
Strabismus
- Article Author:
- Venkata Kanukollu
- Article Editor:
- Gitanjli Sood
- Updated:
- 8/10/2020 9:34:51 PM
- For CME on this topic:
- Strabismus CME
- PubMed Link:
- Strabismus
Introduction
Strabismus is derived from a Greek word, which means “eyes looking obliquely.” Strabismus means misaligned eyes. Often strabismic eyes are referred to as “squinting eyes,” “crossed eyes,” and “wall eyes.” Usually, both eyes fixate equally while focusing on an object with the head held in the primary position. In strabismus or squint, one or both eyes deviate inwards or outwards and appear to be in non-alignment towards the direction of the focused object. It can be due to refractive error or binocular fusion abnormalities or neuromuscular anomalies of ocular movements. If diagnosed and treated early, strabismus has a very good prognosis. Treatment is usually by refractive error correction, orthoptic exercises, occlusive patching, topical medications, and extraocular muscle surgery.
Etiology
Strabismus or squint is broadly classified as
- Pseudostrabismus or apparent squint: Pseudoesotropia and pseudoexotropia
- Latent squint (Heterophoria)
- Manifest squint (Heterotopia): Concomitant squint and incomitant squint
Causes for Pseudostrabismus
- Pseudoesotropia: Prominent epicanthal fold and negative angle kappa
- Pseudoexotropia: Hypertelorism and positive angle kappa
Causes for Heterophoria
- Anatomical causes: Orbital asymmetry, abnormal interpupillary distance (IPD), mild weakness of extraocular muscles, etc.
- Physiological causes: Esophoria is seen in increased accommodation (hyperopes) and exophoria in decreased accommodation (myopes), excessive or decreased use of convergence, and in dissociated works like working with a uniocular microscope or magnifying glasses.
- Decompensation causes psychiatric disorders, illness, the inadequacy of the fusional reserve, older age, and precision jobs.
Causes of Concomitant Squint:
- Sensory causes: These interfere with a clear image formation in one eye. Refractive errors, anisometropia, media opacities, obstruction of pupillary area, macular and optic nerve diseases, and wrong glass prescription for refractive error.
- The motor causes: These interfere with ocular alignment. Orbital, extraocular muscle, and accommodation abnormalities.
Causes of Incomitant Squint:
- Neurogenic causes: Hypoplasia of 3rd, 4th, and 6th cranial nerve nuclei, tumors, infections, trauma, toxicity (alcohol, lead, carbon monoxide), vascular (ophthalmoplegic migraine), and demyelinating lesions affecting the third and sixth cranial nerves.
- Myogenic causes: Congenital lesions, trauma, muscle incarceration in orbital fractures, post-viral myositis, and chronic progressive external ophthalmoplegia (CPEO).
- Neuromuscular junction disorders: Myasthenia gravis.
Risk factors
Strabismus is more prevalent with certain syndromes like Down syndrome, cerebral palsy, Apert-Crouzon syndrome, premature infants with low birth weight, and in kids with affected parents or siblings. All siblings of a strabismic child should be screened at an early age for strabismus as sensorimotor anomalies are common in the pedigrees of strabismic probands.
Epidemiology
The prevalence of strabismus is 2 to 5 percent in the general population.[1][2]. Five to fifteen million population of the United States of America is affected by strabismus. In a National Health Survey, exotropia is seen in 2.1 percent and esotropia in 1.2 percent of the population between 4 to 74 years of age. This difference is due to the higher prevalence of exotropia in the population between 55 to 75 years of age.[2] In a population-based study done in Los Angeles, California, involving children aged between 6 to 72 months, Hispanic/Latino kids showed 2.4 percent, and African Americans showed 2.5 percent of strabismus. Exodeviations were more common than esodeviations.[3]
Fifty percent of all childhood esotropias are either fully or partially accommodative. Non-accommodative esotropia is seen in 10 percent of all strabismus and is the second most common form of childhood esotropia.[4] Infantile esotropia affects one in every 100 to 500 persons, which accounts for 8.1 percent of cases of esotropia.[5] Intermittent esotropia is seen in one percent of the population and is the most common form of exotropia.[6][7] Exotropia is more prevalent in Asian and African American populations than in Whites.[8] Women are affected in 60 to 70 percent of patients with exotropia.[9]
Pathophysiology
Etiopathogenesis of strabismus is unclear. The physiology of ocular motility involves extraocular muscles, cranial nerves, supranuclear pathways, and their cerebral controls. All of these have been implicated in the development of strabismus. Following two theories are popular:
- Claude Worth theory states that an inherent absence of cortical fusional potential is the cause of strabismus.
