Anatomy, Abdomen and Pelvis, Sphincter of Oddi (Hepatopancreatic Sphincter)
- Article Author:
- Abdelwahab Ahmed
- Article Editor:
- Toby Zuchelli
- Updated:
- 7/27/2020 9:18:21 PM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Sphincter of Oddi (Hepatopancreatic Sphincter) CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Sphincter of Oddi (Hepatopancreatic Sphincter)
Introduction
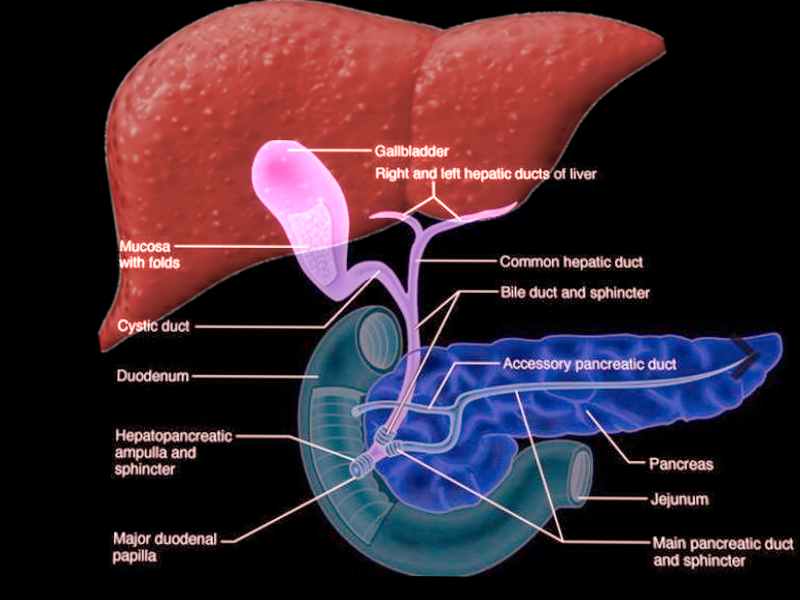
First described by Ruggero Oddi in 1887, the sphincter of Oddi (SO) is a smooth muscle valve located in the second portion of the duodenum. It serves to regulate the flow of hepatic and pancreatic substances into the small intestines. Although its function seems simple, it represents a great example of how smooth muscle can be under the regulation by hormones and other signals. The SO serves many purposes in medicine and is often traversed in procedures such as endoscopic retrograde cholangiopancreatography (ERCP). This sphincter may also become dysfunctional at times requiring either medical or surgical intervention.
Structure and Function
The sphincter of Oddi is a muscular valve responsible for controlling the flow of bile and pancreatic secretions through the ampulla of Vater into the second part of the duodenum. It is composed of three layers of concentric smooth muscle that surrounds the common bile duct, the main pancreatic duct, and the ampulla of Vater. The papilla of Vater includes the SO and its overlying mucosa. So far, the SO has been identified to have at least three functions[1][2]:
- To prevent reflux of duodenal contents thereby preventing the accumulation of sludge and particulate matter in the bile ducts and thus helps to reduce the risk of cholangitis
- Regulate the flow of bile and pancreatic secretions
- Allow retrograde filling of the gallbladder to occur
The sphincter of Oddi serves as a great example of hormonal regulation of smooth muscle. Across the literature, the most important of these hormones is cholecystokinin (CCK). It gets released from enteroendocrine cells in response to the digestion of a meal; this stimulates the contraction of the gall bladder, resulting in the emptying of pancreatic secretions and bile into the common bile duct. CCK has been demonstrated to cause the release of VIP and nitric oxide by intrinsic neurons of the sphincter of Oddi, resulting in a decrease in sphincter tone, ultimately leading to the release of the backed-up contents into the duodenum to aid with digestion. Somatostatin is also another noteworthy hormone shown to increase sphincter of Oddi tone. In contrast, motilin and secretin serve the opposite effect by decreasing sphincter of Oddi tone and allowing the flow of contents from the gallbladder and pancreas.[3][4][5]
Embryology
The sphincter of Oddi is a concentric ring of muscle originating from the mesenchyme surrounding the pre-ampullary portion of the bile and pancreatic ducts. Initially, it begins as a transverse slit in the circular smooth muscle at the junction between the duodenal wall and the bile and pancreatic ducts. The sequence of SO differentiation is as follows[6]:
- Week 10: sphincter of Oddi begins differentiation
- Week 12: the bile and pancreatic ducts emerge through the transverse slit of the concentric smooth muscle of the duodenum
- Week 16: the muscularis propria extends outside the fenestra to the upper end of the ampulla
- Week 28: the muscularis propria is differentiated almost to the distal end of the ampulla
