Anatomy, Thorax, Superior Vena Cava
- Article Author:
- Hunter White
- Article Editor:
- Michael Soos
- Updated:
- 8/15/2020 11:34:55 PM
- For CME on this topic:
- Anatomy, Thorax, Superior Vena Cava CME
- PubMed Link:
- Anatomy, Thorax, Superior Vena Cava
Introduction
The superior vena cava is a large, significant vein responsible for returning deoxygenated blood collected from the body back into the heart. It is present within the superior and middle mediastinum. The superior vena cava handles the venous return of blood from structures located superior to the diaphragm. The inferior vena cava handles venous return from the portion of the body inferior to the diaphragm. The superior vena cava is a commonly used site for central venous access.[1]
Structure and Function
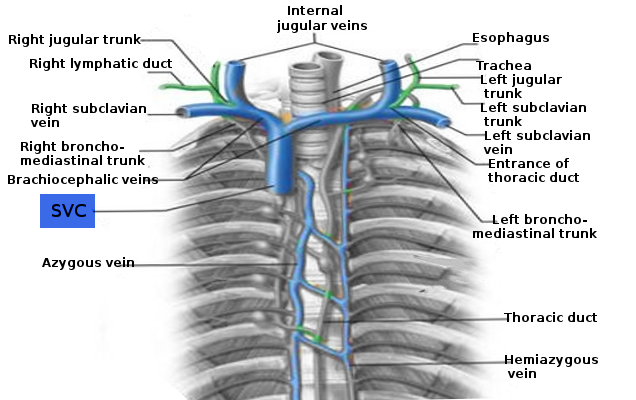
The right and left brachiocephalic veins, also known as the innominate veins, join to form the superior vena cava posterior to the inferior border of the first right costal cartilage. These veins carry blood from the chest wall, esophagus, lungs, neck, and pericardium. The superior vena cava descends downwards vertically, running posterior to the second and third intercostal spaces. The azygos vein drains into the superior vena cava via the azygos arch when it is behind the first intercostal space, just prior to the point at which it penetrates the fibrous pericardium that is located opposite the right second costal cartilage. It drains into the right atrium at the level of the third costal cartilage. The lower portion of the superior vena cava is covered by this fibrous pericardium. The superior vena cava terminates in the superior and posterior portion of the sinus venarum of the right atrium. There are no valves present at the point at which the superior vena cava drains into the right atrium. The superior vena cava is approximately 7 centimeters in length and 2 cm wide.[2]
Embryology
The superior vena cava derives from the proximal portion of the right anterior cardinal vein and the right common cardinal vein at a point that is caudal to the transverse anastomosis in the embryo. During week eight of development, a large anastomosis that formed via the thymic and thyroid veins shunts blood from the left anterior cardinal vein towards the right. Superior to this anastomosis, the anterior cardinal veins become the internal jugular veins. The cardinal veins are responsible for venous return; they represent the primary drainage system during embryonic development. The anterior cardinal veins drain the cephalic portion of the embryo while the posterior cardinal veins drain the remaining embryonic blood. The anterior and posterior cardinal veins merge before entering the sinus venosus. At this point, they become the short common cardinal veins. The right brachiocephalic vein forms from the right anterior cardinal vein at a point that is cranial to the transverse anastomosis. The left brachiocephalic vein forms from a portion of the left anterior cardinal vein and transverse intercardinal anastomosis. During embryonic development, several malformations may occur including left superior vena cava, double superior vena cava, as well as improper pulmonary venous drainage into the super vena cava.
Blood Supply and Lymphatics
The right and left brachiocephalic, or innominate, veins converge to form the superior vena cava at the level of the right first costal cartilage. These veins form at the venous angle from a merging of the subclavian and jugular veins posterior to the sternoclavicular joints. The brachiocephalic veins carry deoxygenated blood that is returning to the heart from the pericardium, lungs, esophagus, chest wall, and neck. The left brachiocephalic vein is more horizontal in its orientation and is longer than the more vertical and shorter right brachiocephalic vein. The right brachiocephalic vein is approximately 2 to 3 cm long and sits anterior to the innominate artery. The left brachiocephalic vein is approximately 6 cm long and lies anterior to the left subclavian vein and common carotid arteries, posterior to the manubrium, and superior to the aortic arch. The left superior intercostal vein joins with the left brachiocephalic vein; the azygos vein joins with the right brachiocephalic vein. The vertebral, internal thoracic, and inferior thyroid veins are all tributaries of the brachiocephalic veins.[2]
The azygos vein is another vein that drains into the superior vena cava. This vein is unpaired. It runs along the right aspect of the thoracic vertebral column and enters into the thorax at the aortic hiatus of the diaphragm. The azygos vein forms from the joining of the right subcostal and ascending lumbar veins. The hemiazygos veins, bronchial veins, pericardial veins, esophageal veins, and posterior right intercostal veins all drain into the azygos vein.