- Chavasse theory states that motor alignment leads to a poor sensory status, which, if left untreated, leads to strabismus. This theory justifies early treatment for squint, which leads to sustained improvement in binocular single vision (BSV). Hence many surgeons justify doing early surgery in conditions like infantile esotropia.
In relation to muscle innervation and action, the following two laws of ocular motility govern the extraocular motility:
- Sherrington law of reciprocal innervation: Increased innervation to a muscle is accompanied by decreased innervation to its antagonist. Exception: Duane retraction syndrome.
- Herring law of equal innervation: Equal and simultaneous innervation flows through synergistic muscles during any conjugate eye movement. Exception: Dissociated vertical deviation.
History and Physical
Although strabismus can occur at any age, its commonly seen before six years with a peak onset around three years. Parents often claim that their child has crossed eyes since birth. Family photographs often help to document the age of onset. Moreover, pictures might show ocular preference in fixation. Alternating fixation denotes an absence of amblyopia in squinting infants. Strong fixation of one eye implies strabismic amblyopia in the other eye. A history of low birth weight indicates retinopathy of prematurity, which might lead to pseudostrabismus from ectopic macula. Acute onset of esotropia in an older child always requires a thorough evaluation to rule out neurological abnormalities. Intermittent strabismus indicates a better recovery of normal binocular vision as it implies that fusion is a present part of the time. Photosensitivity is commonly seen in intermittent exotropia and is caused by a decreased binocular photophobia threshold.[10] History of allergy to dilating drops, familial hepatic porphyria, sensitivity to suxamethonium, and malignant hyperthermia is essential to prevent fatal anesthetic complications during surgical management of strabismus.
Clinical features of the commonly occurring strabismus conditions are as follows:
- Essential infantile esotropia (Congenital esotropia): Large angle stable esotropia, which presents within six months of age with positive family history and no neurological deficit. Refractive error is uncommon with poor potential for BSV. Cross fixation, asymmetrical optokinetic response, and latent horizontal nystagmus are seen. Dissociated vertical deviation (DVD) develops in 80% of children by three years of age. Treatment is aimed at correcting hyperopia and treating amblyopia. Muscle surgery should be performed early between 6 months to 2 years of age.
- Accommodative esotropia: Onset between 2-5 years of age with less than 10 prism diopters (PD) deviation and precipitated by trauma or illness. Family history and amblyopia are common. Mechanisms involved in accommodative esotropia are uncorrected hypermetropia, accommodative convergence, and poor fusional divergence. Normal accommodation convergence/accommodation ratio (AC/A ratio) with hyperopia of more than 2 Diopters (D) is seen in refractive type, while non-refractive type shows a high AC/A ratio with no clinically significant hyperopia. Treatment includes full cycloplegic correction and short term miotics if children are intolerant to spectacles. If AC/A ratio is high, Bifocals are prescribed with minimum plus add given for near vision. Surgery is indicated if the residual esotropia is greater than 10 PD.
- Microtropia: Microtropia or Monofixation syndrome is a unilateral abnormality of BSV with amblyopia, and ultra-small angle deviation of fewer than 5 degrees or 8 PD. Anisometropia is seen nearly in all patients with reduced stereopsis, abnormal retinal correspondence (ARC), normal motor fusion, and foveal suppression scotoma. ‘4 -prism diopter’ placed base out in front of the non-fixating eye, will not show any re-fixation movement in microtropia as the image will be shifted within the central suppression scotoma. Treatment is by correcting anisometropia and amblyopia.
