Shigella
- Article Author:
- Aysha Aslam
- Article Editor:
- Chika Okafor
- Updated:
- 8/11/2020 11:55:10 PM
- For CME on this topic:
- Shigella CME
- PubMed Link:
- Shigella
Introduction
Shigellosis is a form of bacterial diarrhea caused by gram-negative bacteria Shigella species. It is common in developing countries and results from contaminated food, poor sanitation conditions, or direct person to person contact. Shigella can cause infection in all age groups. High-risk group include very young, elderly, and immunocompromised person. Shigella species is relatively resistant to acid in the stomach, and few organisms are required to cause the disease.[1] Once ingested, it multiplies in the small intestine and enters the colon. In the colon, it produces shigella enterotoxins and serotype toxin 1, resulting in watery or bloody diarrhea. Clinical manifestations usually result within 12 hours to 3 days of ingestion of the organism with an average incubation period of 3 days. These symptoms include high fever, vomiting, diffuse colicky abdominal pain followed by bloody mucoid diarrhea and tenesmus.[2][3][4][5] It self-resolves within 5 to 7 days of onset of symptoms. However, high-risk individuals may end up with complications.
Etiology
Shigellosis is a food-borne or water-borne illness caused by Shigella. Shigella is a gram-negative, nonmotile, facultatively anaerobic, non-spore-forming rod. It has 4 serotypes:
- Serotype A: Shigella dysenteriae (12 serotypes)
- Serotype B: Shigella flexneri (6 serotypes)
- Serotype C: Shigella boydii (23 serotypes)
- Serotype D: Shigella soneii (1 serotype)
Shigella sonnei is different from the other serotypes by the expression of ornithine decarboxylase while serotypes A, B and C cannot be differentiated with any biochemical marker.
Shigella sonnei causes mild disease that may be limited to watery diarrhea while Shigella flexneri and Shigella dysenteriae cause dysentery with bloody diarrhea. [5][6]
Epidemiology
Incidence
The incidence of shigellosis is reported to be one hundred eighty-eight million cases per year with approximately 1 million deaths annually.[7] In developed countries, the incidence is around 1.5 million cases per year. In the United States, it results in about 450,000 cases annually. Most cases reported in the United States are caused by S. sonnei (77%). The serotype responsible for mainly causing disease in developing countries is S. flexneri. It is more common in young children with most cases reported in children (28 cases/100,000 in children) younger than 4 years and 25 cases/100,000 in 4 to 11-year-olds). Shigella is the most common cause of diarrheal illness in children younger than 5 years old in Saharan Africa and South Asia.[8] There is no gender predominance and racial predilection for shigellosis.
Shigellosis is common in daycare centers and residential institutions in the United States.[9] Foodborne transmission has also been reported in the United States.[10] Outbreaks of shigellosis have also occurred in men who have sex with men.[11][12]
Pathophysiology
Route of Transmission
The path of transmission of shigellosis is mostly via the fecal-oral route in developed countries and fecal-oral route, water-borne or food-borne in developing countries. [13] However, it can also be transmitted sexually especially in men who have sex with men [11] [14] or by flies. Humans are the only natural reservoir for shigella.
Size of Inoculum
The number of organisms required to cause the disease is usually 10 to 200 due to the low sensitivity to stomach acid and downregulation of antibacterial proteins of the host by the organism.
Pathogenesis
Once ingested, Shigella enters the small intestine and multiplies then enters the large intestine. Shigella causes cell injury and resulting complications by direct invasion of colonic mucosa and production of enterotoxins.
Direct Invasion of Epithelial Cells
In the large intestine, it invades using transcytosis and transports through basolateral epithelium using M cells which are mainly responsible for immune activation of intestinal lymphoid tissue by antigen recognition.[15] Following transcytosis, it induces macrophages and cellular apoptosis.[16] This results in the release of inflammatory cytokines such as IL-1 and IL-18 which results in intestinal inflammation and subsequent activation of the innate immune system. Shigella is released from the macrophages after following apoptosis and inflammation. It continues to invade the adjacent epithelium and the immune system by using the intercellular actin polymerization process. As Shigella invades the epithelial cells, it activates nuclear factor (kappa B) in the cells causing the production of IL-8 which stimulates recruitment of neutrophils at the site causing more inflammation and epithelial damage. It causes impaired absorption of nutrients causing diarrhea.
