Rotator Cuff Syndrome
- Article Author:
- Matthew Varacallo
- Article Author:
- Youssef El Bitar
- Article Editor:
- Scott Mair
- Updated:
- 7/20/2020 10:41:45 AM
- For CME on this topic:
- Rotator Cuff Syndrome CME
- PubMed Link:
- Rotator Cuff Syndrome
Introduction
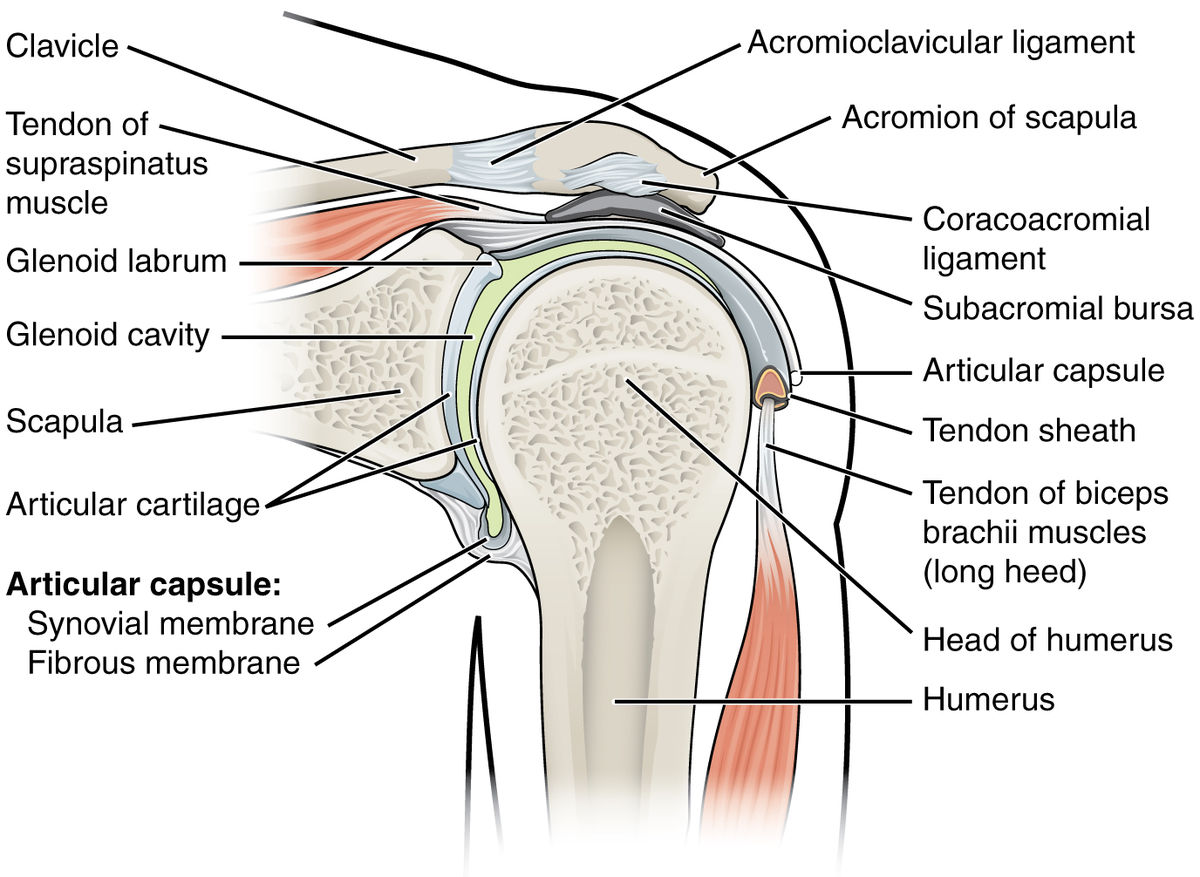
The rotator cuff (RC) is an anatomic coalescence of the muscle bellies and tendons of the supraspinatus (SS), infraspinatus (IS), teres minor (TM), and subscapularis (SubSc). Rotator cuff syndrome (RCS) constitutes a spectrum of disease across a wide range of pathologies associated with injury or degenerative conditions affecting the rotator cuff (RC).