- Intermittent exotropia: This presents around two years with exophoria, which breaks down to exotropia under conditions of visual inattention, bright light, and fatigue, or ill-health. Other features are headache, asthenopia, diplopia, photo-diplopia, micropsia, abnormal stereopsis, and temporal retinal hemisuppression. Treatment should begin with correcting refractive error and treating amblyopia. Orthoptic exercises with pencil pushups help to some extent. A bilateral lateral rectus recession is commonly performed strabismus surgery to correct the divergence excess.
- Dissociated vertical deviation (DVD): This bilateral, asymmetric, and asymptomatic strabismus manifests around two years and is commonly associated with congenital esotropia (75%). It presents as an updrift with excyclotropia of the eye undercover or during visual inattention. When the cover is removed, the affected eye will move down without the corresponding downdrift of the other eye. This downdrift of the occluded eye is also seen when the fixating eye is occluded with increasing neutral density filters. This is called the ‘Bielschowsky phenomenon’ and is specific for DVD. Inferior oblique overaction (IOOA) is the most common differential diagnosis of DVD, which shows the absent Bielschowsky phenomenon. Superior rectus recession with Retroequatorial myopexy (Faden procedure) is the surgery of choice.
- Monocular elevation deficiency: Also called ‘Double elevator palsy’, presents as a unilateral total inability to elevate with hypotropia in primary gaze, ptosis, and chin-up position. Knapp procedure (full tendon width vertical transposition of horizontal recti) for superior rectus weakness and inferior rectus recession for inferior rectus restriction is the procedure of choice.
- Alphabet patterns: Alphabet pattern is strabismus where the horizontal deviation changes from upgaze and downgaze. V pattern is common than A pattern.
- Duane retraction syndrome: This congenital syndrome presents as a globe retraction on adduction with narrowing of the palpebral fissure. In severe cases, globe up-shoot or down-shoot is seen with adduction. Its commonly seen in females with a preponderance to the left eye and is seen bilaterally in 20% of cases. It arises due to a congenital innervation of lateral rectus by the third cranial nerve due to agenesis of the sixth cranial nerve (pontine agenesis). Globe retraction is due to the co-contraction of both medial and lateral rectus. Surgery is indicated in significant heterotopia in primary gaze, abnormal head position, cosmetically unacceptable globe retraction, and for up-shoot/down-shoot movements.
- Browne syndrome: This restrictive disorder of superior oblique tendon can be congenital or acquired and presents as a limitation of elevation in adduction. Presents bilaterally in 10 % of cases, commonly seen in females affecting more in the right eye. Acquired causes are due to trauma or inflammation (Rheumatoid arthritis, sinusitis, scleritis, etc.) to the superior oblique tendon. Forced duction test is positive on retropulsion.
- Mobius syndrome: This presents as an inability to abduct either eye past midline with vertical gaze being normal and is due to congenital bilateral aplasia of the sixth and seventh cranial nerve.
- Oculomotor palsy: Third cranial nerve palsy presents as ptosis with abducted and intorted eye with defective accommodation.
- Lateral rectus palsy: Presents as an esotropic eye with limitation of abduction.
- Superior oblique palsy: Presents as ipsilateral limitation of depression on adduction, excyclotorsion, vertical and torsional diplopia on looking down. Parks 3 step test helps in diagnosing the paretic muscle in vertical diplopia, especially in superior oblique palsy. A right superior oblique palsy presents as hypertropia on the primary gaze with increasing hypertropia on the left gaze and on right-sided head tilt. The Head is tilted and turned towards the opposite side with depression of chin. Bilateral cases show right hypertropia in right gaze and left hypertropia on left gaze with greater than 10 degrees of cyclodeviation on double Maddox rod test and chin depression without head tilt. It is seen both as a congenital or acquired disorder. Acquired causes are trauma, vascular lesions, aneurysm, and tumors. Surgery involves superior oblique strengthening by Tucking/Tenoplication or Harada Ito procedure (Splitting and anterolateral transposition of the lateral half of the superior oblique tendon).