Toxin production
Another mechanism for cell injury by Shigella is through the production of enterotoxin 1 and 2 which plays a part in impaired fluid and nutrient absorption causing Shigella-associated diarrhea. Cytotoxin Shigella dysenteriae serotype 1 is responsible for cytotoxicity and vascular lesions in the colon and other organs such as kidneys causing bloody diarrhea and complications such as hemolytic uremic syndrome (HUS).[5]
Histopathology
Microscopic examination of the infected tissue such as colon, rectum, or distal ileum may result in the following findings including polymorphonuclear cells infiltration of the epithelial cells, and the formation of inflammatory patch pseudomembranes. Shigella multiplies in the colonic epithelium leading to cell death. It then spreads laterally to infect and kill adjacent epithelium causing ulceration of mucosa which leads to inflammation and bleeding.[13]
History and Physical
Common symptoms may include mild abdominal discomfort to severe diffuse colicky abdominal pain (70% to 90%). Patient reports of small volume mucoid diarrhea (70% to 80%) that precedes bloody diarrhea (30% to 50%). Other symptoms include fever, nausea, vomiting, anorexia, lethargy, and tenesmus.[17][18][13] Rare but severe symptoms include delirium, encephalopathy, anuria, seizures, meningismus, and coma.[19][20]
Physical examination of patients suffering from shigellosis may indicate lethargic or toxic individuals. Vital signs may reveal fever, tachycardia, tachypnea, and hypotension. An abdominal examination may show a distended abdomen with hyperactive bowel sounds. Tenderness may be present especially in the lower abdomen due to the involvement of sigmoid colon and rectum.
Evaluation
Laboratory Evaluation
- Complete blood count (CBC): Leukocytosis with left shift, leukopenia may also be present.[21][22] Anemia and thrombocytopenia may also be present.
- Stool examination: Stool analysis shows fecal leukocytes and blood. Microscopic evidence of stool examination may show evidence of leukocytes in stool smear. Stool culture gives a better yield than a rectal swab culture.[23]
- Liver function test: Mild elevation of bilirubin may be possible in severe disease.
- Renal function: Elevated BUN and creatinine may be present in dehydrated or very young and elderly patients.
- Hyponatremia: Usually due to the syndrome of inappropriate antidiuretic hormone secretion.[24][25]
- Inflammatory markers: May be elevated such as ESR and CRP
- Blood culture: May be positive in complicated cases and more common in children than adults. Bacteremia is usually associated with an increased mortality rate.[26][27][28]
- Stool alpha-1 antitrypsin: high during the acute phase of shigellosis and remains high in patients that failed medical therapy.[29]
- ELISA and Polymerase chain reaction: May be required in a minority of patients. ELISA usually detects S. dysenteriae type-1 toxin in stool, and PCR may be used to identify the virulent genes of Shigella such as ipaH gene, virF gene, and virA gene.
Treatment / Management
The mainstay of treatment of shigellosis is medical management and includes hydration and electrolyte management. Oral rehydration might be adequate in many cases.
- Antimotility drugs such as loperamide, paregoric or diphenoxylate are not recommended for patients with Shigella infection as they may prolong the infection and increase the shedding of the organism.[30]
- The antibiotic regimen used for the treatment can be divided into two groups based on age. The antibiotic susceptibility testing is highly recommended as resistance to the drugs is common and may vary regionally.
