Scapholunate Advanced Collapse
- Article Author:
- Robert Lane
- Article Author:
- Dawood Tafti
- Article Editor:
- Matthew Varacallo
- Updated:
- 7/2/2020 5:36:54 PM
- For CME on this topic:
- Scapholunate Advanced Collapse CME
- PubMed Link:
- Scapholunate Advanced Collapse
Introduction
Scapholunate advanced collapse (SLAC) describes a characteristic degenerative clinical wrist condition of progressive instability, deformity, and arthritis affecting the radiocarpal and midcarpal joints of the wrist. [1] Specifically, the characteristic pattern of arthritic deformity and progressive instability occurs secondary to a long-term, chronic dissociation between the lunate and the scaphoid carpal bones. [2] SLAC wrist is often the terminal and end-stage result from an untreated scapholunate interosseous ligament (SLIL) injury. Radiographic, CT, and MRI imaging often demonstrate widening of the scapholunate interval, degenerative changes of the affected carpal bones, and proximal migration of the capitate. [3] A four stage categorization to grade arthrosis is often used. [4] Treatment most commonly includes four-corner arthrodesis, capitolunate arthrodesis, and scaphoidectomy. [5]
Etiology
Chronic SLIL injuries often result secondary to trauma although they can also occur in association with other degenerative or inflammatory arthritic conditions of the wrist. [6][7] Many clinical presentations are either initially under-appreciated or may be acutely diagnosed as a "wrist sprain." Football linemen are particularly prone to "acute on chronic" repetitive SLIL injuries as these contact athletes are subject to high impact, forced wrist dorsiflexion movements for several years. [8] As SLAC arthritis progresses and untreated scapholunate interosseous ligament (SLIL) injury worsens, the scaphoid changes shape and position. This leads to an increased mechanical burden on the capitate, which subsequently migrates between the lunate and scaphoid over time.
Epidemiology
SLAC is the most common degenerative condition of the wrist.[9] The incidence of acute injury to the scapholunate ligament occurs in approximately 10% to 30% of intra-articular distal radius fractures. [10] One study evaluating the epidemiology of SLAC wrist noted that patients were more often males, had a history of wrist trauma, engaged in a manual job, and were often younger when compared to carpometacarpal osteoarthrosis. [11]
Pathophysiology
There is a well-established and recognized pathologic sequential algorithm for SLIL and SLAC wrist. The SLIL is a key stabilizer of the wrist and is a critical intercalating stabilizer to ensure normal, physiologic motion of the carpal bones, specifically the scaphoid and lunate bones. [12]
As the normal opposing forces at the SL interval are lost, the scaphoid assumes an abnormally flexed position, while the lunate pathologically deviates into extension. [13] This condition results in a dorsal intercalated segment instability (DISI deformity) pattern. The scapholunate angle increases to greater than 70 degrees while the lunate is extended to greater than 10 degrees beyond neutral. These abnormal flexion and extension positions alter the distribution of forces across the midcarpal and radiocarpal joints. Eventually, cartilage degeneration occurs beginning with the radioscaphoid joint (recognized on radiographs at the radial styloid).
The pathologic cascade continues in an ulnar-based direction, with the final iteration yielding the collapse of the capitate proximally between a widened SL interval (known as the "Terry Thomas sign"), and end-stage patterns include capitolunate arthritis. [14] Of note, the radiolunate joint remains spared in the SLAC pattern of degenerative deformity.
Histopathology
The SLIL consists of three regions of the dorsal, proximal, and palmar regions. The dorsal and palmar regions histologically represent true capsular ligaments. The proximal region is made of fibrocartilage with occasional collagen fascicles. The dorsal region is histologically composed of transversely oriented collagen fascicles and is surrounded by connective tissue containing neurovascular bundles. [15]
History and Physical
When a patient presents after a fall on an outstretched hand, the clinician should consider the possibility of a SLIL injury. These injuries can be seen in isolation, in the absence of fractures, but they can be present in association with distal radius and/or scaphoid fractures. Up to 30% of distal radius fractures have some degree of injury to the SL region. Aside from wrist trauma, SLIL secondary injuries may occur from other falls on the ipsilateral extremity (e.g., a fall on the elbow, for example), SLIL compromise secondary to underlying inflammatory arthritis, or SLIL iatrogenic compromise that may occur following excessive capsular excision when removing dorsal ganglion cysts. [16] [17]
Patients will likely present with some degree of pain although not all SLAC wrists are symptomatic. Pain is common and may be aggravated by heavy use and is sometimes associated with a clunking sensation during movement. [13] There will usually be a decreased wrist ROM and weakness of the grip strength.
