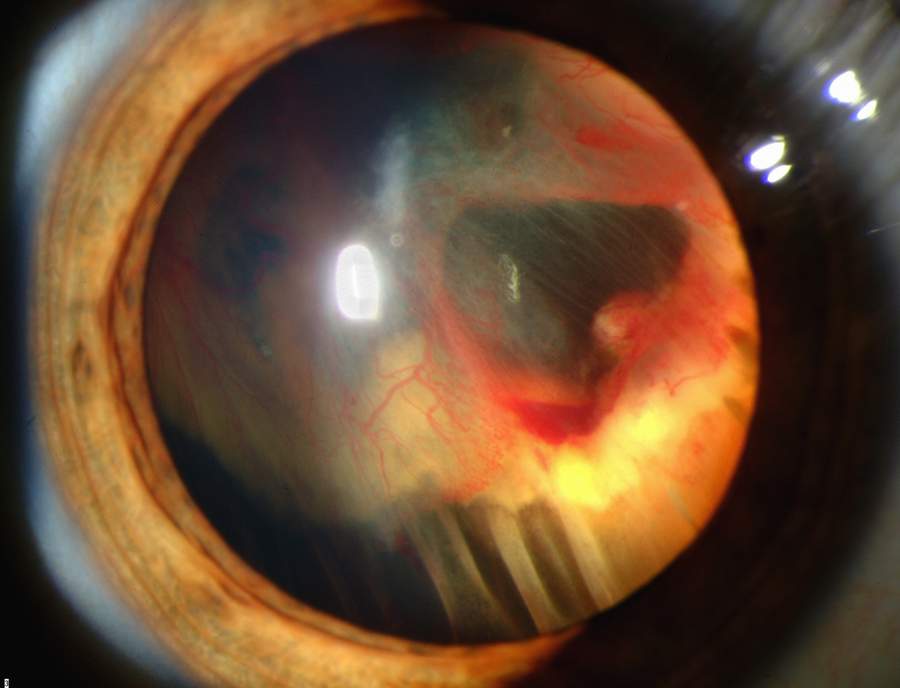
(Click Image to Enlarge)
Contributed by Harry J. Goett
(Click Image to Enlarge)