In adults, the choice of empiric antibiotics is based on demographics and regional resistance. Fluoroquinolone is recommended for patients with no risk factors for resistance while a third-generation cephalosporin is recommended in high-risk patients including infected patients in Africa and Asia, international travelers, HIV-infected patients and men having sex with men.[31][14] Antibiotics should be changed once susceptibility result is available. Second-generation cephalosporin, ampicillin, and trimethoprim-sulfamethoxazole can also be used for the treatment of Shigella infection if susceptibility is documented.
In pediatrics, the first-line drug is azithromycin if antibiotic susceptibility is unknown. In a randomized trial, Azithromycin was found to be clinically and bacteriological successful in 82% and 94% of patients treated respectively.[32] Cefixime and ceftibuten can be used as first-line to treat shigellosis in South Asia due to widespread resistance to commonly used antibiotics.[33] The alternative regimen includes pivmecillinam, an extended-spectrum penicillin is effective in decreasing diarrhea duration and eradication of shigella organisms in the stool.[34][35]
Parenteral antibiotics are indicated in children with suspected and proven shigellosis who have a severe infection with signs of bacteremia including lethargy, temperature >39° C (102.2°F), underlying immune deficiency including AIDS and those unable to take oral medications.[27] Ceftriaxone is recommended as a single dose or for five days.
Frequent handwashing with soap and water is recommended especially after bathroom use and before food preparation. Food handlers should not engage in food preparation if stool cultures remain positive. Usually, conversion to negative stool cultures occurs about 2 days after initiation of antibiotic therapy.
Differential Diagnosis
Differential diagnosis of shigellosis include infection with the following organisms due to overlapping symptoms of fever, nausea, vomiting and abdominal pain:
- Nontyphoidal Salmonella
- Escherichia coli infection
- Campylobacter infection
- Clostridium difficile
- Typhoid fever
- Entamoeba histolytica
- Aeromonas
Other diseases causing chronic diarrhea which might be differentiated include:
- Crohn disease
- VIPoma
- Hyperthyroidism
- Lactose intolerance
- Celiac disease
- Irritable bowel syndrome
Prognosis
If diagnosed and treated on time, the prognosis of shigellosis is good, and patients recover without sequelae. However, certain poor prognostic factors include a delay in treatment, immunocompromised state, prolonged duration of disease (more than 7 days), and extremes of age such as elderly and very young individuals can lead to severe disease and complications.
Complications
Complications of shigella infection include intestinal and systemic complications listed below. [5]
Intestinal Complications:
- Colon perforation- Very rare and primarily occurs in infants and malnourished patients. It is associated with S. flexneri and S. dysenteriae 1. [36]
- Intestinal obstruction-usually seen in severe disease and S. dysenteriae 1.[37]
- Toxic megacolon-Usually occurs in S. dysenteriae 1 infection.[24]
- Proctitis or rectal prolapse-Invasion of shigella organisms into colonic mucosa can lead to rectal prolapse and proctitis in infants and young children.[5]
Systemic Complications:
- Bacteremia-Common in young children under the age of 5.[26] [27][28]
- Hemolytic-uremic syndrome-Although uncommon, HUS is the most frequent acute kidney injury in young children and infants.[38]
- Moderate to severe hypovolemia