RCS includes subacromial impingement syndrome (SIS) and bursitis, RC tendonitis, partial- versus full-thickness RC tears (PTTs versus FTTs), and, chronically, can influence the development of glenohumeral degenerative disease (DJD) and rotator cuff arthropathy (RCA).[1][2][3][4]
Etiology
The relationship between SIS and rotator cuff syndrome (RCS) remains controversial.[1][2][3][4]
Terminology
In order to best understand the clinical association of these conditions, one must first appreciate the constellation of symptoms implied by each clinical diagnosis and its associated terminology.
- Rotator cuff (RC) tendonitis/tendinosis: acute or chronic tendinopathic conditions that result from a vulnerable environment for the rotator cuff secondary to repetitive eccentric forces and predisposing anatomical/mechanical risk factors.
- Acute injuries and chronic overuse can result in focally weakened cuff regions. These vulnerable areas evolve into PTTs or FTTs, depending on the type of eccentric forces experienced by the rotator cuff .[1]
- Shoulder impingement: a clinical term often used nonspecifically to describe patients experiencing pain/symptoms with overhead activity.
- Internal impingement:[5] common in overhead-throwing athletes such as baseball pitchers and javelin throwers. Impingement occurs at the posterior/lateral articular side of the cuff as it abuts the posterior/superior glenoid rim and labrum when the shoulder is in maximum abduction and external rotation (i.e., the “late cocking” phase of throwing)
- The term, "thrower's shoulder" refers to a common set of anatomic adaptive changes that occur over time in this subset of athletes.
- These adaptive changes include but are not limited to increased humeral retroversion and posterior capsular tightness.
- Glenohumeral internal rotation deficit (GIRD) is a condition resulting from these anatomic adaptations, and GIRD is known to predispose the thrower's shoulder to internal impingement.
- External impingement: a term used synonymously with subacromial impingement syndrome . External impingement (EI) encompasses etiologies of external compressive sources (i.e. the acromion) leading to subacromial bursitis and bursal-sided injuries to the RC.[2][3][4]
One must also appreciate the historical and evolving theories behind the etiology and pathophysiology of the RCS clinical spectrum:
Extrinsic Compressive theories
Historically, the popular theory for the etiology of RCS cited extrinsic compression factors as the primary source for the onset of the pathophysiologic cycle. Extrinsic factors consist of anatomic entities that cause direct injury to the cuff.[3] Historically, Watson-Jones described the pathologic abutment of the lateral acromion on the RC during mid-arc shoulder abduction.[3] Neer later popularized and modified the theory of degenerative acromial spurring and advocated for the clinical importance of the anterior aspect of the acromion as the predominant source of impingement. Neer's classic report in 1972 suggested that 95% of RC tears occurred secondary to the aforementioned mechanical site of impingement.[6] In addition to the anterior spurring, the coracoacromial ligament (CAL) can become calcified in chronic SIS and can serve as another source of extrinsic compression on the cuff.[3] Bigliani later highlighted the importance of acromial morphology, especially the hooked-type acromion, in the predisposition of patients developing SIS.[6] Several studies later documented an association between the hooked-type acromial morphology and the presence of impingement symptoms and full-thickness RC tears.[7][8] Other possible anatomical causes include AC joint degenerative changes[9] subacromial spurs[10], and in much rarer instances, symptomatic os acromiale.[11]
After Neer's proposal regarding the prevalence of extrinsic compressive sources as the primary driving force causing injury to the RC, a decade later he coined promote his theories linking RC injury, extrinsic compression, and subacromial impingement syndrome (SIS).[12] SIS implies extrinsic compression secondary to a narrowing of the subacromial space. As knowledge of extrinsic compression has evolved, a particular subset of patients exhibiting a variation in RC pathology was becoming documented in the literature with increasing incidence rate recognition. Internal impingement occurs secondary to the pathologic abutment of the articular side of the RC, between the posterior/superior glenoid rim and greater tuberosity of the humerus with the arm in maximum shoulder abduction, external rotation, and extension.[13][14] In effect, the theory behind internal impingement provided an important distinction with respect to external compressive forces and a narrowed subacromial space, as these patients did not demonstrate a pathologically narrowed acromiohumeral interval.
