Anatomy, Abdomen and Pelvis, Sphincter Urethrae
- Article Author:
- Peter Sam
- Article Author:
- Jay Jiang
- Article Editor:
- Chad LaGrange
- Updated:
- 10/28/2020 1:05:36 AM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Sphincter Urethrae CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Sphincter Urethrae
Introduction
The urethral sphincter is a muscular structure that regulates the outflow of urine from the bladder into the urethra. There are 2 urethral sphincters, the external and internal urethral sphincters. When these muscles contract, the urethra narrows, and urination stops or slows. The urethral sphincter is critical for the maintenance of urinary continence. Urinary incontinence is usually associated with the pathology of the urethral sphincter and is a very common problem worldwide. Also, normal urethral sphincter function is necessary for ejaculation of semen in males. The urethral sphincter muscles are located within the deep perineal pouch.[1][2][3][4][5]
Structure and Function
The internal urethral sphincter regulates involuntary control of urine flow from the bladder to the urethra, and the external urethral sphincter provides voluntary control of urine flow from the bladder to the urethra. The internal urethral sphincter in men also functions to prevent retrograde flow of semen into the bladder during ejaculation.
Embryology
In the ninth week of the fetal period, there is undifferentiated mesenchyme that is located in the anterior part of the urethra, which develops into the external urethral sphincter. The external urethral sphincter is also known as rhabdosphincter. Later, around the 12th week, striated muscle fibers start to develop. The internal urethral sphincter is thought to arise from the absorption of the Wolffian duct into the bladder and urethra.
Blood Supply and Lymphatics
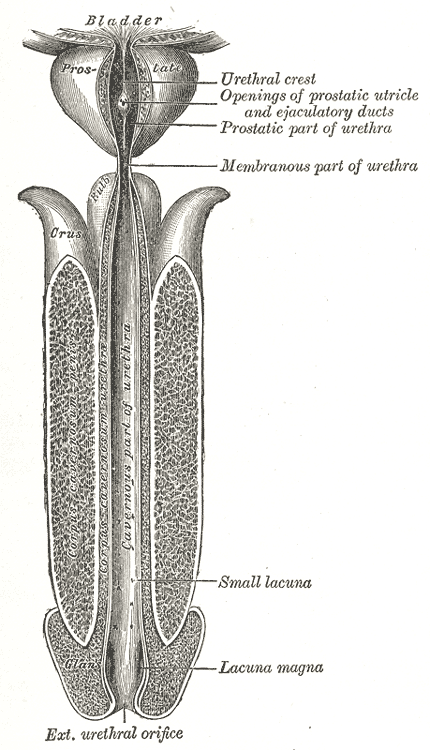
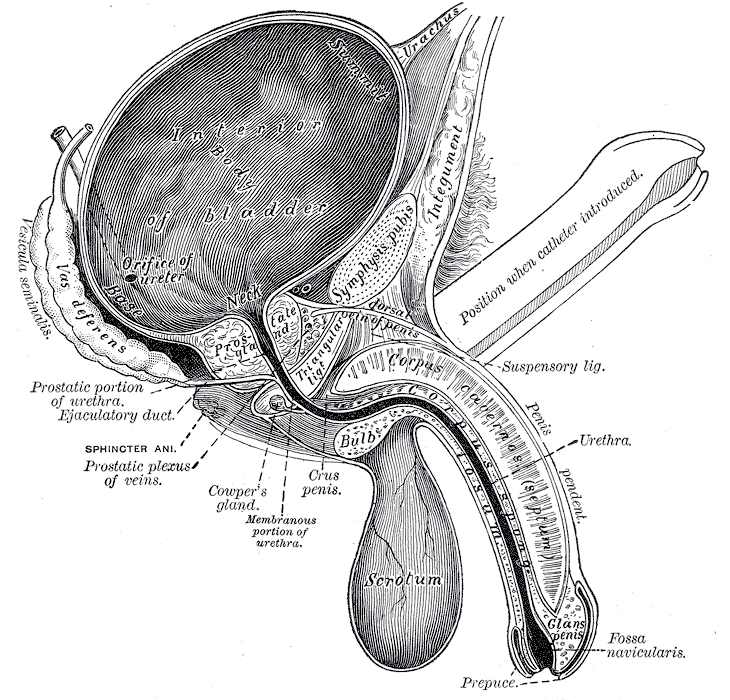
The internal urethral sphincter is located inferiorly, in the neck of the bladder. In males, the inferior vesical artery supplies blood to the neck and fundus of the bladder. However, in females, the vaginal artery replaces the inferior vesical artery to supply the neck and fundus of the bladder. In females, the blood supply to the external urethral sphincter is the internal pudendal artery from the internal iliac artery. In males, the external urethral sphincter is in the same area as the membranous urethra which is supplied by the bulbourethral artery. The vessels of the internal pudendal which supply the area of the external urethral sphincter and the internal urethral sphincter drain into the internal iliac lymph nodes.
