Cerebrovascular Disease
- Article Author:
- Aunali Khaku
- Article Editor:
- Prasanna Tadi
- Updated:
- 8/10/2020 4:42:52 PM
- For CME on this topic:
- Cerebrovascular Disease CME
- PubMed Link:
- Cerebrovascular Disease
Introduction
A stroke or cerebrovascular accident (CVA) is an acute compromise of the cerebral perfusion or vasculature. Approximately 85% of strokes are ischemic and rest are hemorrhagic.[1] In this discussion, we mainly confine to ischemic strokes. Over the past several decades, the incidence of stroke and mortality is decreasing.[2] Stroke is the leading cause of adult disability worldwide. It is thus critical to recognize stroke early and treat it rapidly to prevent or minimize morbidity and mortality. There are many causes of stroke. Hypertension is the leading cause of ischemic stroke. In the younger population, there are numerous causes of stroke including clotting disorders, carotid dissection, and illicit drug abuse. In the acute setting, a quick history and examination to be performed. As "time is brain", it is very important not to waste any time. As acute stroke management is evolving rapidly, one must consider patients for intravenous tissue plasminogen activator (IV tPA) up to 4.5 hours and mechanical thrombectomy for up to 6 hours. The recent DAWN trial showed that one can extend the window for mechanical thrombectomy up to 24 hours in selected cases of large vessel occlusion.[3]
Etiology
Ischemic etiologies can further be divided into embolic, thrombotic, and lacunar. In general, the common risk factors for stroke include hypertension, diabetes, smoking, obesity, atrial fibrillation, and drug use. Of all the risk factors, hypertension is the most common modifiable risk factor for stroke. Hypertension is most prevalent in African-Americans and also occurs earlier in life.[1] According to JNC8, the recommended blood pressure targets in patients with stroke should be less than 140/90 mm Hg.[4] Chronic uncontrolled hypertension causes small vessel strokes mainly in the internal capsule, thalamus, pons, and cerebellum.[5] Lifestyle measures such as weight loss, salt restriction, taking more fruits and vegetables (such as the Mediterranean diet)[6] are helpful in decreasing the blood pressure. Every 10 mm Hg reduction in blood pressure is associated with a 1/3rd reduction in stroke risk in primary prevention.[7] One-third of the adults in the USA have elevated low-density lipoprotein (LDL), leading to plaque formation in the intracerebral vasculature. Eventually, due to the excessive plaque build-up thrombotic strokes occur. In the older population, the risk of cardioembolic stroke increases mainly due to atrial fibrillation.[8] The rest 20% of strokes are hemorrhagic in nature. Hemorrhagic etiologies can be from hypertension, aneurysm rupture, arteriovenous malformations, venous angiomas, bleeding due to illicit drugs like cocaine, hemorrhagic metastasis, amyloid angiopathy, and other obscure etiologies.
Lacunar strokes contribute up about 20% of all ischemic strokes and result from occlusion of the small penetrating branches of the middle cerebral artery, vertebral or basilar artery or the lenticulostriate vessels. Typical causes of lacunar strokes include microemboli, fibrinoid necrosis secondary to vasculitis or hypertension, amyloid angiopathy, and hyaline arteriosclerosis.
Epidemiology
Stroke is the fifth leading cause of death in the US. The incidence of stroke is around 800,000 people annually. Stroke is the leading cause of disability.[9] The incidence of stroke has declined, but the morbidity has increased. Due to longer life expectancy, the lifetime risk of stroke is higher in women. Globally, at least 5 million people die from strokes and millions of others remain disabled.
Pathophysiology
Stroke is the result of ischemia in an area of the brain. The Na+/K+ ATPase pumps fail mainly because of the poor production of adenosine triphosphate (ATP) and failure of the aerobic mechanism. Ischemia leads to depolarization of cells which results in calcium influx into cells, elevated lactic acid, acidosis, and free radicals. Cell death increases glutamate and leads to a cascade of chemicals (excitotoxicity).[10]
History and Physical
The most important piece of historical information that the clinician should obtain is the time of symptoms onset or time last seen normal. This is critical because it determines the eligibility to receive rtPA or endovascular intervention for stroke. [11] Other important information to obtain is risk factors for arteriosclerosis and cardiovascular disease, diabetes, smoking, atrial fibrillations drug abuse, migraine, seizures, infection, trauma or pregnancy.
