Anatomy, Tendons
- Article Author:
- Bruno Bordoni
- Article Editor:
- Matthew Varacallo
- Updated:
- 7/31/2020 3:58:01 PM
- For CME on this topic:
- Anatomy, Tendons CME
- PubMed Link:
- Anatomy, Tendons
Introduction
The tendon is a "mechanical bridge." It allows the transmission of muscle strength to the bones and joints, on the other it allows the contraction of the muscle to make the final tangible movement. There are different types of tendons which reflect the morphology of the muscle and their specific function. Tendon tissue is not just about the terminal or initial area of each muscle but involves the entire muscular tissue. The connective layers (epimysium, perimysium, and endomysium) merge into a single organization to make contact with one or more fixed bone points. The same tendon near the muscle has contractile fibers. The muscle affects the tendon, and the tendon affects the functional expression of the muscle. In the context of manual therapy, rehabilitation, or surgery, it is a mistake not to consider these close relationships of anatomy and function. The tendon tissue can adapt its cellular structure under physiological (training) or pathological (trauma) stimuli, depending on the systemic hormonal environment and age.[1][2]
Structure and Function
The tendon plays an extraordinary role in mechanics and movement. They transmit the force produced by the muscular contraction to the skeletal levers, thus allowing the movement and the maintenance of the body posture. The tendons allow the muscle to be at an optimal distance from the joint on which it acts without requiring an excessive length of the muscle between the origin and the insertion. Tendons are stiffer than muscles, have greater tensile strength and can withstand very large loads with minimal deformations. This property of the tendons makes the muscles capable of transmitting forces to the bones without losing energy to stretch the tendons. For example, the flexor tendons of the foot can bear more than 8 times the body weight and store about 40% of this weight for an elastic hysteresis during the walk.[3][4][5][6]
Tendon Sheaths
The tendons have satellite structures whose main task is to facilitate the sliding of the tendon tissue surrounding anatomical structures and prevent the tendon from losing its course of action during muscle contraction.
Fibrous Sheaths
The fibrous sheaths or retinaculas represent the sliding channels of the tendons, in particular, the long ones. This sliding on the neighboring tissues could be considerably compromised by the friction developed especially at bone structures. In these regions, there are tunnels in which the tendons flow surrounded by a synovial sheath. In particular, the showers and bone incisions are generally covered by a fibrocartilaginous floor on which a fibrous fabric roof passes over a bridge. This represents the fibrous or retinacellar sheath, a formation that is found at the extremities. Typical examples are the retinaculae of the flexor and extensor tendons of the hand and foot at the level of the wrist and the instep.
Synovial Sheaths
The synovial sheaths facilitate sliding of the tendon inside the fibrous sheath. They consist of 2 thin serous sheets: the parietal sheet that covers the walls of the fibrous sheath and the visceral leaf that covers the surface of the tendon. The 2 sheets continue at the level of the 2 ends of the duct. The closed space delimited by the 2 sheets contains a thin veil of liquid, the peritendinous liquid, which has roughly the same composition of the synovial fluid. It mainly has a lubricating function. Peduncles of loose tissue detach themselves from the walls of the osteo-fibrous canals and terminate on the tendinous belly leading to the tendon vessels and nerves. These structures constitute the mesotenonium and are also covered by the synovial and may be more or less numerous depending on the length of the tendon itself. However, not all tendons possess true synovial sheaths; these are in fact found only in areas where a sudden change in direction and an increase in friction require very efficient lubrication.
Peritendon Sheaths (Paratenon)
The peritendinous sheets have a function that can be superimposed on that of the synovial sheaths, although they present a different histological structure. Paratenon is made up of collagen fibrils of type I and III and of thin elastic fibers. It helps to reduce friction and works as a sort of elastic sleeve that allows the free movement of the tendon with respect to the surrounding structures.
Reflection Pulleys
They are circumscribed thickenings of dense fibrillar tissue located along the course of the fibrous sheaths. They contain the tendon inside the sliding bed, especially where there are curvatures along the course of the tendon.
Tendon Bursae
Tendon bursae help to minimize friction between the tendon and adjacent bone structures. These are small serous vesicles, located in the sites where a bony prominence can compress and then wear out the tendon; typical examples are subacromial, infrapatellar, and retrocalcaneal bursae.
Below the paratenon, the entire tendon is surrounded by a thin sheath of dense connective tissue called epitenonium. Together, these can be called peritenonium. Within the epitenonium the collagen fibrils are differently oriented, being disposed transversely as well as longitudinally and obliquely. Occasionally the epitenonium fibrils appear to be fused with the superficial tendon fibrils. On its external surface the epitenonium is contiguous to the peritenonium, and on the inner surface, it is instead in continuity with the endotenonium, a thin membrane of loose connective tissue that covers the individual tendon fibers and groups them in larger units represented by bundles of fibers of various order. The function of endotenonium is to circumscribe, individualizing, the various orders of bundles and to allow the penetration and the capillary distribution of vasculonervous structures inside the tendon.
The point where the muscle pierces in the tendon is called muscle-tendon junction, while the point where the tendon inserts on the bone is called osteo-tendinous junction.
Cells
Two different types of specialized fibroblasts co-exist in the tendon tissue: tenocytes and tenoblasts.