Intrinsic degenerative theories
Intrinsic degenerative RC theories advocate for another set of etiological factors as the primary source of pathology leading to the clinical presentation of patient-reported symptoms. Although the opposing theories existed as early as the 1930s, with Codman and Akerson proposing intrinsic tendon degeneration of the RC,[15] more extensive evidence began to surface as multiple reports in the 1990s demonstrated increasing evidence to support increasing degenerative RC changes seen in association with increasing patient age.[16][17]
In general, the intrinsic degenerative theories cite the that cuff degeneration eventually compromises the overall stability of the glenohumeral joint. With the dynamic stability compromised, the humeral head migrates superiorly, and the subacromial space decreases in size. Thus, the cuff becomes susceptible to secondary extrinsic compressive forces which ultimately leads to cuff degeneration and tearing:[3][18]
Vascular changes
Several studies have identified regions of hypovascularity in the RC tendons which may lead to attritional degeneration of the cuff. Lohr et al. initially demonstrated a distal area of the SS tendon on the articular side that lacks blood vessel supply in a cadaveric study.[19] Rudzki et al. demonstrated an age-dependent manner of increasing degrees of hypovascularity in this tendinous region as well.[16] However, controversy proposed by other studies supports that the attritional areas develop secondary to the preceding impingement mechanisms. Subsequently, EI/SIS leads to blood vessel damage, ensuing ischemia, tenocyte apoptosis and gross tendinopathy, and attritional cuff damage.[20] Furthermore, many studies cite increased vascularity in focal areas of the cuff, and the hypervascularity has been associated with age-related changes, tendinopathy, and PTTs and/or FTTs.[21][22]
Age, sex, and genetics
Histologically, age-related RC changes include collagen fiber disorientation and myxoid degeneration.[23] The literature favors increasing frequencies of RC abnormalities with increasing age. The frequency of RC abnormalities increases from 5% to 10% in patients’ younger than 20 years of age to 30% to 35% in those in their sixth and seventh decades of life and tops out at 60% to 65% in patients’ over 80 years of age.[24][18][25]
Tensile forces
A study by Budoff et al. proposed that the primary mode of failure of the cuff occurs as a result of eccentric tension repeatedly imposed on the RC.[26]
RCS also can be seen in association with glenohumeral instability, PTTs and RC fatigue over time (especially with overhead overuse), and posterior capsular contractures.[5][27][28] The subacromial bursa degenerates and eventually loses its physiologic protective potential for the cuff. As a consequence of the degenerative process, the bursa serves as another source of mechanical compression.[4]
Environmental factors
Sports and occupation
Various social and environmental factors predispose patients to developing RCS over time. Occupational mechanical risk factors include manual laborer positions requiring significant heavy lifting, constant overhead working requirements,[29] and repetitive work activities in general.[30] Miranda et al. reported a 20-year follow-up study of a cohort of workers in Finland that demonstrated the synergistic effect of multiple occupational mechanical risk factors in the development of RCS and/or shoulder pain. Pertinent factors included occupational force requirements, the posture of the shoulder during the actual work, and overhead activity requirements.[31] As alluded to earlier, overhead activities in sports such as throwing also predispose patients to the development of RCS.[5]
Smoking
Multiple studies in the literature have supported a dose- and a time-dependent association between smoking and RC tears. A 2010 study investigated 586 subjects with unilateral shoulder pain, noting almost two-thirds of the RC tear subgroup having a documented current or history of smoking.[32] Other studies have suggested a correlation between smoking and RC degeneration, symptomatic cuff tears, and even the increase in the size of the cuff tear when present.[33][34]
Medical comorbidities
Multiple medical conditions play a potential role in the development and exacerbation of RCS. Metabolic syndrome and its associated diagnoses (i.e., dyslipidemia, hypertension, hyperglycemia, and abdominal obesity) have known associations with RC pathology.[35][36] The individual medical conditions of metabolic syndrome itself, in addition to thyroid disorders, diabetes, and inflammatory arthritides, are considered additional risk factors for RCS.[37][38][39][40]
Contemporary etiologies for RC pathology
We now appreciate that most RC tears occur in the anterior half of the supraspinatus tendon, typically initiating about 1cm from its insertional footprint on the greater tuberosity. This area has been termed the "anterior critical zone" [41][42]. This critical zone of hypovascularity has been attributed to our contemporary knowledge and appreciation that the majority of RC tears originate at the articular side [43].