Nerves
The pudendal nerve innervates the external urethral sphincter from the S2 to S4 nerve roots. When stimulated, it leads to constriction of the urethra. The external urethral sphincter is made of skeletal muscle and is under voluntary control via the pudendal nerve and nicotinic receptors. The internal urethral sphincter is composed of smooth muscle. Thus it is controlled by the autonomic nervous system via the hypogastric nerves and alpha one receptors. When the bladder is full, the parasympathetic response increases and sympathetic activity decreases, which leads to relaxation of the internal sphincter muscle.[6][7]
Muscles
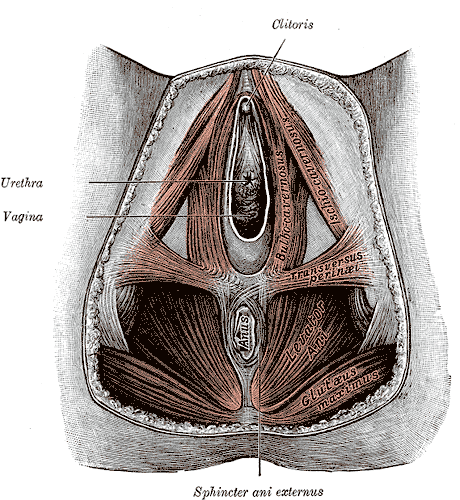
The internal urethral sphincter consists of smooth muscle and is continuous with the detrusor muscle of the bladder. The muscle fibers form a circular configuration that is continuous with the smooth muscle fibers of the bladder. Contraction of internal urethral sphincter stops the flow through the internal urethral orifice preventing the flow of urine from the bladder. The internal urethral sphincter is made of a layer of smooth muscle that is surrounded by striated muscle. The external urethral sphincter is composed of striated muscle and is located distally and inferiorly to the bladder neck in women between the vaginal orifice and clitoris. In the females, the external sphincter is also known as the urogenital sphincter and is made of 3 parts. The first part is circular. The second part is known as the urethral compressor muscle and passes anteriorly pass the urethra and connects to the ischial rami. The third part surrounds both the vagina and urethra and is known as the urethrovaginal sphincter. Contraction of urethrovaginal sphincter leads to constriction of both the urethra and vagina. In males, the external urethral sphincter is located at the same level as the membranous urethra and is composed of circular muscle fibers. The external urethral sphincter is continuous with the isthmus of the prostate. The external sphincter is located between the area of the pudendal canals below the pelvic diaphragm.
Surgical Considerations
Urinary incontinence can occur after pelvic surgeries. This is a common complication, especially in prostate cancer treatment. Urethral sphincter incompetence is one of the most important contributing factors for post-radical prostatectomy urinary incontinence. Although, bladder dysfunction could also play a role in the incontinence. Rates of postoperative urinary incontinence vary widely by surgeon experience, but good results are between 4% to 8% of patients.[8][9][10]
Clinical Significance
When there is a malfunction of the urethral sphincters, it can lead to disorders of the lower urinary tract. Urinary incontinence can occur in both men and women at all ages but is significantly more common in females. The urethral sphincter may be damaged during childbirth due to stretching of the ligaments and dysfunction of the pelvic floor muscles. The pudendal nerve may be injured during vaginal birth as it travels between the sacrotuberous and sacrospinous ligaments. Stress incontinence accounts for nearly 90% of patients with incontinence. This occurs because there is a problem with the closing mechanism at the urinary tract outlet. Stress incontinence is characterized by loss of urine during sneezing, coughing, or intense physical activity. Urge incontinence is associated with the sudden need to urinate that leads to loss of urine that is more commonly associated with detrusor overactivity. Overflow incontinence is frequent dribbling of urine because the bladder can not empty completely that is usually due to detrusor underactivity or bladder outlet obstruction. Functional incontinence is the inability to get to the restroom due to mental or physical issues. Mixed incontinence is a mixture any of the types of incontinence. A bladder stress test can be used in patients suspected of having stress incontinence. To do the test in women, an examiner will visualize the urethra by separating the labia and have a patient cough or Valsalva. If there is leakage of urine from the urethra, then she is confirmed to have stress incontinence. The treatment for urinary incontinence varies depending on the cause. However, initial treatment for most types of urinary incontinence includes lifestyle modifications and pelvic floor muscle exercises. Lifestyle modifications include: weight loss, dietary changes, minimize constipation, and smoking cessation. Pelvic floor or Kegel exercises are very effective in treating stress incontinence. If these initial conservative measures fail to work, the patient may opt for support devices, pharmacotherapy, or surgery.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)