The external appearance of scapholunate instabilities may not be evident. Even in the acute phase, swelling may be moderate. When the patient presents with scapholunate advanced collapse, however, pain with provocative movements will usually be present. A scaphoid shift test is the passive mobilization of the dysfunctional scapholunate joint. This test is valuable not only in determining the presence of abnormal radioscaphoid subluxation but also in reproducing the patient's pain and the reason they are presenting to the doctor. [18] A positive scaphoid shift test is said to be diagnostic of scapholunate instability.
To perform the (Watson) scaphoid shift test, firm pressure is applied to the palmar tuberosity of the scaphoid while the wrist is moved from ulnar to radial deviation. In normal wrists, the scaphoid cannot flex because of the external pressure by the examiner's thumb. A positive test is seen in a patient with a scapholunate tear or a patient with a lax wrist. When pressure on the scaphoid is removed, the scaphoid goes back into position, and a typical snapping occurs.
A scapholunate ballottement test can also be performed. [19] The lunate is firmly stabilized with the thumb and index finger of one hand, while the scaphoid, held with the other hand is displaced dorsally and palmarly with the other hand. A positive result elicits pain, crepitus, and excessive mobility of the scaphoid.
Evaluation
Imaging begins with standard PA and lateral wrist radiographs. [3] Bilateral clenched-fist comparison views may reveal a DISI with a relative widening of the scapholunate interval on the affected side. This radiograph should be taken and appreciated acutely in the disease process as possible.