The stroke exam is a multi-person coordinated rapid exam. While staff obtain vitals, attach telemetry, and obtain IV access, the physician performs a rapid neurological evaluation. National Institutes of Health Stroke Scale (NIHSS) is routinely used to get the baseline evaluation. The exam has to be rapid as “time is brain.” One must examine the following items:
- The level of consciousness (alert and responsive, arouses to noxious stimuli, comatose…)
- Language (fluency, naming, comprehension, repetition)
- Dysarthria (slurring) which may be picked up in the history
- Motor (subtle arm weakness can be picked up by performing a pronator drift)
- Visual field deficits
- Eye movement abnormalities (in general if a gaze preference is present, the eyes deviate towards the side of the lesion)
- Facial paralysis (asking the patient to smile)
- Ataxia (finger to nose)
With a good history and physical exam, we can localize the stroke. There are various stroke syndromes.
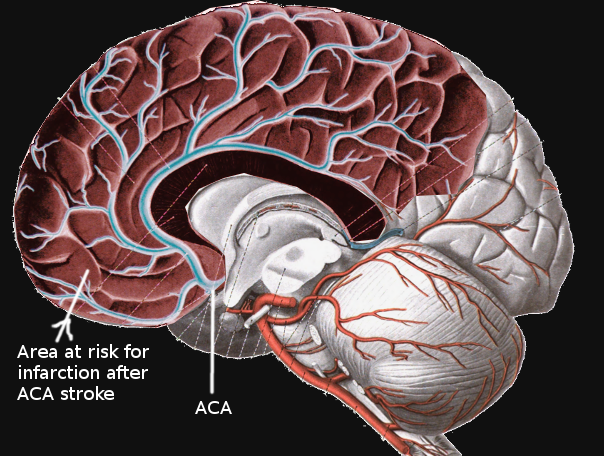
Anterior Cerebral Artery (ACA) Infarction
There is significant collateral blood supply in the ACA territory. So, pure ACA strokes are rare. The ACA distribution involves mainly Broca’s area, primary motor, primary sensory and pre-frontal cortex. So patients present with motor aphasia, personality issues, and contralateral leg weakness and numbness. Hand and face are usually spared.
Middle Cerebral Artery (MCA) Infarction
The MCA has the main trunk (M1) and it divides into two M2 Branches. The M1 (horizontal branch) supplies the basal ganglia and M2 (Sylvian branches) supplies part of the parietal, frontal and temporal lobes. As MCA supplies a wide territory it is extremely important to rule out MCA occlusion. The MCA syndrome causes contralateral arm and facial numbness and weakness, gaze deviation towards the affected side. Aphasia in the left-sided lesions and neglect in the right-sided lesions.
Posterior Cerebral Artery (PCA) Infarction
The PCA mainly supplies occipital lobe, thalamus and some portion of the temporal lobe. The classic presentation of PCA stroke is homonymous hemianopsia. Apart from this hypersomnolence, cognitive issues, the hemisensory loss can be seen when the deep PCA is involved. Some times there is bilateral infarction of distal PCAs producing cortical blindness and the patient is unaware of the blindness and denies it. This is called Anton-Babinski syndrome.[12]
Cerebellar Infarction
The patients with cerebellar strokes present with ataxia, dysarthria, nausea, vomiting, and vertigo.
Lacunar strokes are due to occlusion of small perforating vessels and can be a pure motor, pure sensory and ataxic hemiparetic strokes. In general, these strokes don't impair memory, cognition, level of consciousness or speech.
The stroke can be quantified by the NIHSS scale which includes the following:
- Visual function
- Level of consciousness
- Sensation and neglect
- Motor function
- Cerebellar function
- Language
A high score suggests proximal vessel occlusion.
Evaluation
The initial workup of a stroke patient involves stabilizing the Airway, Breathing, and Circulation (ABC). This is followed by a rapid, concise, history and exam such as the NIHSS which is administered simultaneously as the patient gets IV access, telemetry, and labs were drawn. The patient should then get a stat non-contrasted head computed tomogram (CT) or a combination of head CT, CT Angiography, and perfusion imaging. "Time is brain," and so we should not waste any time at all. Ideally, rtPA should be prepared as imaging is occurring, and as soon as the non-contrasted head CT can be visualized, and a bleed is excluded, rtPA should be administered after discussing the risks and benefits, and excluding rtPA contraindications. Time is critical, as only patients who get all the required studies within 4.5 hours qualify for potentially lifesaving thrombolysis. After IV rtPA, the CT angiography should be reviewed to determine if the patient qualifies for endovascular therapy as well.
