Anatomy, Head and Neck, Skull
- Article Author:
- Bradley Anderson
- Article Author:
- Michael Kortz
- Article Editor:
- Khalid Al Kharazi
- Updated:
- 7/27/2020 9:19:20 PM
- For CME on this topic:
- Anatomy, Head and Neck, Skull CME
- PubMed Link:
- Anatomy, Head and Neck, Skull
Introduction
The cranium (Latin term for skull) is the most cephalad aspect of the axial skeleton. It is composed of 22 bones and divided into two regions: the neurocranium (which protects the brain) and the viscerocranium (which forms the face). The skull also supports tendinous muscle attachments and allows neurovascular passage between intracranial and extracranial anatomy. The skull is embryologically derived from mesoderm and neural crest and will fuse, harden, and mold from gestation through adulthood. It gives the human face its form, and even minor variations in anatomy among individuals can lead to wide differences in appearance. Various foramina, condyles, and other bony landmarks provide passageways and attachments for the important structures associated with the skull. Due to its complex development and associated important structures, understanding skull anatomy holds abundant clinical and surgical significance.[1][2][3]
Structure and Function
The skull consists of 22 bones in most adult specimens, and these bones come together via cranial sutures. The function of the skull is both structurally supportive and protective. The skull will harden and fuse through development to protect its inner contents: the cerebrum, cerebellum, brainstem, and orbits. It supports the muscles of the face and scalp by providing muscular and tendinous attachments, protects neurovascular structures, and houses various sinuses to accommodate increases in pressure.
Calvaria and Skull Base
The calvaria, the uppermost part of the skull, protects the cerebral cortex, cerebellum, and orbital contents. It is composed of the frontal bone, parietal bones, temporal bones, and occipital bone. The coronal suture is the transverse mid-anterior junction of the frontal bone and the two parietal bones. The parietal bones articulate with the temporal bones inferiorly via the squamosal sutures and the occipital bone posteriorly via the lambdoid suture. The sagittal suture lies along an anterior-posterior axis and is the articulation of the two parietal bones. The pterion is the articulation of the frontal, parietal, temporal, and sphenoid bones just superior to the pinna. The asterion is the articulation of the parietal, temporal, and occipital bones. Finally, the skull base allows the passage of various neurovascular structures and is composed of the sphenoid bone and ethmoid bone (which have their own associated air sinuses), as well as parts of the frontal, temporal, and occipital bones.
Anteriorly, the frontal bone forms the superior aspect of the orbits. The glabella is a key midline landmark of the frontal bone. It lies superior to the nasion and between the superciliary ridges. The frontal sinuses lie deep to the brow ridges. The bregma is the junction of the coronal and sagittal sutures, and lambda is the junction of the lambdoid and sagittal sutures. The temporal bones subdivide into petrous, squamous, zygomatic, and mastoid parts. The petrous portion houses the inner ear. The mastoid is a bony prominence that lies posterior to the auricle and also has an associated sinus. The occipital bone is the most posterior aspect of the skull.
Intracranial Fossae
There are three cranial fossae with various structural landmarks. The anterior cranial fossa forms from the frontal bone, the sphenoid bone, and the ethmoid bone. The middle cranial fossa forms from the sphenoid bone and two temporal bones. Finally, the posterior cranial fossa forms from the occipital bone and two temporal bones. The critical anatomic landmarks of each fossa are listed below.
- Anterior Cranial Fossa
- Cribriform plate
- Middle Cranial Fossa
- Optic canal
- Superior orbital fissure
- Foramen spinosum
- Foramen rotundum
- Foramen ovale
- Posterior Cranial Fossa
- Internal auditory meatus
- Jugular foramen
- Foramen magnum
- Hypoglossal canal
Facial Bones
There are 14 facial bones with very specific anatomical landmarks and embryologic development mechanisms. These include the two nasal conchae, two nasal bones, two maxilla bones, two palatine bones, two lacrimal bones, two zygomatic bones, the mandible, and the vomer. The maxillae have associated air sinuses. The temporomandibular joint (TMJ) is an especially important landmark for effective mastication, and its dysfunction is common in the adult population.[4][5][6][2]
Embryology
The skull embryologically derives from ectodermal neural crest and mesoderm. The frontal bone, ethmoid bone, and sphenoid bone derive from the neural crest, while the parietal bones and occipital bone originate from mesoderm. The temporal bones derive from both mesoderm and neural crest. The skull develops alongside the rapid growth of the nervous system in the embryonic phase of development (weeks 1 to 8). Ossification and structural molding begin in the fetal phase (week 7 and on).
