Subclavian Artery Thrombosis
- Article Author:
- Ateeq Mubarik
- Article Editor:
- Arshad Muhammad Iqbal
- Updated:
- 8/15/2020 11:37:50 PM
- For CME on this topic:
- Subclavian Artery Thrombosis CME
- PubMed Link:
- Subclavian Artery Thrombosis
Introduction
There is a pair of large arteries in the thorax arising from the arch of the aorta (left) and brachiocephalic trunk (right) known as subclavian arteries. The subclavian artery continues as the axillary artery. It gives off various branches including the vertebral arteries, which supply about 20% of blood to the brain.[1] Like many other arteries, the subclavian artery is also prone to disease, and one common problem is subclavian artery thrombosis.
Subclavian artery thrombosis is typically underdiagnosed by physicians. Harrison, in 1829 was the first to uncover stenosis of the initial segment of the subclavian artery.[2] Bachman and Kim, in 1980 performed the first angioplasty of the subclavian artery.[3] The disease is more common in the left subclavian artery by four-fold as compared to the right. Subclavian artery stenosis can cause significant ischemic symptoms in the upper extremities, brain, and rarely in the heart.
Etiology
The most widely recognized etiology for subclavian artery thrombosis is atherosclerosis; other uncommon etiologies are inborn deformities, fibro-muscular dysplasia, neurofibromatosis, autoimmune vasculitis-like Takayasu, radiation exposure, neurofibromatosis, and mechanical causes including injury or compression disorders.[4]
Epidemiology
The incidence of subclavian artery thrombosis in a patient with peripheral vascular disease is approximately 11 to 18%.[5] Likewise, the patient with subclavian artery thrombosis will have a 50% chance of having coronary artery disease, 27% for lower extremity artery disease, and 29% for carotid artery disease.[6] Because of the common pathogenesis, the patients with subclavian artery thrombosis have an elevated risk for coronary artery disease, transient ischemic attack, and cerebrovascular ischemia or infarct, and this risk correlates more with the left-sided lesion.[7][8][9]
Pathophysiology
The risk factors for subclavian artery thrombosis are the same as thrombosis in any other site of the body. The main risk factors are obesity, hypertension, diabetes mellitus, smoking, and metabolic syndrome. Similar to other artery thromboses, subclavian artery thrombosis also involves an area subjected to increased shear stress leading to endothelial injury and subsequent platelet aggregation and release of platelet-derived growth factor. This sequence triggers the proliferation of smooth muscle cells in the arterial intima and forms the locus of the atherosclerotic plaque.
History and Physical
The presence of symptoms depends on collateralization. Upper limb symptoms comprise arm claudication or muscle fatigue, rest pain and finger necrosis from embolic debris. Characteristic neurologic symptoms include vertebrobasilar hypoperfusion including visual abnormalities (diplopia), drop attacks, syncope, ataxia, vertigo, dysphasia, dysarthria, dizziness, nystagmus, tinnitus, hearing loss, and facial sensory deficits. Vertebrobasilar insufficiency develops when subclavian artery thrombosis is distal to the origin of the vertebral artery; thus, during conditions of increased flow distal to the stenosis like exercise, results in retrograde flow in the vertebral artery, followed by decreased flow in the basilar artery.
One of the rare complications of subclavian stenosis develops in a patient who has had coronary artery bypass surgery with the internal mammary artery (IMA) graft is angina pectoris. The internal mammary artery arises from the subclavian artery and can be affected by stenosis. If there is subclavian artery thrombosis proximal to the IMA graft, flow impairment to the IMA may occur. In instances of severe stenosis, retrograde flow from the grafted coronary artery to the brachial artery may lead to angina; a phenomenon called coronary steal syndrome.
Physical examination particularly cardiovascular examination may reveal unequal blood pressure in arms, absent or diminished pulses (axillary, brachial and radial/ulnar) compared to the contralateral arm, and cervical or supraclavicular bruits. Ischemic findings such as gangrenous skin changes of the fingers or splinter hemorrhages of the nail bed may also present. The examination should also focus on the cerebral circulation including palpation of carotid pulses and auscultation for vertebral (suboccipital region) and carotid bruits.
The inter-arm systolic blood pressure difference of less than 10mm Hg has a negative predictive value of 99%.[5]
Evaluation
The goal standard diagnostic modality is imaging. However, diagnosis is possible from clinical findings which may suggest possible subclavian artery thrombosis, including unequal upper limb blood pressures, absent or diminished axillary, brachial, radial or ulnar pulses, and digital ulceration or gangrene.