The earliest CT sign of stroke is:
- A hyperdense segment of a vessel (direct visualization of the intravascular thrombus/embolus) - most often seen in the MCA (hyperdense MCA sign and MCA dot sign)
Interpretation of CT perfusion scan:
- Infarct core - Demonstrates matched defects in cerebral blood volume (CBV) and mean transit time (MTT)
- Ischemic penumbra - Prolonged MTT, but preserved CBV
Interpretation of magnetic resonance imaging (MRI) scan:
- Early hyperacute - Increased diffusion-weighted image (DWI) signal and reduced apparent diffusion coefficient (ADC) values
- Late hyperacute (>6 hours) - High T2 signal in fluid-attenuated inversion recovery (FLAIR) image
In recent years there are significant advancements in acute stroke care. Multiple stroke trials in 2015 showed that endovascular thrombectomy in the first six hours is much better than standard medical care in patients with large vessel occlusion in the arteries of the proximal anterior circulation. These benefits sustained irrespective of geographical location and patient characteristics.[13]
Again in 2018, a significant paradigm shift happened in stroke care. DAWN trial showed significant benefits of endovascular thrombectomy in patients with large vessel occlusion in the arteries of the proximal anterior circulation. This trial extended the stroke window up to 24 hours in selected patients using perfusion imaging. Due to this, we can treat more patients even up to 24 hours.[3]
All patients should be treated with an antiplatelet agent and a statin, and be admitted for full stroke evaluation. Hypertension is often seen in acute stroke. This should not be aggressively treated. A baseline electrocardiogram is recommended. The following labs would be indicated when a diagnosis of stroke is entertained:
- Basic metabolic panel (BMP)
- Complete blood count (CBC)
- Cardiac markers
- Coagulation profile: prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT)
- Lipid Panel
- Hemoglobin A1C
A transthoracic echocardiogram, telemetry monitoring, and neck vessel imaging are necessary to elucidate the etiology of stroke.
Treatment / Management
Acute ischemic stroke patients who meet the criteria for rtPA and do not have any contraindications should receive IV rtPA. Patients who have large vessel occlusions should be evaluated for possible endovascular intervention. All patients suspected of having an acute ischemic stroke should be admitted for a full neurological workup. Neurology consultation should be obtained. The workup of acute ischemic stroke includes a search for a source of thrombus, which includes carotid artery evaluation by ultrasound, CTA, MRA, or conventional angiography. A transthoracic echocardiogram is obtained to ascertain for low ejection fraction, the cardiac source of the clot, or patent foramen ovale. EKG and telemetry are obtained to ascertain for rhythms predisposing to stroke such as atrial fibrillation. Labs such as a fasting lipid panel, and hemoglobin A1C, are obtained to ascertain for modifiable risk factors for stroke. Other labs such as a hypercoagulable panel in young patients or B12 and syphilis testing in selected patients is also obtained. Antiplatelet and statins remain the mainstay of medical management of stroke.
For ischemic stroke, Alteplase (IV rtPA) within 4.5 hours of stroke onset is the standard of care.
The following patients are excluded from receiving IV rtPA, if they present between 3 and 4.5 hours:[14]
- Age >80 years
- Severe stroke (NIHSS > 25)
- History of diabetes and prior stroke
- Taking an oral anticoagulant regardless of INR
Contraindications for IV rtPA include:[14]
- Unclear time and/ or unwitnessed symptom onset
- Time last known to be at baseline state is >3 or 4.5 hours
- Current intracranial or subarachnoid hemorrhage
- Severe head trauma or ischemic stroke within 3 months
- Cranial or spinal surgery within 3 months
- Gastrointestinal malignancy or bleed within 21 days
- Active internal bleeding
- Coagulopathy (platelets <100 000/mm, INR >1.7, aPTT >40 s, or PT >15 s)
- Those who received a treatment dose of low molecular weight heparin within 24 hours.
- Infective endocarditis
- Direct thrombin inhibitors or direct factor Xa inhibitors
- Glycoprotein IIb/IIIa receptor inhibitors
- Intra-axial intracranial neoplasm
- Current severe uncontrolled hypertension (not maintained less than or equal to 185/110 mm Hg)
The indications for mechanical thrombectomy with a stent retriever in a patient >18 years of age include:[14]
- Minimal pre-stroke disability
- Causative occlusion of the internal carotid artery or proximal MCANIHSS of ≥6
- Reassuring non-contrast head CT [Alberta Stroke Program Early Computed Tomography Score (ASPECT) score of ≥6]
- If the patient can be treated within 6 hours of last known normal.