Epidemiology
The prevalence of rotator cuff syndrome (RCS) and its associated pathologies affects millions of patients on a global scale.[18] Shoulder pain accounts for approximately 4.5 million office visits and about $3 billion in healthcare costs in the United States alone.[44] RCS afflicts patient populations in an age-dependent fashion, from 5% to 10% of patients younger than 20 years of age to over 60% in patients over age 80 years. Overall, chronic shoulder pain in the adult population has a 67% lifetime prevalence rate.[24][18][45] SIS is considered the most common cause of acute and chronic shoulder pain.[3][18] The literature supports an equal incidence of RCS and RC tears when comparing male and female populations.[46][47]
Pathophysiology
-
The extrinsic compressive theory of SIS supports the inciting factors leading to SIS to be anatomic and/or mechanical in nature. These structures result in increased pressures and pathologic contact, leading to a susceptible and tendinopathic cuff. Extrinsic mechanisms include:
- Subacromial impingement syndrome
- Internal impingement
-
The intrinsic theory of SIS cites the predisposition for a weakened cuff which degenerates over time. Age, hand-dominance, vascular changes, and repetitive eccentric forces cause the cuff to weaken over time, compromising the dynamic stability of the shoulder. Consequently, the humeral head migrates proximally and decreases the acromiohumeral interval, predisposing the cuff to further injury and degeneration. Intrinsic mechanisms include:
- Tendon vascularity (the anterior critical zone of the supraspinatus tendon)
- Tendon biology
- Tendon mechanical properties
- Tendon morphology
- Genetic predisposition
Histopathology
Rotator cuff syndrome (RCS) histologic changes include the following[21][22][23][25]:
- Rounded tenocytes (apoptosis)
- Extracellular matrix disorganization and myxoid degeneration
- Vascular changes (focal hypervascularity; focal hypovascular regions as well)
- Reduced total cellularity
- Calcified depositions
- Collagen fiber thinning
- Degenerative acromion, CAL
History and Physical
Clinicians evaluating patients with acute or chronic shoulder pain should obtain a comprehensive history. Characteristics of rotator cuff syndrome (RCS) include
- Atraumatic, insidious onset of pain
- symptom exacerbation with overhead activity
- Pain at night
A thorough history includes current or history of sports participation (as well as specific positions played in each sport), occupational history and current status of employment, hand dominance, any history of injury/trauma to the shoulder(s) and/or neck, and any relevant surgical history.
Physical Examination Pearls
C-spine / neck exam:[48]
Co-existing cervical radiculopathy should be ruled out in any situation where neck and/or shoulder pathology is in consideration. Observation of neck posturing, muscular symmetry, palpable tenderness, and active/passive ROM should be evaluated. Special tests that are helpful in this regard include the Spurling maneuver, myelopathic testing, reflex testing, and a comprehensive neurovascular exam.
Shoulder exam:[3][18][49][50][51]
Clinicians must observe the overall shoulder girdle for assessment of symmetry, shoulder posturing, and overall muscle bulk and symmetry. Scapular winging should also be ruled out. The skin should be observed for the presence of any previous surgical incisions, lacerations, scars, erythema, or induration.
After the observational component of the physical examination, the active and passive ROM are documented. In cases of RCS, patients may demonstrate compromised active ROM but should normally exhibit full passive ROM. In the absence of advanced degenerative changes affecting the glenohumeral joint, limited passive ROM is considered diagnostic for adhesive capsulitis and involves a separate treatment algorithm from RCS/impingement.
