Subarachnoid Hemorrhage
- Article Author:
- Endrit Ziu
- Article Editor:
- Fassil Mesfin
- Updated:
- 8/8/2020 8:20:41 PM
- For CME on this topic:
- Subarachnoid Hemorrhage CME
- PubMed Link:
- Subarachnoid Hemorrhage
Introduction
Subarachnoid hemorrhage is an important type of head bleed that every physician should be aware of because it is important to provide fast and appropriate care to each patient. Subarachnoid hemorrhage is defined as blood between the arachnoid membrane and the pia membrane. Several factors compromise this syndrome. Most subarachnoid hemorrhages are traumatic in nature. Aneurysmal subarachnoid hemorrhage compromises a small portion of this patient population, but nevertheless is the most worrisome type of subarachnoid hemorrhage. History is the first clue to where the subarachnoid hemorrhage originated. Spontaneous subarachnoid hemorrhage should raise suspicion for aneurismal rupture. Most of the aneurysmal ruptures occur in patients older than 50 years old. While a severe headache during strenuous postcoital activity is a typical scenario, 30% of subarachnoid hemorrhage occurs during sleep. Occasionally subarachnoid aneurysmal hemorrhage is preceded by warning sharp, severe headache, or a sentinel headache, that happens a few weeks before the rupture. It is challenging to distinguish a sentinel headache from other headaches, but an intense headache in a patient that is not prone to headaches should raise suspicion for further imaging. While subarachnoid hemorrhage is typical of aneurysmal rupture, often is also associated with intraventricular hemorrhage, intracerebral hemorrhage, and subdural hematoma. The force of the rupture and location of an aneurysm determine the presence of the other types of hemorrhage. The interesting unexplained fact is that most of the aneurysmal hemorrhage occurs during the spring and autumn season. While caring for a patient with a diagnosis of subarachnoid hemorrhage, a physician should be highly suspicious and promptly evaluate the patient when changes in mental status are noted. This patient population is prone to seizures as well as to hydrocephalus and vasospasm, both potentially devastating factors.[1][2][3]
Etiology
Trauma causes the highest incidence of subarachnoid hemorrhage. Non-traumatic subarachnoid hemorrhage is mostly due to vascular malformation. Aneurysmal hemorrhage is the biggest player in this subgroup. To a lesser extent, patients experience subarachnoid hemorrhage after using certain drugs like cocaine. After practitioners complete evaluation in these cases, about 10% do not have a clear identifying factors. Determining the precise etiology of the hemorrhage is very important, as practitioners can tailor treatment to the cause of hemorrhage. Response to treatment varies, for example, for subarachnoid hemorrhage stemming from vasospasm.[4][5]
Epidemiology
The incidence of subarachnoid hemorrhage in the United States is between 10 to 14 for 100,000 population per year. Incidence is slightly higher in women, 1.3 compared to men. It is more prevalent in black and Hispanic populations than in white populations. Around the world, Japan and Finland have higher cases of subarachnoid hemorrhage, but the reason is unknown. Several factors are associated with subarachnoid hemorrhage, hypertension, cigarette smoking, excessive alcohol consumption, gender, age, genetic syndromes like Ehlers-Danlos, and polycystic kidney disease. Among the above-stated factors, the history of a previously ruptured intracerebral aneurysm is very highly associated with new subarachnoid hemorrhage. The second highest association is between smoking and subarachnoid hemorrhage.
Pathophysiology
Am initial inciting event releases blood into the subarachnoid space. Blood close to the brain surface is an irritant, and many complications of subarachnoid hemorrhage are due to the irritant effect of blood on the brain. Responses include seizures, vasospasm, and confusion. Subarachnoid hemorrhage has effects outside the brain. Two prominent features of this disease are neurogenic pulmonary edema and neurogenic stunned myocardium. Blood products eventually circulate with cerebral spinal fluid and in many cases impede normal fluid clearance in arachnoid granulations. When these events happen, resultant hydrocephalus ensues. If hydrocephalus is not treated in timely fashion fluid collection in the ventricular system will eventually create enough pressure to cause brain herniation syndromes and possible death. Neurosurgical intervention should be the priority when hydrocephalus is identified.
History and Physical
A typical presenting symptom is a thunderclap headache. During a medical interview, patients usually call it the “worst headache of my life.” This problem should prompt further imaging. A headache often is associated with nausea, vomiting, and diplopia. Quite often signs of meningismus are present due to irritant blood spreading into the fourth ventricle and further down the spinal cord irritating nerves and causing neck and back pain. Cranial nerve deficits can occur. Practitioners should perform a detailed exam. The presence of a focal deficit increases the grade of subarachnoid hemorrhage and changes the perspective of post-event recovery. Patients with a high-grade subarachnoid hemorrhage quite often present in a state of coma that calls for a quick evaluation and urgent treatment, as the coma can be reversible. In addition to subarachnoid hemorrhage patients could have an intraocular hemorrhage, initially described and named after French ophthalmologist Albert Terson. When the physician identifies Terson syndrome, an ophthalmology service should be consulted to help with the care of the patient. Eighty percent of patients that develop Terson syndrome do not require further interventions other than regular follow-ups.