A notable potential complication after fibrinolytic therapy is hemorrhagic transformation. Hemorrhagic transformation is classified as hemorrhagic infarction and parenchymal hematoma, each with 2 subsets. Predictive factors for the occurrence of this complication include increased infarction area, gray matter location, atrial fibrillation, and cerebral embolism, acute hyperglycemia, low platelet count, and poor collateral circulation.[15]
Aspirin is recommended within 24-48 hours after stroke onset. Its administration can be delayed for 24 hours in patients treated with IV tPA. Mono/dual antiplatelet therapy is not a contraindication for receiving rtPA.
When to start anticoagulation in patients with atrial fibrillation after acute stroke is always a dilemma. Usually, it depends on various factors like the size of the stroke and other comorbidities. Usually, if the size of the stroke is smaller to moderate and no hemorrhage, we start anticoagulation in 7-14 days.[16]
Sometimes there are patients with small hemorrhagic transformation after acute stroke, and in this scenario, it is better to wait for anticoagulation for a couple of weeks. This delay is not associated with excessive stroke recurrence.[17]
For patients with significant disabilities, physical therapy and occupational therapy consults should be obtained. Similarly, if swallowing and speech are of concern, then speech/swallow consults should be obtained. All patients should have follow-ups arranged with their primary care providers, and with neurology at appropriate times post-discharge. For symptomatic and significant carotid artery stenosis, referrals to vascular or neurological surgery should be sought.
The patient's comorbidity has to be addressed and one should avoid hyperthermia. Oxygen supplementation is recommended when the oxygen saturation is less than 94%. Both hypo- and hyperglycemia need to be addressed as they can affect the outcome.
Significant cerebral edema can occur after stroke and thus a CT scan should be done in patients who have altered mentation. Mannitol can be used but there is no evidence to support the routine use of corticosteroids. Patient position, hyperosmolar therapy, hyperventilation, and barbiturate coma may be used to lower the intracranial edema.
Seizures occur in about 15% of patients within the first few days of the stroke. Those who develop chronic seizures need treatment.
it is important to understand that palliative care is also an important component of stroke management. Some patients have severe stroke and are incapacitated. Thus, one has to discuss the end-of-life, palliation, and do-not-resuscitation issues with the family.
Differential Diagnosis
The differential diagnosis is broad and can include stroke mimics such as:
- Transient ischemic attack (TIA)
- Hypoglycemia
- Hyponatremia
- Hemiplegic migraine
- Encephalitis
- Brain abscess
- Cerebral neoplasm
- Syncope
- Conversion disorder[15]
Prognosis
Stroke continues to carry high morbidity and mortality. One-year-survival for stroke varies from 60-80%. For those who survive, the recovery is prolonged and the risk of another stroke is high. Most patients following a stroke remain disabled or have partial neurological deficits that prevent them from being active in the workforce.
Complications
Complications after a stroke include worsening neurological status from the extension of the stroke or hemorrhagic conversion and a multitude of other complications associated with prolonged immobility and hospitalization. According to one multicenter study the incidence of complications after a stroke in the acute phase were:[18]
- Recurrent stroke - 9%
- Epileptic seizure - 3%
- Urinary tract infection - 24%
- Pneumonia - 22%
- Pressure sores - 21%
- Deep venous thrombosis - 2%
- Pulmonary embolism - 1%
- Depression - 16%
- Anxiety - 14%
Deterrence and Patient Education
Stroke prevention, either primary or secondary is the primary goal of treatment. Patients at the highest risk should be identified early and counseled on lifestyle changes as well as control of comorbid conditions to prevent this devastating outcome. Conditions that increase a patient's risk for cerebrovascular accidents include uncontrolled diabetes mellitus, uncontrolled hypertension, nicotine abuse, and atrial fibrillation. These are the most common and high prevalence diseases, however, other conditions are also linked to vascular pathologies such as vasculitis and certain autoimmune diseases. Primary care and specialty providers must diligently identify these patients and provide focused counseling as well as aggressive therapy for underlying diseases to prevent this outcome.
