Anatomy, Joints
- Article Author:
- Pallavi Juneja
- Article Author:
- Akul Munjal
- Article Editor:
- John Hubbard
- Updated:
- 7/27/2020 12:12:15 PM
- For CME on this topic:
- Anatomy, Joints CME
- PubMed Link:
- Anatomy, Joints
Introduction
A joint is a point where two bones make contact. Joints can be classified either histologically on the dominant type of connective tissue functionally based on the amount of movement permitted. Histologically the three joints in the body are fibrous, cartilaginous, and synovial. Functionally the three types of joints are synarthrosis (immovable), amphiarthrosis (slightly moveable), and diarthrosis (freely moveable). The two classification schemes correlate: synarthroses are fibrous, amphiarthroses are cartilaginous, and diarthroses are synovial.[1][2]
Fibrous Joint
A fibrous joint is a fixed joint where fibrous tissue comprised primarily of collagen connects bones. Fibrous joints are usually immoveable (synarthroses) and have no joint cavity. They are subdivided further into sutures, gomphoses, and syndesmoses.
- Sutures are immobile joints in the cranium. The plate-like bones of the skull are slightly mobile at birth because of the connective tissue between them, termed fontanelles. This initial flexibility allows the infant’s head to get through the birth canal at delivery and permits the enlargement of the brain after birth. As the skull enlarges, the fontanelles reduce to a narrow layer of fibrous connective tissue, called Sharpey’s fibers, that suture the bony plates together. Eventually, cranial sutures ossify- the two adjacent plates fuse to form one bone; this fusion is termed synostosis.
- Gomphoses are the immobile joints between the teeth and their sockets in the mandible and maxillae. The periodontal ligament is the fibrous tissue that connects the tooth to the socket.
- Syndesmoses are slightly movable joints (amphiarthroses). In syndesmosis joints, the two bones are held together by an interosseous membrane. For example, the tibia connects to the fibula, forming the middle tibiofibular joint, and the ulna attaches to the radius, forming the middle radio-ulnar joint.
Cartilaginous Joint
In cartilaginous joints, the bones attach by hyaline cartilage or fibrocartilage. Depending on the type of cartilage involved, the joints further classify as primary and secondary cartilaginous joints.
- Primary cartilaginous joints, also known as synchondroses, only involve hyaline cartilage. These joints may be slightly mobile (amphiarthroses) or immobile (synarthroses). The joint between the epiphysis and diaphysis of growing long bones is an example.
- The secondary cartilaginous joint, also known as symphysis, may involve either hyaline or fibrocartilage. These joints are slightly mobile (amphiarthroses). A classic example is the pubic symphysis.
Synovial Joint
Synovial joints are freely mobile (diarthroses) and are considered the main functional joints of the body. Its joint cavity characterizes the synovial joint. The cavity is surrounded by the articular capsule, which is fibrous connective tissue that is attached to each participating bone just beyond its articulating surface. The joint cavity contains synovial fluid, secreted by the synovial membrane (synovium), which lines the articular capsule. Hyaline cartilage forms the articular cartilage, covering the entire articulating surface of each bone. The articular cartilage and the synovial membrane are continuous. Some synovial joints also have associated fibrocartilage, such as menisci, between articulating bones.
Synovial joints are often further classified by the type of movements they permit. There are six such classifications: hinge (elbow), saddle (carpometacarpal joint), planar (acromioclavicular joint), pivot (atlantoaxial joint), condyloid (metacarpophalangeal joint), and ball and socket (hip joint).
Structure and Function
The histological and functional classification schemes offer a broad understanding of joints. Within these categories, each specific joint type (suture, gomphosis, syndesmosis, synchondrosis, symphysis, hinge, saddle, planar, pivot, condyloid, ball, and socket) has a specific function in the body.
Of the fibrous joints, sutures and gomphoses are found only in the skull and the teeth, respectively.
Fibrous: Syndesmosis
A syndesmosis, an amphiarthrosis joint, and the third type of fibrous joint maintain integrity between long bones and resists forces that attempt to separate the two bones. All syndesmoses are amphiarthroses, but each specific syndesmosis joint permits a different degree of movement. For example, the tibiofibular syndesmosis primarily provides strength and stability to the leg and ankle during weight-bearing; however, the antebrachial interosseous membrane of the radioulnar syndesmosis permits rotation of the radius bone during forearm movements. The interosseous membranes of the leg and forearm are also areas of muscle attachment.
Cartilaginous: Synchondrosis
A synchondrosis, or primary cartilaginous joint, only involves hyaline cartilage and can be temporary or permanent.
