
Temporal Fracture
- Article Author:
- Avik Patel
- Article Author:
- Daniel Lofgren
- Article Editor:
- Matthew Varacallo
- Updated:
- 8/10/2020 9:36:16 PM
- For CME on this topic:
- Temporal Fracture CME
- PubMed Link:
- Temporal Fracture
Introduction
The temporal bone is he thickest bone in the body, and requires great force to fracture (1875 pounds of lateral force in one study). The temporal bone houses portions of the internal carotid artery and internal jugular vein, cranial nerves (CN) VII-XI, the middle and inner ear structures, and forms a portion of the middle cranial fossa. Such high-velocity injury to these crucial structures carris the risk of significant morbidity and mortality.
The temporal bone is a paired component of the skull base, articulating posteriorly with the occipital bone, superiorly with the parietal bones, and anteriorly with the sphenoid bone creating the occipitomastoid, squamous and sphenosquamosal sutures, respectively. The temporal bone has complex anatomy including four geographic parts (squamous, mastoid, petrous, tympanic) and numerous named foramen/canals (foramen lacerum, carotid canal, internal acoustic meatus, jugular foramen).
- Foramen lacerum: greater petrosal nerve
- Carotid canal: internal carotid artery
- Internal acoustic meatus: CN VII, CN VIII
- Jugular foramen: internal jugular vein, posterior meningeal artery, CN IX, CN X, CN XI
Additionally, there are 3 bony processes (zygomatic, mastoid, styloid).
The otic capsule, or bony labyrinth, is the dense portion of the petrous temporal bone that surrounds the membranous labyrinth of the inner ear. This is, in turn, surrounded by the less dense and variably pneumatized petrous apex and the mastoid segment of the temporal bone. From anterior to posterior the otic capsule contains the cochlea, vestibule, and three semicircular canals.
Etiology
Temporal bone fractures are caused by a significant lateral force to the cranium. Approximately one-third of temporal bone fractures in the general population result from motor vehicle accidents, assaults, and falls and an additional ~25% are attributed to sports injuries, gunshot wounds, bicycle accidents, and other miscellaneous causes.
Epidemiology
Pathophysiology
The temporal bones are the thickest skull base components. Dynamic loading studies have yielded a minimum lateral impact force of 6000 to 8000 Newton (N) necessary to cause a fracture.[3] The course of the fracture will be determined by the path of least resistance relative to the direction of the inciting force, more frequently involving the pneumatized portions of the bone as opposed to the denser petrous portion.
History and Physical
Any history of significant trauma to the head, especially with associated loss of consciousness, should elicit suspicion for cranial bone fractures. On physical examination, patients with temporal bone fractures may present with hemorrhagic or clear otorrhea, hemotympanum, vertigo, nystagmus, facial paralysis, conductive or sensorineural hearing loss, ear canal laceration, or Battle’s sign (bruising over the mastoid process).[4][2] Patients may present with altered mental status or abnormal Glasgow coma scale (GCS) scores secondary to concomitant acute intracranial pathology.
Evaluation
Imaging plays a crucial role in the evaluation and management of temporal bone fractures. Computed tomography (CT) has a significantly higher sensitivity for temporal bone fractures than a physical examination.[5] There is a significant association with intracranial injury, and the temporal bone fracture may be first identified on a standard head CT. If a temporal bone fracture is identified, a non-contrast, high-resolution CT with less than 1.5-mm slice thickness and coronal/sagittal reconstructions is recommended to best characterize the fracture. In addition to the evaluation of the skull, CT will demonstrate associated subdural/epidural hematoma, cerebral contusion and/or hemorrhage, subarachnoid hemorrhage and pneumocephalus. Trauma to the head necessitates the evaluation of the cervical spine, often with plain film X-rays. CT angiography should be obtained if the fracture involves the foramina of the internal carotid artery or internal jugular vein. If a cerebrospinal fluid (CSF) leak is suspected due to clear otorrhea, this can be confirmed by testing the fluid for beta-2-transferrin, and the location of the defect can be characterized further via cisternogram.
Once the patient is stable, an MRI can be obtained for patients who suffer cranial nerve palsy not explained by CT findings. MRI can help differentiate between a fluid-filled mastoid and a mastoid containing herniated intracranial contents. MRI may also reveal intracranial pathology not previously diagnosed on CT.[5]
The first classification system for temporal bone fracture described two types relative to the long axis of the petrous ridge: fractures that course parallel are considered "longitudinal" and fractures that course perpendicular are considered "transverse." Longitudinal fractures made up approximately 70-90% of all temporal bone fractures compared with transverse (10-30%), though in reality, it is rare to find a pure example of either, with most fractures taking a somewhat oblique course.[2] A more clinically relevant classification describes fractures relative to the otic capsule involvement. Fractures are either otic capsule sparing or otic capsule violating. Otic capsule sparing fractures generally involve the squamosal temporal bone and external auditory canal, starting from mastoid air cells to the middle ear to the tegmen tympani. These generally have lower rates of CN VII paralysis but tend to have higher rates of mixed or conductive hearing loss due to hemotympanum or (more rarely) ossicular chain disruption. Temporal bone fractures that violate the otic capsule have a much higher association with CSF leak, sensorineural hearing loss (SNHL), and certain intracranial pathology.[6] These fractures generally pass through foramen magnum to the petrous pyramid and then the capsule, and are generally from a blow to the occipital region. They almost always induce SNHL and rarely affect the ossicular chain or external auditory canal.