The clinician can assess motor strength grading for C5 to T1 nerve roots in addition to specific RC muscle strength testing. Specifically, RC strength and/or pathology can be assessed via the following examinations:
Supraspinatus (SS)
- Jobe’s test: positive test is pain/weakness with resisted downward pressure while the patient’s shoulder is at 90 degrees of forward flexion and abduction in the scapular plane with the thumb pointing toward the floor.
- Drop arm test: the patient’s shoulder is brought into a position of 90 degrees of shoulder abduction in the scapular plane. The examiner initially supports the limb and then instructs the patient to slowly adduct the arm to the side of the body. A positive test includes the patient’s inability to maintain the abducted position of the shoulder and/or an inability to adduct the arm to the side of the trunk in a controlled manner.
Infraspinatus (IS)
- Strength testing is performed while the shoulder is positioned against the side of the trunk, the elbow is flexed to 90 degrees, and the patient is asked to externally rotate (ER) the arm while the examiner resists this movement.
- External rotation lag sign: the examiner positions the patient’s shoulder in the same position, and while holding the wrist, the arm is brought into maximum ER. The test is positive if the patient’s shoulder drifts into internal rotation (IR) once the examiner removes the supportive ER force at the wrist.
Teres Minor (TM)
- Strength testing is performed while the shoulder positioned at 90 degrees of abduction and the elbow is also flexed to 90 degrees. Teres minor (TM) is best isolated for strength testing in this position while ER is resisted by the examiner.
- Hornblower’s sign: the examiner positions the shoulder in the same position and maximally ERs the shoulder under support. A positive test occurs when the patient is unable to hold this position and the arm drifts into IR once the examiner removes the supportive ER force.
Subscapularis (SubSc)
- IR lag sign: the examiner passively brings the patient’s shoulder behind the trunk (about 20 degrees of extension) with the elbow flexed to 90 degrees. The examiner passively IRs the shoulder by lifting the dorsum of the handoff of the patient’s back while supporting the elbow and wrist. A positive test occurs when the patient is unable to maintain this position once the examiner releases support at the wrist (i.e., the arm is not maintained in IR, and the dorsum of the hand drifts toward the back)
- Passive ER ROM: a partial or complete tear of the subscapularis (SubSc) can manifest as an increase in passive ER compared to the contralateral shoulder.
- Lift off test: more sensitive/specific for lower SubSc pathology. In the same position as the IR lag sign position, the examiner places the patient’s dorsum of the hand against the lower back and then resists the patient’s ability to lift the dorsum of the hand away from the lower back.
- Belly press: more sensitive/specific for upper subscapularis pathology. The examiner has the patient’s arm at 90 degrees of elbow flexion, and IR testing is performed by the patient pressing the palm of his/her hand against the belly, bringing the elbow in front of the plane of the trunk. The elbow is initially supported by the examiner, and a positive test occurs if the elbow is not maintained in this position upon the examiner removing the supportive force.
External impingement/SIS
- Neer impingement sign: positive if the patient reports pain with passive shoulder forward flexion beyond 90 degrees.
- Neer impingement test: positive test occurs after a subacromial injection is given by the examiner and the patient reports improved symptoms upon repeating the forced passive forward flexion beyond 90 degrees.
- Hawkins test: positive test occurs with the examiner passively positioning the shoulder and elbow at 90 degrees of flexion in front of the body. The patient will report pain when the examiner passively IR’s the shoulder.
Internal impingement
- Internal impingement test: the patient is placed in a supine position, and the shoulder is brought into terminal abduction and external rotation. A positive test reproduces the patient’s pain.
Evaluation
Radiographic imaging should be obtained in all patients with acute or chronic shoulder pain.
Radiographs[3]
Recommended imaging includes a true anteroposterior (AP) image of the glenohumeral joint (i.e., the “Grashey” view). The true AP image is taken with the patient rotated between 30 and 45 degrees offset the cassette in the coronal plane. Alternatively, the beam can be rotated while the patient remains neutral in the coronal plane. The distance between the acromion and the humeral head (i.e., the acromiohumeral interval) can be calculated. A normal interval is between 7 and 14 mm, and this interval is decreased in cases of advanced degenerative arthritis and RCA.