The American Stroke Association has suggested the acronym ACT FAST to recognize the early symptoms of a stroke. They include:
- F (Face) - A droop or an uneven smile on a person’s face.
- A (Arms) - Arm numbness or weakness - Elicited by asking the patient to lift the arms
- S (Speech difficulty) - Slurred speech or difficulty in understanding speech
- T (Time) - If any of the above features are present, even if transient, it is time to call the emergency helpline (911).
The additional symptoms of stroke to be watched for are:
- Sudden Numbness
- Sudden Confusion
- Sudden Trouble Seeing
- Sudden Trouble Walking
- Sudden Severe Headache
Pearls and Other Issues
Other issues to remember:
- A stroke generally presents with an acute focal neurologic deficit with no pain.
- The most important part of the history is the time of onset of symptoms.
- Rapid evaluation and treatment are paramount for the best outcomes.
- The use of a stroke rating scale, preferably the NIHSS, is recommended and the AHA / ASA recommends that all clinicians who care for stroke patients should be NIH Stroke Scale certified.
- IV rtPA is approved for use up to 4.5 hours following symptom onset, but the earlier the rtPA is administered, the better the outcomes.
- At a minimum, a non-contrasted head CT should be obtained to rule out hemorrhage before administering IV rtPA.
- The only lab needed before administering rtPA is a finger-stick serum glucose unless a bleeding diathesis or clinical situation warrants more labs.
- Endovascular or interventional therapy should be considered in patients who have significant deficits (NIHSS > 6) up to 6 hours following symptom onset if treatment can be initiated within 6 hours.
- The risk of intracranial hemorrhage in stroke mimics treated with IV rtPA is extremely low (~ 1%).
- For patients who do not qualify for rtPA, permissive hypertension is indicated for at least the first 24 hours, and blood pressure should not be lowered unless it exceeds 220/120.
- Before initiating rtPA, blood pressure should be gently lowered to a value below 185/110.
- After rtPA, blood pressure should be kept below 180/105 for 24 hours.
- For patients who do not receive rtPA, an antiplatelet agent and statin should be administered.
Enhancing Healthcare Team Outcomes
Stroke continues to carry high morbidity and mortality. In addition, the cost to the healthcare system is enormous. Even though treatments for strokes exist, the outcomes are not satisfactory and many people remain permanently disabled.
To improve outcomes, there is ample evidence indicating that the management of stroke is best done with an interprofessional team that includes the emergency department physician, nurse practitioner, neurologist, radiologist, and the stroke team. The key is to first identify if the stroke is embolic or hemorrhagic and then institute thrombolytic treatment accordingly. For those who recover, physical, speech and occupational therapy may be necessary.
Early identification of a stroke is crucial. The nursing staff must be trained to identify potential stroke victims and immediately contacting the clinician to evaluate the patient. Once the diagnosis is made, depending on the type, the clinicians should work with the pharmacist on rapid screening for medication interaction and then implement treatment as quickly as possible.
However, today the focus is on stroke prevention as it is more cost-effective. All clinicians have the responsibility for educating the public on methods to prevent strokes. The pharmacist should encourage blood pressure medication compliance since uncontrolled blood pressure is one of the risk factors for stroke. The clinicians including nurses should educate patients on discontinuing smoking, eating a healthy diet, exercising regularly and maintaining healthy body weight. Patients should be provided with supporting literature and educated about stroke and its complications.
For those who have developed a stroke, one may need to involve a social worker to ensure that the home is a safe place and that the patient has the support systems. A dietary consult should be made to educate the patient on what to eat. In addition, some patients may need to enroll in rehabilitation to regain speech, muscle and joint function. Only via an interprofessional team approach and open communication can this lead to improved outcomes and a better quality of life.