Evaluation
The evaluation of strabismus starts with good history taking, ocular/physical examination, and with appropriate investigations. The history-taking aspect is already dealt with above. The physical and ocular assessment are as follows:
Visual Acuity:
- Infants: ‘CSM’ method is a simple technique to observe fixation and the followability. With a simple torch, observe the corneal reflex while moving it side to side. Central corneal light reflex shows “central” fixation, and the followability of eye sidewards to the torch is termed as “steady,” and if both eyes are in alignment during the movement, then its termed as “maintained”.
- Preverbal children: Preferential looking tests e.g., Cardiff picture cards
- Uncooperative children: children might cry or object to occluding the eye with good vision.
- Children: Snellen charts, Illiterate E chart, Sheridan-Gardiner charts
Stereo acuity: Stereoacuity measures the visual sense of depth. It is the sense of fusion of two simultaneous, slightly dissimilar images with integration by the brain. Titmus stereo-fly test and Lang cards are commonly used. Worth 4 dot test and Bagolini striated glasses are used to assess the fusional reserve while both stereopsis and fusion can be assessed by synoptophore.
Compensator Head Posture (CHP): CHP is a motor adaptation to strabismus to attain binocular single vision (BSV). Loss of CHP in concomitant strabismus may indicate the loss of BSV and warrants surgical intervention. In acquired paretic strabismus, CHP eliminates diplopia and helps to centralize the binocular visual field. Head tilt, face turn and chin up/down are commonly seen as abnormal head postures. A head tilt to the left is seen in right superior oblique palsy. A face turn to the left is seen in the left lateral rectus palsy. Chin up or down is seen in “A” or “V” pattern strabismus.
AC/A ratio: The accommodative convergence/accommodation (AC/A) ratio is defined as the amount of convergence in prism diopters per diopter change in accommodation. Two methods are used to measure the AC/A ratio: the lens gradient method and the heterophoria method. The normative range lies between 3 and 5 to 1.
Measurement of Deviation
- Hirschberg test: The Hirshberg test gives a rough estimate of the angle of manifest strabismus by noting the position of the corneal light reflex produced by shining a torchlight over the cornea. Each millimeter of deviation is equal to 7 degrees of deviation or 14 PD, assuming pupil to be 4 mm in diameter. If the light reflex is at the temporal border of the pupil, then the angle of deviation of esotropia is about 15 degrees, and if it is at the limbus, the angle is about 45 degrees.
- Krimsky test: This test uses prisms placed in front of the fixating eye to measure the deviation. The modified Krimsky test is done by holding the prism in front of the deviating eye. This test is essentially used to measure tropias and not for phorias.
- Cover test: The cover test is done to detect heterotropia. The fixating eye is covered, and movement of the uncovered eye is noted both for distance and near.
- Uncover test: Uncover test detects heterophoria. After covering an eye for 2 to 3 seconds, the same eye movement is observed on uncovering. This test is done for both distance and near. Most examiners do the cover test and uncover test sequentially; hence it is called the “cover-uncover” test.
- Alternate cover test: This is a dissociation test that reveals the total deviation when fusion is interrupted and should be performed only after the cover-uncover test. Patients with poor fusional control may decompensate to a manifest deviation when this test is done. The speed and smoothness of recovery are noted following a fast cover-uncover test done alternatively to both eyes.
- Prism cover test: This test combines the alternative cover test with prism for both near and distant fixation.
- Maddox wing: This test dissociates the eyes for near fixation (33cm) and measures heterophoria. When seeing through this instrument, the right eye sees only the arrows (white vertical and red horizontal), while the left eye sees only rows of numbers (horizontal and vertical). The white arrow position denotes horizontal deviation, and a red arrow denotes the vertical deviation. By aligning the red arrow parallel to the horizontal row of a number, cyclophoria can be measured.