Blood Supply and Lymphatics
In about half of individuals, the retroduodenal artery (i.e., the posterior superior and anterior superior pancreaticoduodenal artery) forms an arterial plexus that provides the primary blood supply to the region of the sphincter of Oddi. The remaining half receive blood supply to the sphincter of Oddi directly from one of the major branches of the retroduodenal artery, with the most likely branch being the posterior superior pancreaticoduodenal artery. The lymphatic drainage of the sphincter of Oddi follows the drainage of the encompassing ampulla of Vater, which drains into the posterior pancreatoduodenal lymph nodes, followed by the lymph nodes around the superior mesenteric artery, and finally into the para-aortic lymph nodes that follow their well-described path of drainage.[7][8]
Nerves
The sphincter of Oddi possesses a complex intrinsic set of neural innervation. Currently, two ganglionated plexus have appeared in the literature:
- Myenteric plexus, which lies between the sphincter's muscular layers
- Submucosal plexus
There have also been a few subpopulations discovered in animal models that helped our understanding of the intrinsic innervation of the sphincter of Oddi. One of these described subpopulations was in guinea pigs and was found to be immunoreactive to choline acetyltransferase and served to provide an excitatory effect, thereby increasing sphincter of Oddi tone. Researchers also found a second, smaller, subset of neurons in the sphincter of Oddi that was immunoreactive to nitric oxide (NO) synthase and expressed vasoactive intestinal peptide (VIP) and neuropeptide Y (NPY).
As opposed to the intrinsic neural innervation of the sphincter of Oddi, its extrinsic innervation is not very well understood but is thought to display characteristics similar to that of most of the biliary tract. This neurology includes parasympathetic nervous system innervation originating from the vagus nerve and sympathetic nervous system innervation originating from the superior mesenteric ganglion following the inferior pancreatic duodenal artery.
The sphincter of Oddi is also thought to be part of bidirectional signaling pathways. There seems to be a bidirectional connection between the sphincter of Oddi and the gallbladder; the electrical activity of the gallbladder has been shown to inhibit sphincter of Oddi contraction reflexively. Similar to the aforementioned bidirectional system, there also exists evidence of a subpopulation of neurons demonstrating bidirectional signaling between the duodenum and sphincter of Oddi ganglia as part of an excitatory cholinergic pathway.[7][9][10][11]
Physiologic Variants
Concerning the sphincter of Oddi musculature, only variations of size of been described. Of clinical significance is the existence of hypertrophic sphincter of Oddi smooth muscle in a small proportion of patients, which increases the risk of stenosis. Hypertrophic smooth muscle may also represent a risk factor for chronic obstructive pancreatitis or a cause for biliary type pain.[12][13]
Surgical Considerations
Surgeons encounter the sphincter of Oddi in many surgical and nonsurgical procedures, and so a proper understanding of potential variations in arterial supply is crucial in avoiding undue harm. In about 5% of the population, the distance between the retroduodenal artery and the papillary orifice is less than 35 millimeters. This proximity creates a small risk of hemorrhage during procedures that require entry through the sphincter of Oddi, such as an ERCP with sphincterotomy, sphincteroplasty, or surgical interventions.[7]