Other radiographic imaging includes a 30-degree caudal tilt view that can be performed to visualize the presence of acromial spurring. In addition, the “scapular Y” or “supraspinatus outlet” view is used to determine acromial morphology.
Pertinent findings
The most common radiographic changes associated with EI/SIS and RCS include:
- RCA: Proximal humeral migration and decreases in the acromiohumeral interval to < 7 mm
- Degenerative findings:
- osteophytes on the acromion, proximal humerus and/or glenoid are often seen in cases of advanced disease
- calcification of the CAL and/or coracohumeral ligament (CHL)
- greater tuberosity cystic degeneration
- AC joint arthritis
- “Hooked” acromion: best appreciated on the supraspinatus outlet view
- Os acromiale: best seen on an axillary lateral radiograph
Ultrasound[18]
Ultrasound (US) is an often-underutilized imaging modality to detect RC tendon and muscle belly integrity. In 2011, a meta-analysis of over 6,000 shoulders revealed a sensitivity of 0.96 and specificity of 0.93 in assessing shoulders for partial- or full-thickness cuff tears. Another study highlighted the potential inability to differentiate between partial- and full-thickness cuff tears (PTT versus FTT) measuring about 1 cm in size.
Magnetic Resonance Imaging[3]
Magnetic Resonance Imaging (MRI) is useful in evaluating the overall degree of RC pathology. MRI can be helpful in providing more accurate cuff tear details, including partial- versus full-thickness tears, the extent and size of the tear(s), location, and the degree of retraction. In cases of chronic RC pathology, the cuff can be assessed for fatty degenerative changes on the T1-weighted sagittal sequence series.
Subdeltoid and/or subacromial bursitis can also be evident and are important considerations as potential sources of pain. In addition, the acromioclavicular (AC) joint, acromial morphology, and long head of the biceps (LHB) tendon integrity are better appreciated. A systematic approach to reviewing shoulder MRIs is important, especially when correlating the MRI findings with the patient reported symptoms and clinical examination.
Treatment / Management
Given the complex nature of rotator cuff syndrome (RCS), we recommend the treatment and management be broken down into the following categories:
Group 1: Partial-Thickness (PTTs) or Full-Thickness RC Tears (FTTs), Asymptomatic Patient[52]
Patients presenting with MRI-evidence of PTTs or FTTs often present without any symptoms. The most recent American Academy of Orthopaedic Surgeons (AAOS) clinical practice guideline (CPG) summary reported the growing awareness of incidental RC pathology revealed via shoulder MRIs in asymptomatic patient populations. Although there is evidence of increasing prevalence of RC disease in the aging population, there is no reliable evidence that surgical intervention prevents tear propagation or the development of clinical symptoms. Thus, the committee recommended symptomatic management via nonoperative modalities alone.
Group 2: Partial-Thickness (PTTs), Symptomatic Patients[1][52]
Patients presenting with symptoms of EI/SIS in the absence of FTTs are first managed with nonoperative treatment modalities. There is no agreed upon time interval that is most appropriate to proceed with surgical intervention in this particular group of patients. The literature ranges from 3 months to 18 months. Surgical intervention should be individually tailored based on the patient’s symptoms, improvement with nonoperative modalities, and overall goals.
Group 3: Chronic RC Tears, Symptomatic Patients [52]
The AAOS CPG reported a “weak” recommendation grade secondary to limited available evidence in the literature comparing rotator cuff repair (RCR) to continued nonoperative treatment modalities in this subset of patients. Certainly, the overall clinical picture must be considered, and the treatment tailored to the individual patient in each scenario.
Nonoperative RCS Treatment Modalities[1][52]
Physical therapy (PT)
- Physical therapy (PT) remains the mainstay of first-line treatment for RCS. PTTs can often be managed with PT alone, including an aggressive RC and periscapular stabilizer strengthening programs, as well as ROM exercises.
Anti-inflammatory medications
- First-line nonoperative management also includes the use of non-steroidal anti-inflammatory (NSAIDs) medications in conjunction with PT modalities.