Early Development
Mesoderm begins to form in the third-week gestation after early mesenchymal cells have migrated through the primitive streak. These cells then proliferate in a longitudinal fashion adjacent to the notochord (paraxial mesoderm) and eventually divide into various early connective tissue populations, including the sclerotome and myotome. The sclerotome develops into the mesodermal portions of the skull (parietal bones, occipital bone, and petrous portion of the temporal bone).
Neural crest cells form the rest of the neurocranium, including the frontal bone, ethmoid bone, sphenoid bone, and squamous portion of the temporal bone, as well as the entirety of the viscerocranium. Five significant pharyngeal arches form in humans, starting rostral to caudal around days 19 to 21 of gestation. These arches form muscles, cartilaginous and osseous structures, nerves, blood vessels, and organs of the head and neck. Each one has components of ectoderm, mesoderm, endoderm, and neural crest. Some of the neural crest components form parts of the viscerocranium previously discussed, including the mandible, maxilla, incus, and malleus (arch 1) and stapes and styloid process of the temporal bone (arch 2).
Several genes play an important role in the formation of the cranium, including the Dickkopf family, matrix metallopeptidase 9, Indian hedgehog, Sonic hedgehog (Shh), Fibroblast Growth Factor 3, and family of collagen genes (i.e., COL1A1).
Fetal Development and Ossification
There are two mechanisms by which bones develop and ossify: intramembranous ossification and endochondral ossification. Intramembranous ossification is the direct formation of early bone from undifferentiated mesenchyme without a template, and endochondral ossification utilizes cartilage as a precursor formed by chondrocytes for bone maturation. The bones of the cranial vault (including the parietal bones, frontal bone, occipital bone, and squamous temporal bone) and viscerocranium (including the maxilla, mandible, and other flat bones of the face) undergo intramembranous ossification. The skull base forms via endochondral ossification (including the sphenoid bone and ethmoid bone). Mesenchymal maturation does not occur until after the formation of the neurovasculature, allowing for the development of the foramina. This process is especially important in the skull base, where nerves and blood vessels exit the cranium.[7][8][9]
Blood Supply and Lymphatics
Most of the blood supply to the skull and its associated structures comes from the common carotid arteries (anterior circulation) and vertebral arteries (posterior circulation). The common carotid artery splits into the internal and external carotid arteries. The external carotid is the main blood supply to the skull bones and meninges. It travels up the side of the neck with eight main branches feeding the superficial structures of the skull and face. Of these branches, the maxillary artery is the most prominent and clinically relevant. The middle meningeal artery is a branch of the maxillary artery, and injury secondary to blunt force trauma to the lateral skull at the pterion can lead to epidural hematoma. The internal carotid has no branches in the neck and enters the base of the skull, supplying intracranial structures. The internal carotid and vertebral arteries combine to form a large anastomosis called the circle of Willis. The anterior communicating artery, two anterior cerebral arteries, two middle cerebral arteries, two posterior communicating arteries, two posterior cerebral arteries, and basilar artery (superior continuation of the vertebral arteries) all contribute to this anastomosis. The dural venous sinuses (i.e., superior sagittal, straight, and transverse sinuses) and superficial and deep veins of the head (i.e., cerebral veins, great vein of Galen, cerebellar, and facial veins) drain into the internal and external jugular veins bilaterally and ultimately to the superior vena cava and right atrium of the heart.
The brain and central nervous system have been traditionally thought not to contain lymphatic vessels. However, some believe that the cerebrospinal fluid (CSF) does have some connection with the lymphatic system and drains through the cervical lymph nodes. The recent discovery of a “glymphatic system,” composed of a network of CSF, interstitial cerebral fluid, and meningeal vasculature, has shed more light on this debate and is an area of ongoing research.[10][11]
Nerves
The skull has multiple foramina that allow passage into and out of the skull for blood vessels and nerves. The cranial nerves mostly exit via foramina in the cranial base. A brief list of the most important foramina and their associated cranial nerves appear below.