Further workup includes audiometric testing for any hearing loss, vestibular testing for vertigo or nystagmus, and nerve conduction studies for facial nerve paresis or paralysis. Historically the minimal nerve excitability test or maximal stimulation test was used for evaluation of the facial nerve, these have been supplanted by more precise testing and are mentioned for completeness purposes only. If there is an immediate, complete facial nerve paralysis in the setting of a temporal bone fracture, emergent surgical exploration is warranted. If there is a new facial paresis in the setting of a temporal bone fracture, further nerve function testing is indicated. The modern standard battery of tests is a combination of electroneuronography (EnOG) and electromyography (EMG). EnOG provides a qualitative measurement of nerve stimulation by comparing function to that of the contralateral side and can be performed serially to determine if a facial nerve injury is progressing.[7][8] Loss of 90% of function on EnOG is also an indication for surgical exploration and decompression of the nerve. EMG assess action potentials in facial muscle movement and can be performed when voluntary movement is not present. Denervated muscle will display fibrillation potentials, while re-innervating muscle will demonstrate polyphasic potentials. Both of these tests are the most useful 10-14 days out of injury to allow time for Wallerian degeneration to occur if a facial nerve injury is present.[9]
Treatment / Management
Treatment and management of associated life-threatening, intracranial pathology should be the primary focus. The management of temporal bone fracture complications should be addressed once the patient is stable.
Facial Nerve Paralysis
Immediate paralysis and/or significant degeneration (>90%) on EnOG are indications for surgical exploration and decompression. Findings in such surgery most often demonstrate bony impingement of the nerve, stretch injury, or edema/hematoma rather than transection of the nerve.[10]elayed onset paralysis usually indicates the development of neural edema or compression by hematoma which can be treated with a 1- to 3-week course of corticosteroids in most cases; serial EnOG should be performed and surgery considered if degeneration reaches or exceeds 90%.[11]
CSF Leak
Conservative management including elevation of the head, bed rest, avoidance of straining should be instituted. Antibiotic prophylaxis to avoid the development of meningitis is somewhat controversial, though nearly always employed in the setting of ongoing CSF leak.[12] Should conservative measures be unsuccessful, a lumbar drain is placed to decrease intracranial pressure. A small minority of patients will require surgical repair.
Hearing Loss
Early evaluation is only able to identify conductive versus sensorineural loss. Formal audiological evaluation is deferred several weeks post-injury to ensure edema and hemotympanum have completely resolved. Persistent conductive hearing loss is an indication for surgical exploration with ossiculoplasty. Persistent sensorineural hearing loss can be treated with hearing aids or cochlear implant, depending on severity.
Vertigo
Vestibular function testing should be performed on an elective, outpatient basis once the patient has returned to their neurological baseline. In cases of perilymph fistula, surgical repair is warranted. Post-traumatic perilymphatic hydrops should be managed with corticosteroids and diuretics.[1]
Differential Diagnosis
- Conductive hearing loss
- Cranial nerve palsies
- CSF leak
- External auditory canal stenosis
- Facial paralysis
- Internal carotid artery dissection and thrombus
- Meningitis
- Meningocele
- Sensorineural hearing loss
- Vertigo
Prognosis
Overall the patient prognosis depends on intracranial involvement. The prognoses of common temporal bone fracture complications are as follows:
- Facial nerve paralysis: Partial and/or delayed facial paralysis has an overall favorable prognosis with conservative treatment only. Complete paralysis carries a much more guarded prognosis, with ~50% of such patients regaining near-normal facial nerve function.
- CSF leak: The majority of CSF leaks will resolve within two weeks with only conservative measures. Surgical repair of the leak is possible in refractory cases.
- Hearing loss: Hearing loss is most commonly conductive in nature, and due to hemotympanum. Complete recovery is expected. If ossicular chain disruption is present this can be surgically repaired with excellent results. Recovery of sensorineural hearing loss is much more variable, and treatment can include amplification or cochlear implant, depending on the severity.
- Vertigo: Vertigo may improve within several months post-injury, participation in physiotherapy or a more formal neuro-rehabilitation program can improve long-term outcomes.
- Meningitis: Generally resolves with appropriate antibiotic treatment.