Clinical Significance
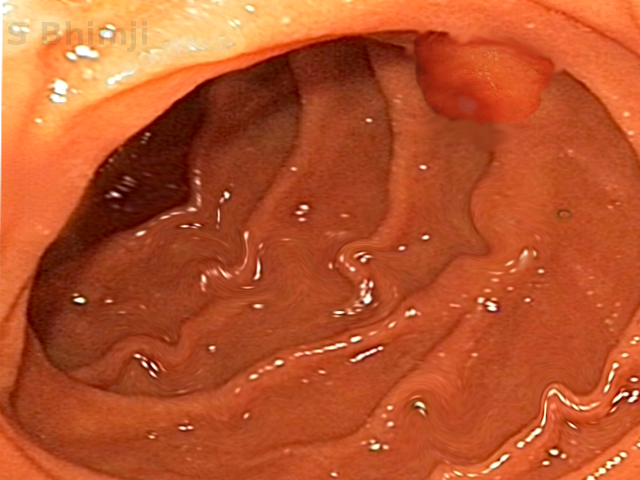
Perhaps one of the most clinically significant topics on the sphincter of Oddi is sphincter of Oddi dysfunction (SOD). SOD is defined broadly as the impairment of the sphincter's ability to perform its normal functions of controlling the flow of contents into the duodenum, as mentioned above. The main clinical feature of SOD is intermittent bouts of epigastric and right upper quadrant pain that is often precipitated by meals. The pain may last between half an hour up to several hours and most commonly presents in middle-aged women. The pain is often associated with:
- Nausea and vomiting, which may be mistaken for a gallbladder attack
- Transient increase in liver function tests (LFT) or pancreatic enzymes
- Delay in the emptying of contrast from the CBD or PD while in the supine position
- Radiating pain in the region of the back, shoulder, or scapula
- Dilation of the CBD or PD
While all the above are typical symptoms/findings associated with SOD, all of these factors are not present in every patient with sphincter of Oddi dysfunction. SOD is often broken down into two main categories: (1) stenosis and (2) dyskinesia.
SO Stenosis
Any processes that involve a narrowing of the sphincter of Oddi, excluding dysfunction inherent to the sphincter muscle itself, is described as sphincter of Oddi stenosis. This condition includes inflammatory or neoplastic processes around and including the sphincter that decreases the caliber of the orifice. Trauma to the sphincter may also lead to stenosis; this includes trauma due to the passage of stones or sludge, as well as intra-operative trauma. Sphincterotomies, performed during ERCP, may also be complicated by stricture formation. As described earlier, patients with congenitally hypertrophic sphincters may also develop SO hypertension, which may lead to stenosis. The result of sphincter of Oddi stenosis is abnormal motility and increased basal pressures.
SO Dyskinesia
While sphincter of Oddi stenosis represents a physical impairment due to damage, inflammation, or neoplastic processes, sphincter of Oddi dyskinesia represents a less understood motility disorder. SO dyskinesia leads to a transient obstruction of the sphincter, manifesting with the symptoms mentioned above of SOD. So far, in the literature, two theories have gained prominence to describe SO dyskinesia:
- A paradoxical response to endogenous hormones due to dysfunctional neurologic pathways may cause sphincter of Oddi dyskinesia
- Sphincter of Oddi dyskinesia may lie at the hormonal and neurotransmitter level leading to sphincter of Oddi hypertension
SOD Diagnosis
The standard test to diagnose SOD has been Sphincter of Oddi Manometry (SOM). It involves the use of ERCP techniques and knowledge of manometry to directly examine the motor activity of the sphincter of Oddi. This test may be useful in patients that have multiple symptoms described above and have been shown to help guide therapeutic decisions. Alternatively, the use of clinical criteria, such as the Milwaukee Classification and Rome IV Criteria, can provide patients and providers a non-invasive way to stratify patients with suspected SOD to allow for appropriate management.[2][14][15][16]