Outcomes
The outcomes for patients with mild embolic strokes are good but those with hemorrhagic strokes tend to have poor outcomes.[19][20](Level V)
(Click Image to Enlarge)
Contributed by Dr. Raju S. Menon (https://www.youtube.com/watch?v=V6cxZa6gy6g)
(Click Image to Enlarge)
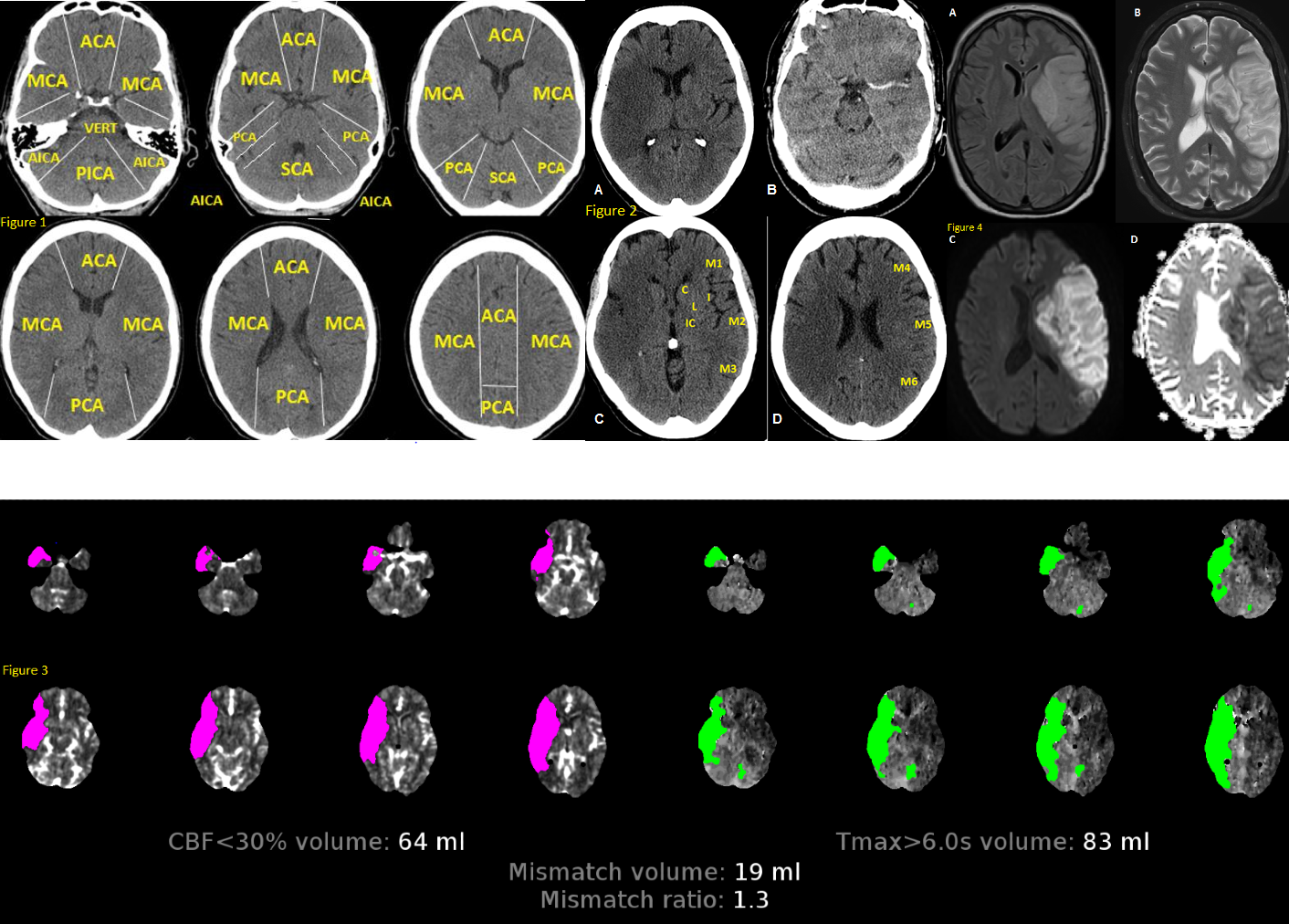
Fig 1. Anatomy of brain vascular territories. ACA: anterior cerebral artery; MCA: middle cerebral artery; PCA: posterior cerebral artery; AICA: anterior inferior cerebellar artery; PICA: posterior inferior cerebellar artery; SCA: superior cerebellar artery. Fig 2. Non-contrast CT shows loss of gray-white matter diffraction in the right MCA territory consistent with acute large right MCA infarction Fig 3. CTP in stroke imaging. The areas of increased MTT, TTP or Tmax and decreased CBV or CBF are considered as infarct core Fig 4. MRI in stroke. There is a large left MCA infarction. Infarction is hypersignal on FLAIR (A) and T2 (B) sequences. Also, there is a mass effect in favour of subacute infarction. The infarction shows “true” diffusion restriction: hyper signal on DWI (C) and hypo signal on ADC map (D).
Contributed by Omid Shafaat, M.D.