- Hyponatremia-Usually associated with S. dysenteriae 1 infection.[25]
- Leukemoid reaction-Common in children between ages 2-10 years old.[39]
- Neurologic symptoms-Generalized seizures are the most common neurologic complication. This is usually associated with a higher mortality rate.[40][41]
- Reactive arthritis or Reiter syndrome-Uncommon sterile inflammatory arthritis. It is usually caused by S. flexneri infection. Arthritis can occur alone or in conjunction with conjunctivitis and urethritis.[42]
- Vulvovaginitis with or without diarrhea-Seen in young girls associated with painless vaginal discharge.[43]
- Keratitis-Rare but should be considered in a young child with keratitis and a history of recent diarrheal illness. [44]
- Acute myocarditis-Seen in children with S. Sonnei infection.[45]
Pearls and Other Issues
There is no vaccine to prevent shigellosis. However, the disease can be limited by practicing certain precautions:
- Frequent and careful handwashing with water and soap
- Supervised handwashing of children in daycare centers and homes with children who are not completely toilet trained
- People with shigellosis should not handle food and water for others unless they are disease-free
- In children who wear diapers and have the disease, precautions are required in handling and disposing of diapers
- Drink only boiled or treated water and avoid eating raw poorly handled food from the vendors while visiting developing countries
- Avoid sexual contact with a patient having diarrhea or recently recovered from diarrheal illness
- Practice safe sex
- Avoid swimming pools when infected
Enhancing Healthcare Team Outcomes
The diagnosis of shigellosis often takes time and the infection can be confused with many other abdominal conditions. Thus, it is best managed by an interprofessional team that includes the emergency department physician, infectious disease specialist, gastroenterologist, and internist. The mainstay of treatment of shigellosis is medical management and includes fluid and electrolyte management. The antibiotic regimen used for the treatment can be divided into two groups based on age. Antibiotic susceptibility testing is highly recommended before as resistance to the drugs is common and may vary regionally. Immunity can occur after shigella infection and appears to be serotype-specific.[46][47][48][49]
Because there is no vaccine to prevent the infection, the primary care provider and nurse specialist play a vital role in educating the public about prevention. This includes handwashing with soap and water, maintaining good personal hygiene, drinking boiled water while traveling and avoiding sexual contact with a patient with a recent diagnosis of shigellosis.[50][51]
The outlook for patients who are treated promptly is good but delays in treatment can lead to multiorgan failure and even death.[52] Confirmed cases of shigellosis in the United States should be reported to the Centers for Disease Control and Prevention via state or local health department.
(Click Image to Enlarge)
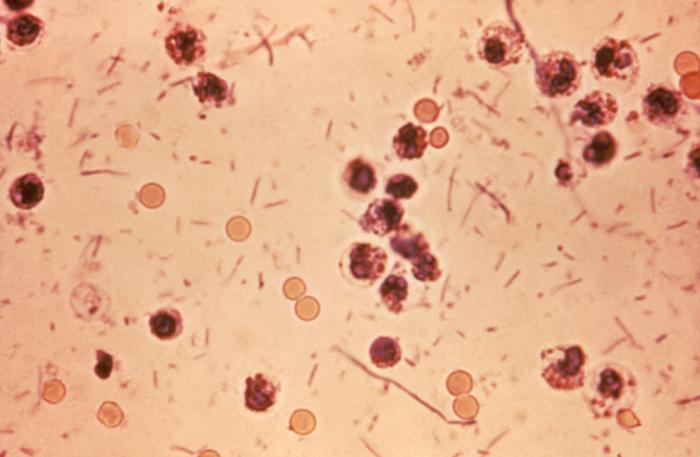
This photomicrograph revealed stool exudates in a patient with shigellosis, which is also known as “Shigella dysentery”, or “Bacterial dysentery”. Usually, those who are infected with Shigella develop diarrhea, which is often bloody, fever, and stomach cramps starting a day or two after they are exposed to the bacterium. Shigellosis usually resolves in 5 to 7 days.
Contributed by The Centers for Disease Control and Prevention (CDC)
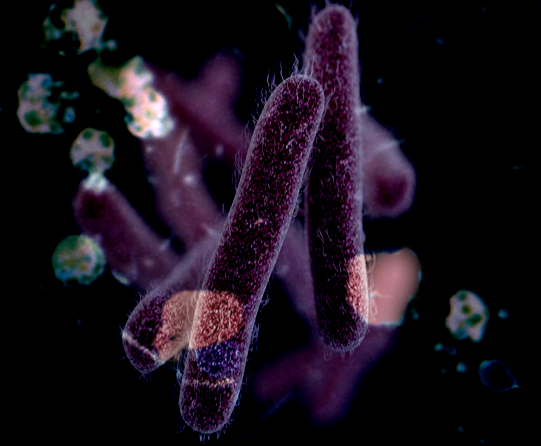
(Click Image to Enlarge)
(Click Image to Enlarge)