SLAC wrist will have a pattern of arthrosis which shows the progression of the injury. Localized arthrosis of the scaphoid fossa begins at the styloid tip (radial styloid beaking) which is indicative of a Stage I SLAC wrist. Progressive joint space narrowing and sclerosis affecting the entire scaphoid fossa of the distal radius is indicative of Stage II SLAC wrist. Stage III SLAC wrist entails sclerosis and joint space narrowing between the lunate and capitate. Eventually, the capitate will migrate proximally into the space created by the scapholunate dissociation. Stage III SLAC wrist is synonymous with "Terry Thomas sign." The lunate may fall into dorsiflexion (dorsal intercalated segment instability), and the scaphoid into flexion but the integrity of the radiolunate articulation is preserved until late in the process.
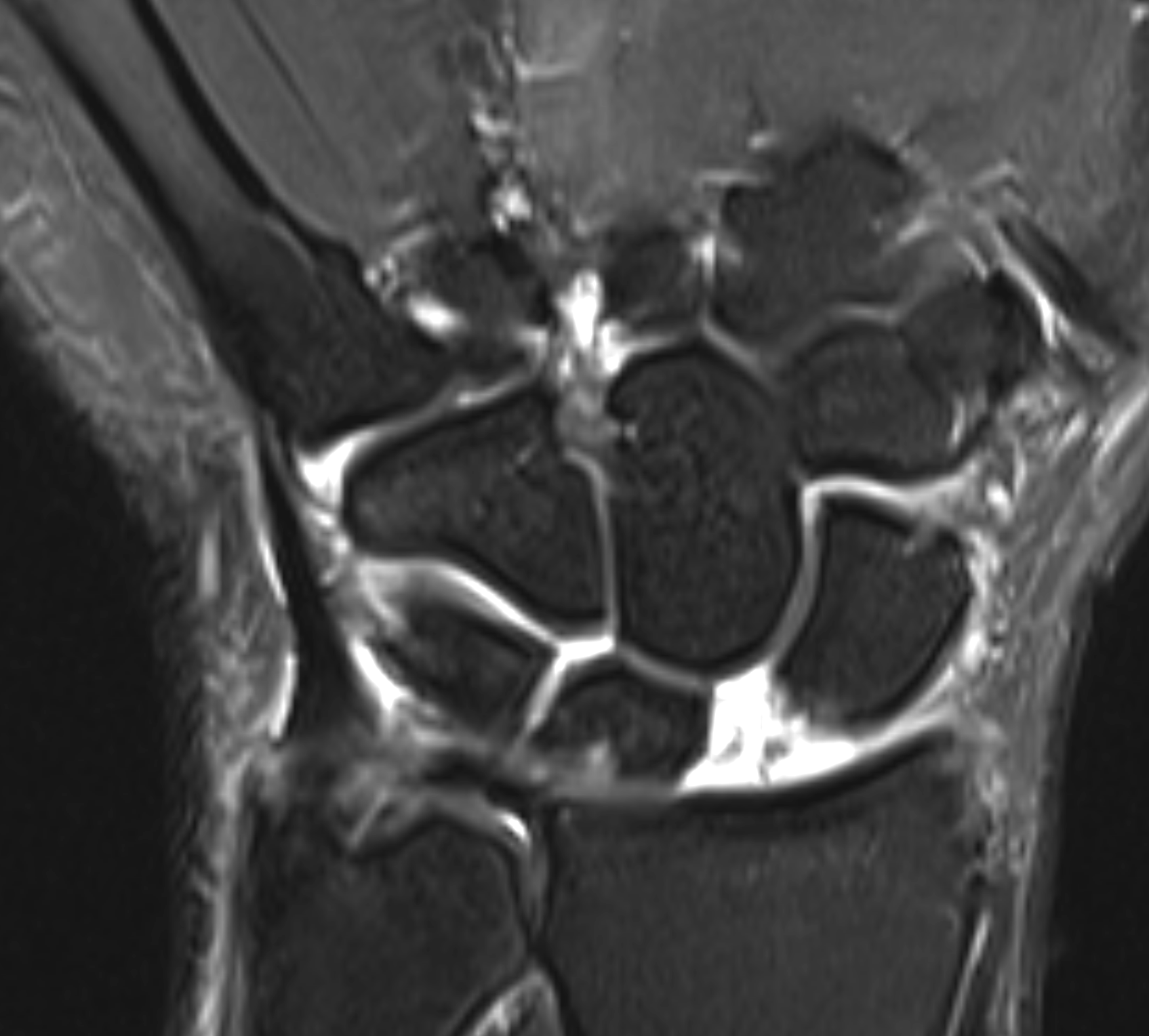
Advanced Imaging Modalities
While CT scans are often not indicated, MRI scans may facilitate diagnosis in subtle clinical presentations. However, the latter are also often not necessary as radiographs are often sufficient. When obtained, an MRI may reveal thinning of the articular surfaces of the proximal scaphoid. It may also show synovitis of the scaphoid facet of the distal radius and capitolunate joint as well as the overall radiocarpal and midcarpal joints. Sagittal images can demonstrate abnormal changes in the position of the scaphoid and lunate bones and can also demonstrate radioscaphoid incongruity.
Treatment / Management
Treatment of scapholunate advanced collapse is difficult and not always predictable. Nonoperative treatment can include NSAIDS, wrist splints, and possible corticosteroid injections for mild disease.
Operative treatments include[20][21][22][23][24]:
- Stage I SLAC wrist
- Radial styloidectomy and scaphoid stabilization procedures
- PIN and AIN denervation
- Stage II SLAC wrist
- Proximal row carpectomy (PRC) is indicated to treat Stage II (but not Stage III) SLAC wrist.
- Note that a PRC procedure is contraindicated in Stage III deformity given that this implies an element of capitolunate arthritis, and patients inevitably report inferior outcomes in this clinical scenario
- Proximal row carpectomy (PRC) is indicated to treat Stage II (but not Stage III) SLAC wrist.