A temporary synchondrosis is an epiphyseal plate (growth plate), and it functions to permit bone lengthening during development. The epiphyseal plate connects the diaphysis (shaft of the bone) with the epiphysis (end of the bone) in children. Over time, the cartilaginous plate expands and is replaced by bone, adding to the diaphysis. Eventually, when all the hyaline cartilage has ossified, the bone is done lengthening ad the diaphysis and epiphysis fuse in synostosis. Other temporary synchondroses join the ilium, ischium, and pubic bones of the hip; over time, these also fuse into a single hip bone.
A permanent synchondrosis does not ossify with age; it retains its hyaline cartilage. Permanent synchondroses function to connect bones without movement as a synarthrosis joint. Examples include the thoracic cage, such as the first sternocostal joint: the first rib is joined to the manubrium by its costal cartilage. Other examples include the relationship between the anterior end of the other 11 ribs and the costal cartilage.
Cartilaginous: Symphysis
A symphysis, or secondary cartilaginous joint, involves fibrocartilage. Fibrocartilage is thick and strong, so symphyses have a great ability to resist pulling and bending forces. While the fibrocartilage strongly unites adjacent bones, the joint is still an amphiarthrosis joint and permits limited movement.
Symphysis can be narrow or wide. Narrow symphyses include the pubic symphysis and the manubriosternal joint. In females, the slight mobility of the pubic symphysis between the left and right pubic bones is critical for childbirth. A wider symphysis is the intervertebral symphysis or intervertebral disc. The thick pad of fibrocartilage fills the gap between adjacent vertebrae and provides cushioning during high-impact activity.
Synovial: Overview
The primary purpose of the synovial joint is to prevent friction between the articulating bones of the joint cavity. While all synovial joints are diarthroses, the extent of movement varies among different subtypes and is often limited by the ligaments that connect the bones.
Synovial: Hinge
A hinge joint is an articulation between the convex end of one bone and the concave end of another. This type of joint is uniaxial because it only permits movement in one axis. In the body, this axis of movement is usually bending and straightening, or flexion and extension. Examples include the elbow, knee, ankle, and interphalangeal joints.
Synovial: Condyloid
A condyloid joint, or an ellipsoid joint, is defined as an articulation between the shallow depression of one bone and the rounded structure of another bone or bones. This type of joint is biaxial because it permits two axes of movement: flexion/extension and medial/lateral (abduction/adduction). An example is the metacarpophalangeal joints of the hand between the distal metacarpal and proximal phalanx, commonly known as the knuckle.
Synovial: Saddle
A saddle joint is an articulation between two bones that are saddle-shaped, or concave in one direction and convex in another. This type of joint is biaxial, and one example is the first carpometacarpal joint between the trapezium (carpal) and the first metacarpal bone of the thumb. This arrangement permits the thumb to flex and extend (within the plane of the palm) as well as abduct and adduct (perpendicular to the palm). This dexterity gives humans the characteristic trait of “opposable” thumbs.
Synovial: Planar
A planar joint, or gliding joint, is defined as an articulation between bones that are both flat and of similar size. This type of joint is multiaxial because it permits many movements; however, surrounding ligaments usually restrict this joint to a small and tight motion. Examples include intercarpal joints, intertarsal joints, and the acromioclavicular joint.
Synovial: Pivot
A pivot joint is an articulation within a ligamentous ring between the rounded end of one bone and another bone. This type of joint is uniaxial because, although the bone rotates within this ring, it does so around a single axis. An example would be the atlantoaxial joint between C1 (atlas) and C2 (axis) of the vertebrae, permitting side-to-side head motion. Another example is the proximal radioulnar joint. The radius sits in the annular radial ligament, which holds it in place as it articulates with the radial notch of the ulna, which permits pronation and supination.
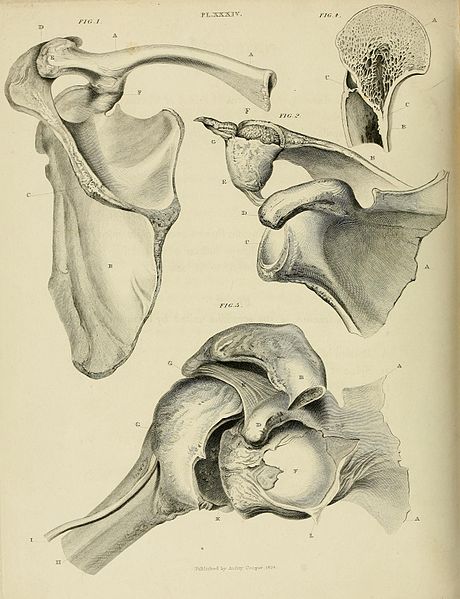
Synovial: Ball and Socket
A ball and socket joint is an articulation between the rounded head of one bone (ball) and the concavity of another (socket). This type of joint is multiaxial: it permits flexion/extension, abduction/adduction, and rotation. The only two ball and socket joints of the body are the hips and the shoulder (glenohumeral). The shallow socket of the glenoid cavity permits a more extensive range of motion in the shoulder; the deeper socket of the acetabulum and the supporting ligaments of the hip constrain the movement of the femur.