- Maddox rod: Maddox rod converts a white light spot into a perpendicular red streak by a series of fused cylindrical red glass rods. The amount of dissociation is calculated by the superimposition of the two images using the prisms.
Ocular Motility: Extraocular movements involves the assessment of smooth pursuit movements followed by saccades.
- Versions: All nine diagnostic positions of gaze binocularly are assessed with a torch or a pen, and the cover-uncover test is done in each cardinal position to assess tropia/phoria.
- Ductions: Ductions are monocular eye movements elicited in all six cardinal positions by occluding the other eye. Ductions are assessed if either or both eyes ocular motility limitations are noticed. Underaction is graded from -1 to -4 with increasing degrees of underaction, and 0 indicates full movement.
- Vergence: convergence and divergence movements
- Near point of Convergence: Near point of convergence (NPC) is the nearest point at which the patient reports diplopia when tested with an RAF rule. It should be nearer than 10 cm.
- Near point of accommodation: Near point of accommodation (NPA) is the nearest point at which the eyes can maintain clear focus when tested with RAF rule. At 20 years of age, it is 8 cm and recedes to 46 cm by 50 years.
- Fusional amplitudes: Fusional amplitudes measure the efficacy of vergence movements and are tested with prism bars or synoptophore.
- Postoperative diplopia test: This test is mandatory for all patients above seven years of age before strabismus surgery. Prisms larger than the planned correction for the deviation is placed in front of the deviating eye. If suppression is seen, then the risk of diplopia following surgery is less. Intermittent or constant diplopia is an indication to do diagnostic botulinum toxin tests before the surgery.
Field of BSV: Field of binocular single vision is that area where bifoveal fusion of the object of regard occurs. The field of BSV is assessed by Hess chart to diagnose and monitor patients with incomitant strabismus caused by either extraocular muscle palsy (third, fourth, or sixth cranial nerve palsies) or restriction (thyroid ophthalmopathy, blow-out fracture or myasthenia gravis). Hess chart uses either Hess screen or Lees screen to chart the field by dissociating the ocular movements. Hess screen uses a tangent screen with a red-green goggle, and Lees screen uses two glass screens at right angles to each other.
The following is the interpretation of the Hess chart appearance:
- Smaller chart: indicates the eye with the paretic muscle, and the greatest restriction is in the direction of the paretic muscle.
- Larger chart: indicates the eye with an overacting muscle, and the greatest expansion is in the main direction of action of the yoke muscle.
The following sequelae are seen in the muscles in a paretic squint:
- Overaction of the ipsilateral antagonist (contracture)
- Secondary inhibition palsy of the antagonist of yoke muscle
Refraction: Assessing the correct refractive error and power is crucial in the management of strabismus. Most commonly, hypermetropia is seen in strabismus patients. Refraction should be done under both non-cycloplegic and cycloplegic conditions. Instilling one drop of 1% cyclopentolate hydrochloride twice at 5-minute intervals followed by retinoscopy thirty minutes later is the standard practice.
Forced duction test (FDT): This test is done to assess if the limitation of movement is due to the mechanical restriction of the muscle (fibrosis/tethering). The anesthetized conjunctiva of the eyeball is held with forceps and moved first in the direction of the muscle action and later in all directions to see if there is a restriction of the movement of the eyeball. This test should be mandatorily performed before any strabismus surgery.
Parks-Bielschowsky 3-step test: This test is done in acquired vertical diplopia to isolate the paretic muscle. Step1: Which eye is hypertropic in the primary gaze? Step 2: Is the hypertropia worsening of right or a left gaze? Step 3: Is the hypertropia worsening with the right head tilt or left head tilt? This test helps in diagnosing superior oblique palsy.
Fundoscopy: Dilated fundus examination is mandatory to rule out intraocular pathologies like optic disc hypoplasia, macular scarring, or retinoblastoma, which might cause squint.