- Stage III SLAC wrist
- Scaphoid excision and four corner fusion
- Produces reliable, positive outcomes in patients suffering from debilitating Stage II or Stage III SLAC wrist deformity
- Outcomes are equivalent in the long-term when comparing this procedure to a PRC in Stage II SLAC wrist deformity
- Wrist fusion
- Indicated in the setting of Stage III SLAC wrist or pancarpal arthritis
- Wrist fusion procedures result in positive outcomes with respect to pain relief, but wrist motion is compromised compared to scaphoid excision/four corner fusion (the latter demonstrates preserved wrist motion following surgical reconstruction via the lunate/distal radius articulation at the lunate fossa)
- Scaphoid excision and four corner fusion
Differential Diagnosis
The differential diagnosis for SLAC wrist and SLIL injury is broad and includes various causes of wrist pain:
- Scaphoid fracture
- Distal radial fractures
- Dorsal ganglion cyst
- Septic arthritis
- Avascular necrosis of the scaphoid
- Gout
- Psuedogout
- Rheumatoid arthritis
- Tear of the triangular fibrocartilage complex
- Kienbock's disease
- Tenosynovitis
- Lunate fracture vs dislocation
- Dorsal intercalated segmental instability
Of note, many of the differentials described above, such as crystalline arthropathies, for example, can secondarily lead to SLAC wrist.
Staging
Classification is broken down to 4 stages. Stage 1 demonstrates radial styloid degenerative changes. Stage 2 is represented by degenerative changes that involve the scaphoid fossa and the styloid. Stage 3 has lunocapitate degenerative changes. Stage 4 is the last stage. Pancarpal arthritis is indicative of stage four; however, this is somewhat controversial because some surgeons do not believe scapholunate advanced collapse will result in pancarpal arthritis. Nevertheless, the radiolunate facet is always spared of arthrosis in scapholunate advanced collapse. [25]
Prognosis
Most cases of scapholunate advanced collapse are in the beginning stages of progressive carpal destabilization around the lunate and result from an injury involving wrist hyperextension, ulnar deviation, and midcarpal supination. Postoperative prognosis is fairly good. In one study, 91% of patients were satisfied with their post-operative result and would undergo the operation again, while 80% returned to their jobs. [26]
Complications
Complications do exist for operative interventions and include possible infection, failure of fusion, and the need for additional procedures. Ashmead et al. studied 100 patients who had surgically treated SLAC wrist and noted an average flexion/extension arc of 53% and grip strength of 80% of the uninjured wrist. [26] A nonunion rate of 3% was noted, and all of these cases healed after bone graft revision. A meta-analysis has shown a nonunion rate of 4.3%. [27] In another systematic review, the most common complication reported was dorsal radiocarpal impingement representing 4.4% of cases with an overall complication rate of 13.5%.
Postoperative and Rehabilitation Care
After a four-corner fusion, patients should be immobilized in a short-arm volar splint for 2 weeks, at which point a custom splint is worn for an additional 6 weeks or until radiographic evidence of healing is confirmed. [28]
Gentle finger range of motion and strengthening are started at 2 weeks, but wrist motion and strengthening are not initiated until there is radiographic confirmation of union.
Patients should expect a 50% loss in wrist range of motion compared with the contralateral side. Grip strength should return to about 80% of the unaffected side. [29]
Deterrence and Patient Education
Most cases of SLAC wrist involve a chronic scapholunate ligament injury that has slowly progressed to collapse. During an initial presentation, especially after diagnosis of scapholunate injury with imaging, an in-depth conversation with the patient is necessary to emphasize the long term complications to include eventual collapse.
Pearls and Other Issues
Acute traumatic SLIL injuries can often be repaired despite even the most traumatic injuries resulting in an obliterated state of ligamentous integrity. In conditions caused by underlying arthritic conditions and inflammatory arthritis, the ligamentous and other pericapsular soft tissue structures are of significantly poor quality and can compromise overall healing and patient-reported outcomes. [27]]
Enhancing Healthcare Team Outcomes
Scapholunate advanced collapse requires strong interprofessional communication between the patient, the doctor, and the hand therapists involve in care. The operations needed to treat this process are typically complex procedures that will require hand therapy post-operatively. Managing patient expectations is also critical. Four-corner arthrodesis is a complex procedure that can have long term implications on a patient's occupational functionality. An informed decision with knowledge of outcomes should be discussed with the patient to establish whether a surgery is advisable, especially in those with significant comorbidities. Alternative treatments should also be discussed. A preassessment that includes blood tests, an electrocardiogram, and further imaging to guide surgical course can be obtained. An anesthetic review by an anesthesiologist or certified nurse anesthesist should also be performed in patients with comorbidities, as well as guiding pain relief as appropriate. A physical therapy assessment during the course of recovery is also an important step in the immediate and long term post-operative course. Follow-up clinic visits also play a role in expediting the correction of post-operative complications.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)