Embryology
Joints, comprising bones and connective tissue, are embryologically derived from mesenchyme. The bones either develop directly through intramembranous ossification or indirectly through endochondral ossification. During direct development, the mesenchymal cells differentiate into bone-producing cells. During indirect development, the mesenchymal cells first differentiate into hyaline cartilage, which is then gradually displaced by bone. The connective tissue of the joint arises from the mesenchymal cells between the developing bones.
For synovial joints of the limbs, the space between the developing long bones is termed the joint interzone. The interzone becomes apparent in the sixth week of embryonic development when a cellular condensation of mesoderm on either side, termed the paraxial blastema, chondrifies into hyaline cartilage models for the long bones. In the eighth week of embryonic development, mesenchymal cells at the margin of the interzone become the articular capsule; cell death in the center forms the joint cavity, which is filled with synovial fluid produced by mesenchymal cells. The articular cartilage is a remnant of the hyaline cartilage that, between gestational weeks 6 and 8, became the long bones via endochondral ossification.
Blood Supply and Lymphatics
Every joint in the body has a different blood supply; however, there are patterns based on the histological classification of joints.
Perforating branches of the proximal vessels usually supply fibrous joints. For example, the tibiofibular joint's blood supply is from branches from the anterior tibial artery as well as the peroneal artery.
Cartilaginous joints only receive vascular supply at the periphery because cartilage itself is an avascular tissue. Intervertebral discs, for example, are supplied at the margins by capillaries from the vertebral bodies.
Synovial joints receive vascular supply through a rich anastomosis of arteries extending from either side of the joint, termed the periarticular plexus. Some vessels penetrate the fibrous capsule to form a rich plexus deeper in the synovial membrane. This deeper plexus, termed circulus vasculosus, forms a loop around the articular margins that supplies the articular capsule, synovial membrane, and terminal bone. The articular cartilage, which is avascular hyaline cartilage, is nourished by the synovial fluid.
Lymphatic vessels for every joint follow the lymph drainage of the surrounding tissue—some joints house lymph nodes, like the popliteal lymph nodes in the popliteal fossa of the knee.
Nerves
Every joint in the body has different innervation; however, innervation of synovial joints is most extensively understood.
Sensory and autonomic fibers innervate synovial joints. The autonomic nerves are vasomotor in function, controlling the dilation or constriction of blood vessels. The sensory nerves of the articular capsule and ligaments (articular nerves) provide proprioceptive feedback from Ruffini endings and Pacinian corpuscles. Proprioception of the joint permits reflex control of posture, locomotion, and movement. Free nerve endings convey pain sensation that is diffuse and poorly localized. The articular cartilage has no nerve supply.
Two general principles apply to synovial joint innervation: Hilton’s law and Gardner’s observation. Hilton’s law states that the articular nerves supplying a joint are branches of the nerves that supply the muscles responsible for moving that joint. Therefore, irritation of articular nerves causes a reflex spasm of the muscles which position the joint for the greatest comfort. These nerves also supply the overlying skin, providing a mechanism for referred pain from joint to skin. Gardner’s observation indicates that the part of the articular capsule that is tightened by contraction of a group of muscles receives nerve supply from the same nerves that innervate the antagonist muscles. This relationship provides local reflex arcs that stabilize the joint.
Muscles
Muscles are most critical in providing additional support for synovial joints. The muscles and their tendons, which cross a joint resist the forces acting on that joint, behaving as a dynamic "ligament." Muscle strength is, therefore, essential to the stability of synovial joints, especially during high-stress activity, as well as for joints with weaker ligaments, for example, the glenohumeral.
Surgical Considerations
The surgical replacement of joints is possible using an operation called an arthroplasty; this procedure treats chronic pain and limited mobility associated with osteoarthritis. Arthroplasty is an invasive procedure, so it is the last line of treatment. The operation removes the damaged bone and replaces the articular surfaces with an artificial metal, plastic, or ceramic device built to mimic the natural structure of the joint (prostheses). Hips and knees are the most commonly replaced joints.
Clinical Significance
Different pathology is associated with different joint types. Below is a review of the most common injuries that plague each histological class.