Investigations for strabismus: Neuroimaging is essential, especially in sudden onset adult-onset strabismus to rule out stroke, diabetic mononeuritis, myasthenia gravis, thyroid eye disease, etc. Rarely a primary neurological disorder such as hydrocephalus, optic nerve glioma, medulloblastoma, or craniopharyngioma might cause childhood strabismus and need neuroimaging.
Treatment / Management
The primary aim of treating strabismus is to restore proper ocular alignment. The secondary aims are to treat amblyopia, maintain binocularity, and eliminate diplopia.
Following are the various methods of treating strabismus:
Observation: Strabismus secondary to myasthenia gravis, diabetic mononeuropathy, and post-traumatic restrictive strabismus mostly improve with time and with the treatment of the primary cause. Some healthy neonates show intermittent deviation of the eyes. These are called ‘neonatal ocular misalignments,’ which improve by two months and resolve in four months. They usually reflect a normally developing vergence system.[11]
Correction of Refractive Errors: The first step in the management of any child with strabismus is to evaluate for a refractive error and correct it fully. The full correction of hypermetropia is the treatment of choice for all forms of esotropia. Full correction without subtracting any lens power for cycloplegia is prescribed. In convergence excess esotropia, executive bifocals are prescribed to relieve accommodation and thereby preventive accommodative convergence. A minimal plus “add” required is prescribed with the flat top of the bifocal segment bisecting the upper border of the pupil.[12] In intermittent exotropia, full myopic correction often controls the exotropia.[13]
Treat Amblyopia: Amblyopia in strabismus is reduced visual acuity in one or both eyes because of misalignment of eyes in the absence of any demonstrable visual pathway abnormality. Refractive correction alone is successful in improving amblyopia in nearly one-third of the patients.[14] Patching of the better eye to force the brain to use the weaker eye is the gold standard treatment for amblyopia. Patching the better eye for 2 to 6 hours in a day is recommended and is most effective with children less than seven years of age. Atropine penalization (atropine 1% eyedrops twice daily in the better eye) is also as effective as occlusion.[15][16] As the effect of atropine actions lasts for 2-3 weeks, frequent follow-ups are necessary to detect occlusion/reversal amblyopia of the better eye.
Orthoptics: Orthoptic exercises are commonly used to treat intermittent exotropia. Fusional exercises like “pencil push-ups” are done with a pencil held at arm’s length and slowly moved towards the nose, thereby inducing accommodation and strengthening convergence, which helps in treating the exotropia.
Prismatic Correction: Ophthalmic prisms move the image closer to the fovea and help in improving the sensory fusion. They are prescribed for deviations of less than 20 PD. Amblyopia, suppression, and anomalous retinal correspondence are contraindications for prism therapy.[17]
Pharmacological Therapy: Miotics act by inducing peripheral accommodation so that the patient uses less of accommodation and thus reducing esotropia. Ecothiopate iodide 0.125 percent once daily is used as a short-term treatment for accommodative esotropia patients. This can be used for kids who are too young or intolerant of glasses.[18]
Botulinum Toxin: Botulinum toxin type A is used as a form of chemodenervation to cause temporary paralysis of the extraocular muscle leading to improvement in the strabismus. It is used as an adjunct to surgical therapy and to assess postoperative diplopia if anticipated following strabismus surgery. This can induce transient ptosis and vertical strabismus.[19]
Extraocular Muscle Surgery: Strabismus surgery should be considered only after conservative treatments have failed to correct the deviation. Esotropias more than 15 PD and exotropia more than 20 PD following full spectacle correction are candidates for surgery. Accommodative esotropias are not ideal candidates for surgery as it induces consecutive esotropia.[20][21] The ideal age for infantile strabismus surgery is before two years of age. A postsurgical deviation of less than 10 prism diopters yields better binocular vision, whereas to achieve stereopsis, the residual deviation should be 4 PD or less.[22] 60 percent reduction of the overall deviation or a deviation of 10 prism diopters or less after six weeks of surgery is considered to be a successful outcome of horizontal strabismus surgery.[23]
The three main types of strabismus surgery are:
- Weakening Procedures: These decrease the effective strength of muscle action. Recession, retro equatorial myopexy or posterior fixation (Faden procedure), marginal myectomy, and myectomy (disinsertion) are some of the weakening procedures.