- Cribriform Plate → olfactory nerve (CN I)
- Optic Canal → optic nerve (CN II)
- Also: ophthalmic artery
- Superior Orbital Fissure → oculomotor nerve (CN III), trochlear nerve (CN IV), abducens nerve (CN VI), ophthalmic division of trigeminal nerve (CN V1)
- Foramen rotundum → maxillary division of trigeminal nerve (CN V2)
- Foramen Ovale → mandibular division of trigeminal nerve (CN V3)
- Stylomastoid Foramen → facial nerve (CN VII)
- Internal Auditory Meatus → facial nerve (CN VII) and vestibulocochlear nerve (CN VIII)
- Jugular Foramen → glossopharyngeal nerve (CN IX), vagus nerve (CN X), and spinal accessory nerve (CN XI)
- Also: jugular vein
- Hypoglossal Canal → hypoglossal nerve (CN XII)
- Foramen Magnum → brainstem and spinal root of accessory nerve (CN XI)
- Also: vertebral arteries
Other key foramina that may or may not be associated with nerves include the foramen spinosum (middle meningeal artery), carotid canal (internal carotid artery and sympathetic plexus), and supraorbital and infraorbital foramina (supraorbital and infraorbital nerves). The superficial sensory nerves of the skull, scalp, and face receive input from branches of the trigeminal nerve anteriorly and the greater and lesser occipital nerves posteriorly.[12][13][14]
Muscles
The muscles of the face and scalp are predominantly striated muscle under voluntary innervation. They serve crucial roles in facial expression, vision, language, and mastication. The majority of these muscles are innervated by the facial nerve, oculomotor nerve, or trigeminal nerve, while the hypoglossal nerve innervates the tongue. Small smooth muscles of the eye are under sympathetic or parasympathetic control for lens accommodation, aqueous humor production, and other functions.[15]
Physiologic Variants
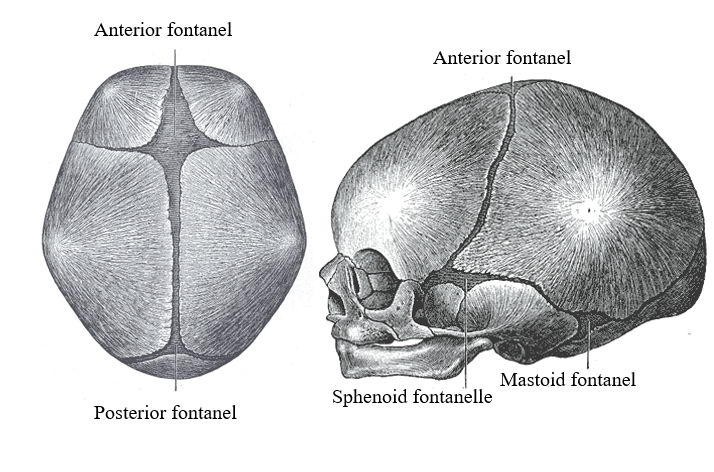
Fontanelles and Cranial Sutures
Fontanelles are soft areas where the skull has not ossified to allow for brain growth and development. There are six fontanelles, with the anterior and posterior being the most prominent and clinically significant. The anterior fontanelle closes around age 1-2 and hardens to become the bregma and adjacent coronal suture. The posterior fontanelle closes around 6-8 weeks of age and becomes the lambda and adjacent lambdoid suture.
The sutures of the skull allow for movement of the cranial bones during infancy, and this persists into adulthood. Eventually, these sutures fuse and are no longer moveable. There is a great deal of variation in the timing of the closure of individual sutures. The sagittal suture closes first around age 22, then the coronal suture, followed by the lambdoid around age 26, and the squamous sutures around age 60. The metopic suture splits the frontal bones and typically closes at three months of age but can take up to 9 months.