Evaluation
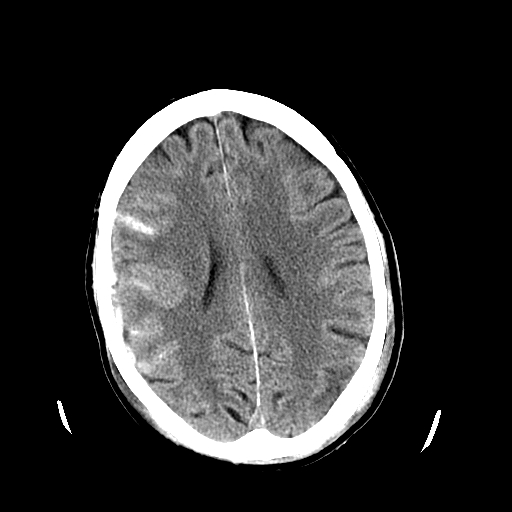
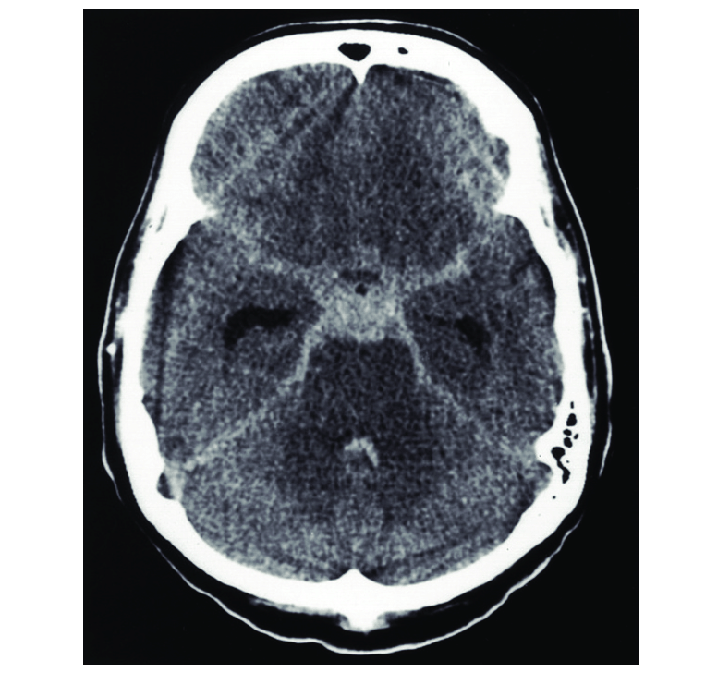
Initial evaluation of a patient suspected of having a subarachnoid hemorrhage should include head computed tomogram (CT). A CT angiography should be added if a subarachnoid hemorrhage is identified. If the initial CT is negative, but a physician has a very high suspicion for hemorrhage, a lumbar puncture should be performed and sent for laboratory evaluation of xanthochromia presence. Sometimes xanthochromia presence can be assessed at the bedside due to visible cerebrospinal fluid color change. A CT angiography diagnosis of an aneurysm or confirmation of negative CT angiography should be followed by cerebral angiography or digital subtraction angiography (DSA). A few factors should be considered in patients who are allergic to contrast or have decreased renal function. These patient populations need pre-procedure treatment to decrease the chances of an adverse reaction. Time-of-flight magnetic resonance angiography (TOF-MRA) is another acceptable mode of imaging that will not require contrast injection but due to the long time that is necessary to obtain complete examination is not always a feasible alternative in very sick patients with subarachnoid hemorrhage.[6][7][8]
Treatment / Management
Treatment of subarachnoid hemorrhage patients should occur in the intensive care unit. On the initial presentation, Hunt and Hess, as well as the World Federation of Neurological Surgeons scores, should be determined. If there is the presence of hydrocephalus, the placement of an external ventricular drain should be considered. Level one evidence supports the use of nimodipine and maintenance euvolemia as important factors to improve outcomes. Tight control of blood pressure until an aneurysm is also secured is necessary. Blood pressure should be less than 160 mmHg and more optimally within the 140-mmHg range. Seizure prophylaxis should be initiated, as 20% of these patients will seize within the first 24 hours post bleed. Seizure, while an aneurysm is unsecured, will worsen patient outcomes. Avoid hyponatremia and hypovolemia and initiate fluids as soon as intravascular access is obtained. Normal saline has shown slight benefits when compared to other fluids like Ringer's lactate solution. Monitor pulmonary status. Often the patient has been intubated in the field by emergency services, but if the patient has been not intubated and the Glasgow coma scale (GCS) score is less than eight, initiate steps to secure an airway. Consider an arterial line to have better control of patient hemodynamic status. Early intervention to secure an aneurysm will allow relaxing blood pressure goals and improving cerebral perfusion pressure which is severely compromised in these patients. The use of prothrombotic agents like aminocaproic acid is surgeon dependent and will need to be considered if an aneurysm cannot be secured within a short time.[9][10][11][12]
Differential Diagnosis
- Bacterial and tuberculous meningitis
- Granulomatous meningitis
- Neurosarcoidosis
- Pseudo-subarachnoid hemorrhage
Prognosis
The prognosis depends on the cause and grade of subarachnoid hemorrhage, and the presence of other complications.
Complications
- Seizures
- Vasospasm
- Rebleed
- Hydrocephalus
- Increased intracranial pressure
- Brain herniation
- Cerebral infarction
- Medical complications
- Neurogenic pulmonary edema[13]
- Death
Deterrence and Patient Education
A patient with an aneurysm, who is being conservatively managed should be advised on all the complications that can occur if it ruptures.
Any patient and relatives getting admitted with subarachnoid hemorrhage secondary to an aneurysm rupture should be aware of the chance of rebleed and the morbidity and mortality associated with any intervention.
Enhancing Healthcare Team Outcomes
The majority of patients with subarachnoid hemorrhage present to the emergency department. Thus, it is vital that the emergency department physician and nurse practitioner know the workup for these patients. Because of the very high mortality, an interprofessional team that includes a neurosurgeon, interventional radiologist, neurologist, intensivist, and Intensive Care Unit nurses is recommended. Unfortunately, despite the optimal case, the majority of patients die within 30 days. Even those who survive are left with severe complications that are disabling.[14][15] (Level V)
(Click Image to Enlarge)