- Although the AAOS CPG reported inconclusive evidence for the use of NSAIDs, iontophoresis, transcutaneous electrical nerve stimulations (TENS), and other similar therapy modalities in the presence of FTTs, the committee reported a “moderate” recommendation grade for exercises and/or NSAIDs in the presence of RCS symptoms in the absence of FTTs.
Cortisone injections
- For EI/SIS, the most utilized injection includes one into the subacromial space. Patients can experience symptomatic relief almost instantaneously after the injection is given, ideally allowing them to participate in subsequent PT therapy sessions.
Rest/Activity modifications
- Patients benefit from an initial period of rest from the exacerbating activity (occupation or sport), especially repetitive overhead activity and heavy lifting
Surgical management
RCS surgical techniques range from debridement, subacromial decompression (SAD), and/or acromioplasty to RC debridement and, when indicated, RC bursal- or articular-sided tear completion with RCR. The latter will not be discussed in this review. Assuming no RC FTTs are present, the extent of surgical management for external impingement/SIS alone includes:[1][3][11][52][53]
Subacromial decompression
- Extensive debridement of the subacromial space is beneficial in patients with persistent symptoms of EI/SIS after at least 4 to 6 months of failed nonoperative modalities
- Comprehensive bursectomy allows for thorough and more accurate evaluation of the bursal side of the cuff itself
- CAL debridement is recommended in the setting of substantial CAL fraying and/or calcification as this is considered an additional source of impingement.
- A meta-analysis of nine studies comparing open versus arthroscopic procedures yielded equivalent surgical times, outcomes, and complication rates at 1-year follow-up; the arthroscopic cohort returned to work quicker compared to the open cohort.
Acromioplasty
- Shaving the undersurface of the acromion, especially in the setting of significant spurring, improves the environment surrounding the cuff and allows additional clearance distance between the acromion and cuff itself throughout mid-arc and terminal ROM and impingement positions.
- With hooked acromion morphologies, care is taken to debride this area with a shaver, burr, or rasp to flatten the undersurface.
- The anterior extent of the acromioplasty is demarcated by the anterior deltoid origin. This area should be respected in the debridement process. The anteroinferior region of the acromion is a common site of spurring and causes impingement symptoms in these patients.
Os Acromiale
- With persistent symptoms, a two-stage procedure is often utilized. First, the os acromiale is fused using bone grafting techniques, followed by a formal acromioplasty after healing is achieved.
Differential Diagnosis
The differential diagnosis for chronic shoulder pain includes several etiologies:
Impingement
- External/SIS
- Subcoracoid
- Calcific tendonitis
- Internal (including SLAP lesions, glenohumeral internal rotation deficit (GIRD), Little league shoulder, posterior labral tears)
RC pathology
- Partial- versus full-thickness tears (PTTs versus FTTs)
- RCA
Degenerative
- Advanced DJD, often associated with RCA
- Glenohumeral arthritis
- Adhesive capsulitis
- Avascular necrosis (AVN)
- Scapulothoracic crepitus
Proximal biceps
- Subluxation – often seen in association with SubSc injuries
- Tendonitis and tendinopathy
AC joint conditions
- AC separation
- Distal clavicle osteolysis
- AC arthritis
Instability
- Unidirectional instability – seen in association with an inciting event/dislocation (anterior, posterior, inferior)
- Multidirectional instability (MDI)
- Associated labral injuries/pathology
Neurovascular conditions
- Suprascapular neuropathy – can be associated with paralabral cyst at the spinoglenoid notch
- Scapular winging – medial or lateral
- Brachial neuritis
- Thoracic outlet syndrome (TOS)
- Quadrilateral space syndrome
Other conditions
- Scapulothoracic dyskinesia
- Os acromiale
- Muscle ruptures (pectoralis major, deltoid, latissimus dorsi)
- Fracture (acute injury or pain resulting from long-standing deformity, malunion, or nonunion)
Prognosis
The majority of patients with rotator cuff syndrome (RCS) in the absence of FTTs improve with nonoperative management. The most recent AAOS CPG touted a “moderate” recommendation grade for initial treatment of NSAIDs and/or exercises programs based on multiple level II studies in the literature.