Nerves
Sympathetic axons originating from the right stellate ganglion descend along the superior vena cava. Most of these axons travel to the posterior surface of the heart. However, some extend onto the anterior side of the heart. These axons provide sympathetic innervation for the sinoatrial node. Cardiac parasympathetic nerves also run along the length of the superior vena cava. Efferent vagal nerve fibers travel through a pad of fat located in between the proximal aorta and medial superior vena cava.[3][4][5]
Muscles
As with other arteries and veins, the superior vena cava is made up of three total layers of muscle. The innermost endothelial lining of the superior vena cava is known as the tunica intima. The middle layer, comprised of smooth muscle tissue, is known as the tunica media. This is the layer that receives input from the nervous system. The outermost layer is the tunica adventitia. It consists of collagen and elastic connective tissue. It is this outmost layer that is primarily responsible for the superior vena cava’s flexibility.
Physiologic Variants
One physiological variation that can occur is known as left superior vena cava. This condition develops when the left anterior cardinal vein fails to disappear with development while the right common cardinal vein, as well as the right anterior cardinal vein, disappear. Another defect known as double superior vena cava occurs when the left anterior cardinal vein fails to disappear during normal embryological development. As a result, the left brachiocephalic vein does not form. Abnormal pulmonary venous return is also possible and would potentially result in the pulmonary veins draining into the superior vena cava.
Surgical Considerations
Obstructions of the superior vena cava via mediastinal mass or thrombus may require surgical correction. Trauma to the thoracic region, damage from long-term central line catheterization, or damage from chronic use of pacing electrodes can also result in a need for surgical repair of the superior vena cava. Great care is necessary when clamping off the superior vena cava for surgical repair as venous return from the head and neck will be impaired under these circumstances, and such impairment could potentially lead to poor patient outcomes.[6]
Clinical Significance
Complete or partial obstruction of the superior vena cava can occur, resulting in a condition known as superior vena cava syndrome. Causes of the obstruction may include intrinsic stenosis, extrinsic compression, or thrombosis of the vein. Malignancy is the single most common cause with cancer of the lung, lymphoma, or metastatic cancers resulting in the majority of superior vena cava obstructions.
The clinical presentation of superior vena cava syndrome may vary widely and depends on a variety of factors including the severity, speed, and location of the obstruction. Patients with a slowly developing obstruction may show few or no symptoms. These patients may develop collateral channels for blood flow to restore their venous return. The location of these collateral channels depends upon the location of the blockage. If the obstruction occurs in the area of the superior vena cava located before the azygos vein, the right superior intercostal veins will serve as the primary collateral pathway for azygos vein drainage. This pathway is often the most asymptomatic. If the obstruction occurs at the azygos vein, collateral channels will form between the superior vena cava and inferior vena cava via the internal mammary veins, superior and inferior epigastric veins, and the iliac vein. If the obstruction occurs past the point at which the azygos vein drains into the superior vena cava the blood will move via channels from the azygos and hemiazygos veins into the ascending lumbar and lumbar veins which will drain into the inferior vena cava and allow return into the right atrium.[7][8]
When this large-bore vein suffers more acute obstruction, it can result in upstream effects causing tributary veins in the head and neck to appear enlarged. It can also result in clinical symptomology that may include shortness of breath, cough, angina, facial flushing, headache, bilateral upper extremity swelling, and dysphagia. Patients with an obstructed superior vena cava may have a positive Pemberton sign. Treatment of the obstruction depends on the cause. In the context of cancer, chemotherapy, or radiation are options. In the event of a thrombus, anticoagulation may be indicated to prevent further clot formation. Stent placement is considered a first-line treatment option. CT is the imaging modality of choice for diagnosis of a superior vena cava obstruction. Plain radiographs may also be used to detect indirect signs of a mediastinal mass, but are not ideal.[8][9][10][11]