The difference of systolic blood pressure of over 10 mm Hg between both the arms has a positive predictive value of 13%.[5] However, if the systolic cut-off increases to 15 or 20 mm Hg, positive predictive value increases to 67% to 100% and negative predictive value up to 100%.[10][11]
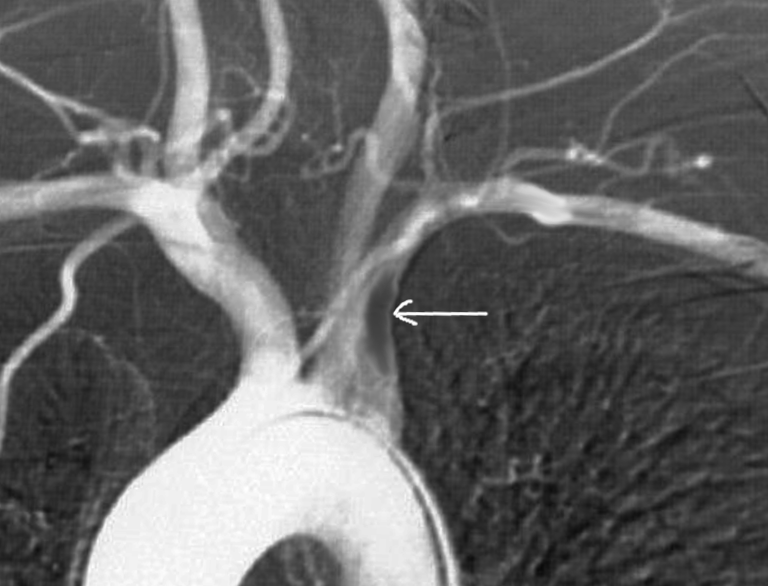
Non-invasive diagnostic imaging for the diagnosis of subclavian artery thrombosis is duplex ultrasound with color flow. Duplex ultrasonography shows waveform dampening or monophasic changes, color aliasing suggestive of turbulent flow, and increased blood flow velocities at the location of the stenosis. Doppler ultrasonography can also diagnose a reversal of ipsilateral vertebral artery flow as seen in subclavian steal syndrome.
More accurate diagnostic modalities include computed tomography angiography and magnetic resonance angiography, reserved for when intervention is mandatory.
The recommendations for screening include when a patient is undergoing coronary artery revascularization using the intermammary artery such as CABG, and the suspicion of subclavian stenosis is high, or if a patient has a history of peripheral artery disease or systolic blood pressure differences in their upper limbs of over 10 mm Hg.[12]
Treatment / Management
Indications for the treatment are as follows;
- Morbid upper arm ischemia (57%)
- Upper limb claudication
- Upper extremity pain at rest
- Fingers embolization
- Vertebrobasilar insufficiency from steal syndrome (37%)
- Anginal symptoms from coronary steal via Intermammary artery graft (21%)
- Leg claudication in the presence of axillofemoral graft
Medical therapy includes antiplatelet including aspirin or clopidogrel, HMG-CoA reductase inhibitors, and either angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers. The patient counseled against smoking, and if diabetes is present, strict glycemic control is advisable with the target HbA1c of less than 7.[4]
Surgical treatment is sometimes necessary. In 1951, Shimizu and Sano first reported surgical repair of subclavian artery thrombosis.[13] The different options to correct subclavian artery pathology include:
- Axillary–axillary bypass
- Carotid-subclavian bypass
- Transposition of the subclavian artery
The axillary–axillary bypass surgery has a good prognosis in terms of morbidity and mortality.[14]
Endovascular intervention is the best modality currently for relieving subclavian artery thrombosis including percutaneous transluminal angioplasty with stenting or ballooning.[15]
Differential Diagnosis
- Congenital malformations
- Fibromuscular dysplasia
- Neurofibromatosis
- Autoimmune vasculitis like Takayasu
- Radiation exposure
- Mechanical causes like trauma or compression syndromes
Prognosis
The prognosis is good with early intervention, before the development of complications.
Complications
The complications of subclavian artery thrombosis are the following:
- Morbid upper arm ischemia (57%)
- Upper limb claudication
- Upper extremity pain at rest
- Fingers embolization
- Vertebrobasilar insufficiency from steal syndrome (37%)
- Anginal symptoms from coronary steal via Intermammary artery graft (21%)
- Leg claudication in the presence of axillofemoral graft
Procedural complications are as follows:
- Stroke
- Subclavian artery dissection
- Transient ischemic attack (TIA)
- Distal emboli
- Thrombosis
- Hematoma
- Bleeding
- Access site infection or bleeding
Deterrence and Patient Education
Smoking cessation is paramount in cases of atherosclerosis. The patient should receive counsel and education regarding the dangerous consequences of continued smoking which can literally threaten both life and limb due to the progression of atherosclerosis to other vasculature of the body.
Enhancing Healthcare Team Outcomes
Subclavian artery thrombosis is a rare presentation, but when it occurs, it is often symptomatic. The condition is best managed by an interprofessional team that includes a cardiologist, radiologist, vascular surgeon, and an interventionalist. It is essential to treat the condition causing the subclavian artery thrombosis, and this will also include reducing risk factors like smoking, hypertension, hyperlipidemia, and diabetes.