Complications
- Facial paralysis: CN VII damage
- Sensorineural hearing loss: CN VIII damage
- Conductive hearing loss: Ossicle/tympanic membrane disruption, hemotympanum
- Vertigo: CN VIII damage, perilymphatic fistula, post-traumatic perilymphatic hydrops, cerebral injury
- CSF leak
- Meningitis
- Cranial nerve palsies: CN IX, X, XI
- Internal carotid artery dissection and/or thrombus
- Meningocele
- External Auditory Canal Stenosis
Consultations
Successful treatment and management of patients suffering from temporal bone fractures require an interprofessional effort. Trauma surgery, neurosurgery, otolaryngology, and neurotology should be consulted. As in all trauma cases, one must follow the ABCD protocol and consult with the relevant specialists depending on the pathology found on imaging studies. The outcomes for most patients without intracranial injury is good, but those with intracranial pathology have a guarded prognosis. Some patients may have residual neurological deficits that may persist for a long time, with some sequela reducing patients' quality of life.
Pearls and Other Issues
- Temporal bones require an immense amount of lateral force to fracture.
- Look for hemorrhagic or clear otorrhea, hemotympanum, hearing loss, vertigo, nystagmus, facial paralysis, and/or Battle’s sign.
- Fractures should be classified as either otic capsule sparing or violating, with violation being more likely to cause SNHL, perilymphatic fistula, facial nerve paralysis, and requiring surgery.
- High-resolution non-contrast CT with slice thickness less than or equal to 1.5 mm is the modality of choice.
- Look for associated intracranial and cervical pathology.
- Once stabilized, temporal bone fracture complications can be treated.
- Complications include facial nerve paralysis, CSF leak, hearing loss, vertigo.
- Hearing loss requires immediate characterization of conductive versus sensorineural hearing loss, with formal audiogram deferred to allow for resolution of hemotympanum or edema.
- Facial nerve paralysis workup should include an EnOG and EMG if paralysis is evolving, and surgical exploration if it is immediate.
- CSF fistulas usually resolve spontaneously but may require lumbar drainage or surgical repair if persistent.
Enhancing Healthcare Team Outcomes
Upon presentation, suspicion for intracranial pathology should be high. The patient should be stabilized before undergoing a detailed temporal bone evaluation. Understanding the anatomical relationships of the temporal bone is necessary for anticipating potential complications. Treatment and management of temporal bone fractures are complex and require an interprofessional approach. Radiologists are tasked with timely identification and classification of temporal bone fractures and communication of findings to surgery and medical teams. The surgery teams should decide when and if intervention is necessary. Nursing staff plays a key role in monitoring the status of the patient throughout their hospitalization. The management of complications requires routine follow-up and, sometimes, additional outpatient testing.
(Click Image to Enlarge)
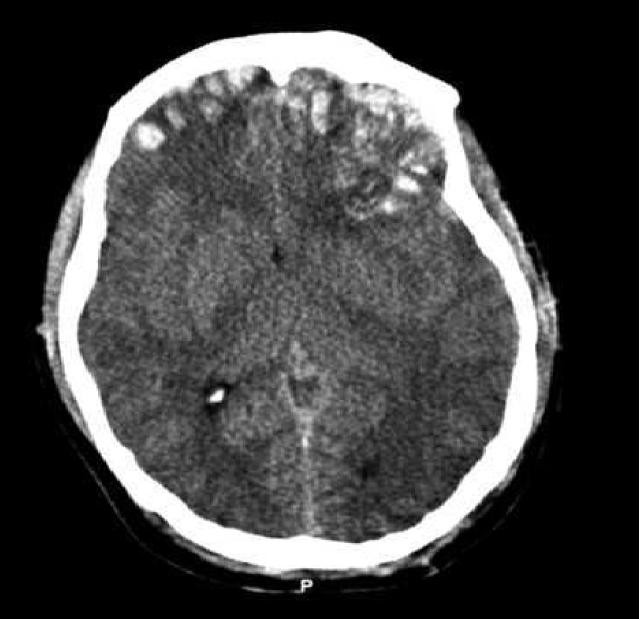
CT scan of patient with brain trauma. Caption reads, "Preoperative CT scan of patient while he had a GCS of 14." Accompanying text in article reads, "Emergent CT imaging revealed a sagittally oriented skull fracture extending from the vertex to the foramen magnum as well as a transverse parietal and temporal bone fracture. Multiple frontal, parietal, and temporal lobe contusions with associated interhemispheric hemorrhage and a left-sided subdural hematoma measuring 1.7 mm in greatest depth were appreciated. Effacement of the basilar cisterns was noted without shift of midline structures."
Contributed by Wikimedia Commons, Rehman T, Ali R, Tawil I, Yonas H (CC by 2.0) https://creativecommons.org/licenses/by/2.0/deed.es