Skull Defects and Embryologic Pathophysiology
Skull defects and neural tube malformations (i.e., anencephaly) are unfortunately fairly common due to several factors. Many cranial structures develop early and are vulnerable to toxic insults in unplanned pregnancies where the mother may not be aware of the developing embryo. Folate and other nutritional deficiencies, as well as substance abuse, can hinder development and appropriate growth of the axial skeleton and central nervous system, and in some cases, lead to early miscarriage. Chromosomal abnormalities (i.e., trisomies 13, 18, and 21) and genetic defects (i.e., Shh mutations) are also associated with cranial malformations. Neural crest abnormalities can lead to cleft palate, inner ear problems, or other skull defects. The premature fusion of cranial sutures is termed craniosynostosis and leads to different shapes of the skull (i.e., brachycephaly and plagiocephaly). Treacher-Collins syndrome is a craniofacial disorder due to the interruption of normal embryonic growth. It is a result of a defect in the development of the first and second embryonic arches and presents with mandibular hypoplasia, facial abnormalities, and craniosynostosis. The complex and intricate way in which the skull forms and fits together leave little room for error.[7][8]
Surgical Considerations
Neurosurgeons, ophthalmologists, interventional radiologists, and otorhinolaryngologists all must have a strong understanding of normal and variant skull anatomy. Due to the inability of the skull to accommodate rapid or significant increases in intracranial pressure and the serious deficits that can arise from damage to the skull’s associated anatomy, any etiology including strokes, tumors, fractures, and infections are considered emergent conditions and often require surgical management. A description of two of the most common skull-related surgical operations appears below.
Craniotomy
A craniotomy is the neurosurgical removal of a portion of the skull to gain access to the meninges, brain, and other intracranial structures. Its indications are for the treatment of intracranial hemorrhage, aneurysms, tumors, infection, or congenital malformations. Preoperative imaging is often utilized to localize the pathological entity, but clinical knowledge of the superficial anatomy of the skull and neurovasculature is paramount to ensure adequate exposure and limit intraoperative and postoperative complications.
Transsphenoidal Hypophysectomy
Large (>10 mm), functional, and/or pharmacologic-refractory pituitary adenomas are often surgically managed to prevent long-term morbidity. This procedure is often performed via transsphenoidal resection of the tumor under the management of a neurosurgeon and/or otorhinolaryngologist. The mass can be extracted via the sphenoid sinus with the intraoperative assistance of a surgical microscope or endoscope. If the mass has grown beyond the sella turcica either on preoperative imaging or intraoperatively, an open approach may be necessary.[16][17][18]
Clinical Significance
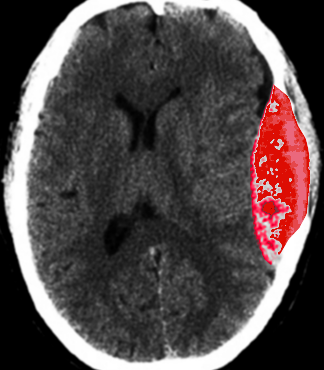
Epidural Hematoma
Epidural hematoma is the result of a lacerated middle meningeal artery, often caused by blunt force trauma to the lateral skull superior to the ear at the pterion. Arterial hemorrhage in the epidural space (a potential space between the dura mater and overlying skull) accumulates quickly and does not cross suture lines. Thus, compression and eventual herniation of the brain can lead to focal neurologic deficits, confusion, and death. Patients will often present with abrupt syncope and then resolution. After a brief lucid interval where the patient may feel normal, significant focal neurologic deficits and signs of increased intracranial pressure may develop. Computed tomography (CT) will display a classic hyperdense “lens-shaped” lesion, and treatment is emergent craniotomy and hematoma evacuation.
Basilar Skull Fractures
Fractures of the skull base should be considered whenever a significant trauma mechanism is involved (most often, a motor vehicle collision). The patient’s presenting signs and symptoms will depend on the location and extent of the fracture. However, patients often present with periorbital ecchymosis (Raccoon eyes) and postauricular ecchymosis (Battle sign), CSF rhinorrhea or otorrhea depending on whether the cribriform plate or petrous temporal bone is fractured, and focal or global neurologic deficits. Thin-slice CT has become an integral part of the diagnosis of subtle skull base fractures.[19][20][21][20]
Other Issues
When interpreting imaging of the skull, a strong understanding of the sutures and their normal variants is needed because of the easy misinterpretation of a suture for a fracture; this is especially true with the increasingly prevalent use of high-resolution CT scans as they can now pick up subtle fractures and the cranial sutures. The anatomy of a child’s skull is continually changing, and these variations are important to note. Clinical correlation is often necessary in these cases.
(Click Image to Enlarge)
(Click Image to Enlarge)