- Strengthening Procedures: These procedures enhance the pull of the muscle. Resection, advancement, Double-breasting or tenoplication, and cinching are the strengthening procedures.
- Vector Adjustment Procedures. These are transpositioning procedures that alter the direction of muscle action. Hummelscheim, Jensen, O’Connor, Knapp, Callahan, Peter, and Helveston are some of the transpositioning procedures.
Differential Diagnosis
Differential diagnoses can be classified on the basis of the type of defect. Following are some important differentials to be considered:
Congenital esotropia
- Early-onset accommodative esotropia
- Abducens palsy
- Nystagmus blockage syndrome
- Duane retraction syndrome
- Sensory esotropia
- Strabismus fixus
- Moebius syndrome
Fully Accommodative esotropia
- Non-accommodative esotropia
- Congenital esotropia
- Cyclic esotropia
- Convergence excess and near esotropia
Intermittent exotropia
- Infantile exotropia
- Convergence weakness or insufficiency
- Sensory exotropia with poor unilateral vision
Prognosis
Prognosis of strabismus is excellent if detected and managed early in life. Healthy neonates sometimes show intermittent deviation of the eyes, which should not be a concern. At about three months, normal binocular coordination sets in, and any strabismus persistent after this period should be considered abnormal and significant. Amblyopia sets in if the strabismus is not appropriately managed before 6-8 years leading to a permanent decrease in the vision. It is extremely important to know the indications for ophthalmologist referral.
Indications for ophthalmologist referral
- Altered pupillary reflex or leukocoria
- Constant esotropia
- Incomitant strabismus
- Persistent esotropia at four months of age
Complications
Complications of strabismus include the following:
- Amblyopia
- Reduced stereopsis
- Asthenopia
- Diplopia
- Nystagmus
- Abnormal head and neck posture
- Impaired social and mental growth
Surgical treatment for strabismus may result in the following:
- Diplopia
- Under/over-correction
- Conjunctival scarring, granuloma, and chronic inflammation
- Corneal Dellen
- Scleral perforation
- Lost muscle
- Endophthalmitis
- Anterior segment ischemia
- Retrobulbar hemorrhage
Deterrence and Patient Education
Parents should be made aware of the prognosis, advantages, and complications of the management of strabismus and its impact on the social, physical, and psychological growth of the child. A treatment plan based on the discussion with the parents should be charted out. In acute onset strabismus, patients and their care providers should be informed about a possible systemic or neurological cause and a possible referral to an appropriate specialist if needed. The parents need to know the risks of developing amblyopia and impaired stereopsis if adherence to treatment is not maintained.
Enhancing Healthcare Team Outcomes
The treatment of strabismus in children involves a multidisciplinary approach and might take place in a variety of locations. The groups involved are the patient and family members, hospital administration, medical staff, orthoptists and optometrists, community pediatricians, general practitioners, and health visitors. In addition to these varied groups, teachers, school nurses, and community optometrists also play an important role in their management. Good communication is very important between staff and parents. A detailed clearly written medical and orthoptic record should be made available with both patients and the doctors during clinic appointments and on surgical admissions. Community pediatricians should always be kept in the loop during all correspondences between the patients and the ophthalmologists.