In 2013, The MOON shoulder group provided insight into the management and outcomes of atraumatic, FTT of the RC. In a cohort of almost 500 patients, nonoperative treatment resulted in 75% reporting positive patient-reported outcomes at 2-year followup. In addition, the patients electing to undergo surgery (25%) typically decided to do so between 6- and 12-weeks following the initial onset of symptoms.
Complications
Complications associated with rotator cuff syndrome (RCS) are best broken down into nonoperative- versus operative-related complications:
Nonoperative management:
- Persistent pain/recurrent symptoms
- In the setting of PTTs, there is at least a theoretical risk of tear propagation, lack of healing, fatty infiltration, atrophy, and retraction.
- Overall a controversial topic, a 2017 study analyzed independent risk factors for symptomatic RC tear progression over a 19-month period of nonoperatively managed shoulders; risk factors for tear progression included:
- The initial presence of an FTT
- Medium-sized cuff tears (1 to 3 cm)
- Smoking
- While PTTs were included in the study, the presence of a PTT was not a risk factor for cuff tear progression
- In the setting of chronic/atrophic tears, especially with RC tear propagation, degenerative joint disease and RCA ensue
Surgical management:
- Surgical treatment tends to be most effective in patients that have failed or reported persistent or worsening symptoms despite at least 4 to 6 months of exhaustive nonoperative treatment modalities
- The standard risks of surgery, including recurrent pain/symptoms, infection, stiffness, neurovascular injury, and risks associated with anesthetic use
- SAD/acromioplasty
- Deltoid dysfunction: can occur secondary to failed deltoid repair following an open acromioplasty or excessive debridement during arthroscopy
- Anterosuperior escape: occurs secondary to aggressive CAL release – the coracoacromial arch and suspensory system becomes compromised, and with CAL release in the setting of massive, retracted, and irreparable RC tears, the humeral head migrates superiorly and anteriorly to compromise patient functional outcomes
Postoperative and Rehabilitation Care
Following SAD/acromioplasty (without RCR), patients are kept in a sling for 1 to 2 weeks with early passive ROM rehabilitation parameters. Clinicians should recognize the risk of overutilization of sling immobilization, especially when soft tissue repair protocols do not have to be respected.
Initially, patients are instructed to avoid heavy lifting and exercises to facilitate soft tissue healing. Cryotherapy devices are often applied for the first 10 to 14 days postoperatively. Physical therapy is often started postoperatively once the sling is discontinued.
Full active ROM should be achieved by 3 to 6 weeks maximum. If applicable, return to sport-specific skills at 6 to 8 weeks as tolerated.
Consultations
Primary care medical doctors can manage the majority of cases of rotator cuff syndrome (RCS), especially along the nonoperative management spectrum. After these modalities are exhausted, an appropriate referral can be made to an orthopedic surgeon. While the nonoperative management is not conclusively managed with a supervised physical therapy protocol, a supervised protocol is recommended in the postoperative setting to regain maximum ROM and full strength.
Deterrence and Patient Education
Patients should be educated about the nature of the condition as well as the possibility of continued chronic pain following surgical management for persistent impingement/rotator cuff syndrome (RCS) symptoms.
Enhancing Healthcare Team Outcomes
Rotator cuff syndrome (RCS) is a clinical entity consisting of a wide range of clinical symptoms, ranging in severity from mild shoulder impingement, but eventually in the long-term setting, can lead to progressive partial-thickness cuff tears (PTTs) and/or full-thickness cuff tears (FTTs). The disorder is best managed by an interprofessional team consisting of clinicians and surgeons.
When clinicians are working up acute or chronic shoulder pain, it is imperative to correlate the clinical examination with radiographic imaging, MRI, and response to nonoperative treatment modalities. The latter consists of physical therapy, NSAIDs, rest/activity modification, and injections.
For patients managed conservatively, the pharmacist should educate the patient on pain management. In addition, the physical therapist should educate the patient on beneficial exercises that can improve muscle strength and joint mobility.
Surgical management is considered after impingement symptoms fail to resolve or worsen after all other management modalities are exhausted. Referral to an orthopedic surgeon should be considered, especially with long-standing persistent symptoms.
Close communication with the members of the team is essential to ensure improved patient outcomes.