Fibrous
Sutures, the immobile fibrous joints that bind the bony plates of the skull, can fuse too early in development, a condition termed craniosynostosis. The plates of a newborn’s skull are not fused to permit space for the brain to grow in all planes; therefore, early fusion (synostosis) alters the shape of the head. For example, if the sagittal suture synostoses, the head will not develop width and will instead grow long and narrow (scaphocephaly). In addition to altered head shape, some children may experience symptoms that are secondary to high pressure on the brain due to more confined skull space. These include headaches, developmental delays, or problems with eyesight.
A syndesmosis joint, the slightly mobile fibrous joint that connects long bones with an interosseous membrane, can be sprained. For example, in the leg, excessive external rotation can push the fibula away from the tibia, causing injury to the distal tibiofibular syndesmosis; this is termed a “high ankle sprain.”
Cartilaginous
Epiphyseal plates, an example of temporary synchondroses, are vulnerable to damage when there is an injury to the associated growing long bone. Such damage to the cartilage would stop bone lengthening and stunt bone growth.
Synovial
Arthritis is inflammation of the synovial joint. There are many types of arthritis, distinguished by different mechanisms of injury. The most common type of arthritis is osteoarthritis, which, by definition, is gradual damage to and subsequent thinning of the articular cartilage. This condition is considered a “wear and tear” injury and presents in older patients; it often correlates with prior injury to the joint and longstanding high-impact stress on the joint (due to sports or excessive body weight). Because the articular cartilage has no innervation, the degradation itself does not cause pain. Instead, as the articular cartilage becomes thinner, more pressure is placed on the bones. The joint responds by overproducing synovial fluid, which leads to swelling and inflammation, that stretches the highly innervated articular capsule to cause pain and stiffness of the joint. The underlying bone also has a rich nerve supply that perceives pain.
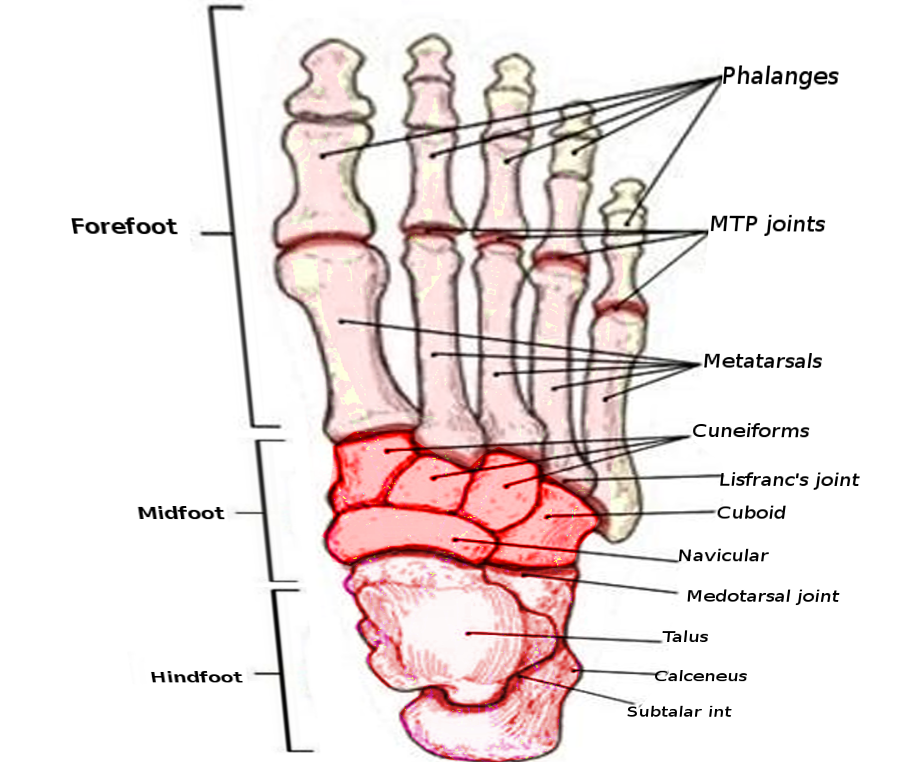
Gout is another form of arthritis caused by the deposition of uric acid crystals within a joint. Uric acid causes gout when there is an excessive amount in the body; this is either due to over-production or improper excretion by the kidneys. The most commonly affected joint is the metatarsophalangeal (MTP) joint of the big toe. Patients often present with excruciating pain and swelling.
Synovitis is inflammation of the synovial membrane that lines the articular capsule of synovial joints. The most common cause is the overuse of a synovial joint in an active, healthy person. Persistent synovitis in multiple joints can indicate rheumatoid arthritis, where the synovium is the target of the autoimmune attack. Patients with synovitis often present with pain out of proportion to examination; in fact, sometimes the patient has pain without swelling or tenderness, or arthralgia.
(Click Image to Enlarge)
(Click Image to Enlarge)