(Click Image to Enlarge)
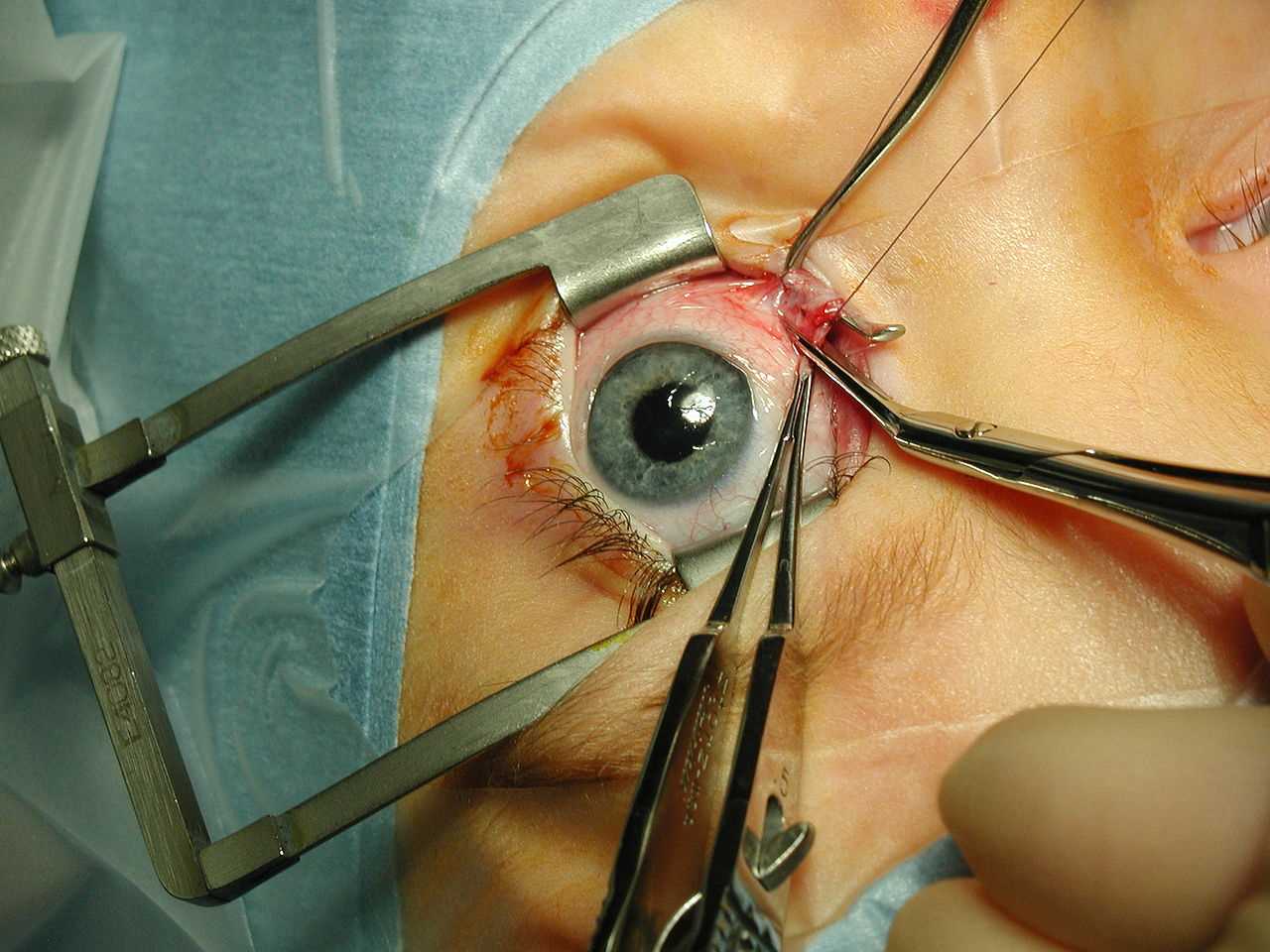
Strabismus surgery—medial rectus muscle being disinserted following pre-placement of polyglactin 910 sutures. A Castroviejo locking forceps is grasping the superior pole of the muscle, while a Manson-Aebli scissors does the cutting. The eyelids are being held by a Cook speculum.
Contributed by Wikimedia Commons (Public Domain)