The tenocytes have an elongated shape, while the tenoblasts have an ovoid shape. In the tendon healing phase, the tenoblasts are more involved in the tissue repair process, depositing collagen fibers. Finally, in the last repair phase, the tenoblasts are transformed into tenocytes.
Tenoblasts represent approximately 90% to 95% of the tendon fibroblasts. In the compression areas we can find endothelial cells and chondrocytes.
These specialized fibroblasts produce extracellular matrix, such as collagen, proteoglycans, and other proteins. Collagen accounts for the largest share (about 65% to 80%). The prevalent collagen in the tendons is that of type I, next to minor proportions of type III collagen, present in the epitenonium and in the endotenonium and of type II, identifiable in the fibrocartilaginous areas of the osteo-tendinous junction. Instead, elastin, proteoglycans and glycoproteins constitute 4%, 4%, and 2%, respectively, of the matrix.
In the tendon, the collagen fibers are made up of a variable number of fibrils arranged in pallel with each other and joined together in fibers, always in parallel to each other and the tendon axis. The bundles of collagen fibers show a wavy pattern, with periodic changes of direction, known in the literature as crimps. In the same tendon, the crimps differ in size and geometry, appearing as isosceles or scalene triangles of variable size. The single crimp, observed by scanning electron microscope, appears to consist of rectilinear fibrillary segments tightly packed together joined by nodes or hinges, in correspondence of which all the fibrils of each fascicle change simultaneously direction. In changing their course, the fibrils do not describe a loop but are deformed as a hollow cylindrical structure would do. Collagen bends but does not break.
Mechanical Properties
The biomechanical behavior of a tendon is related not only to the magnitude of tension stress but also to the shape of the tendon itself. Muscles used to perform delicate and precise movements, such as the flexors of the fingers, possess long and thin tendons, while those that perform actions of power and endurance, such as the quadriceps femoris and the triceps sural, have shorter and more robust tendons. A short tendon has a greater tensile strength than a long tendon because the load required to produce the break is much larger in the short tendon with the same diameter.
A long tendon can undergo a greater deformation than that of a short tendon before going to rupture. Strength and resistance of a tendon are therefore 2 different entities and depend on the diameter and length of the tendon itself. The biomechanical properties of the tendon are related to the diameter and arrangement of collagen fibrils; tendons subjected to high stress are fibrils of a large diameter, less flexible than those of small caliber.
The ability of the tendons to amortize and transmit the force of muscle contraction is also closely related to the tendon crimp. Researchers observe that the greater load a tendon is subjected to, the greater the angle at the base of the crimps. When the tendon is stretched, the crimps gradually tend to become flat. They act as a shock absorber in the tendon during the early stages of pulling, and allow the tendon to recover the form at the cessation of the applied force. The crimps do not disappear simultaneously (flat), but gradually, from the periphery to the center.
The same biochemical and cellular structure of the tendon contribute to the mechanical function of the tissue: the different components of the extracellular matrix; the interactions between fibrils and proteoglycans (PGs) and those between the glycosaminoglycan chains (GAGs); glycoproteins.
Adaptation to Mechanical Stress
There is a difference between a man and a woman. After a training that undergoes the tendon to mechanical stress, the female has less tendon strength than the male. Women have a greater tendon lengthening; this could explain why men are more susceptible to tendon inflammation.
The tendon tissue adapts itself to the mechanical environment that surrounds it. In the presence of mechanical tension (contraction and muscle release), the tendon increases its diameter, thanks to an increase in the synthesis of collagen. Adaptation is specular to the imposed stress. Finally, it increases the stiffness and the Young's modulus. The latter defines the relationship between mechanical stress (force per unit area) and strain (deformation).
Adaptation to Age
The tendon of older people is less adaptable. If in a young person, the tension of the Achilles tendon is within the basic values after 1 hour, in the elderly subjects there is a loss of tension for more time. In an older person's tendon, there is an alteration of the cellular structure (less anisotropy), with a diminished response to the regenerative capacity. The tendon is less able to adequately pilot the force expressed by the muscle toward the bone tissue. Collagen fibers are less organized; calcification phenomena can occur; there is a lower number of fibroblasts and senescent cells and a decrease in the amount of water and the number of proteoglycans, with reduced viscoelastic properties.
The tendon is weakened and becomes more susceptible to trauma.
The decrease of estrogen in women makes the tendon tissue looser (there are estrogenic receptors on the tendon). This metabolic event would make the tendon more prone to trauma and inflammation.
Embryology
The tendon is derived from the ectoderm (such as ligaments). Progenitor cells of the tendon (tenocytes) originate from the ventral and lateral ectodermal area. In the cranial and limb region (animal model) the tendon is formed in the absence of the muscle; subsequently, the contractile tissue will be indispensable for their maintenance. The axial tendons, on the contrary, require the presence of the muscle to induce the movement of the progenitor cells of the tendon, through the action of FGF (fibroblast growth factor). Usually, the progression of cartilage and muscle tissue in the development period occurs more quickly, compared to the tendon.
Blood Supply and Lymphatics
The blood circulation of the tendon is ensured, in small part, by the vessels coming from the muscular belly and the periosteum surrounding the osteotendinous junction and, for the rest, from the vascular network of the peritendinous sheets and the synovial sheath, in the sites where this is present. The circulatory network of peritendinous leaflets has a very variable structure, both in the different tendons and in different areas of the same tendon. In some cases, in fact, the primary trunks are arranged to form a rather regular mesh structure; in other cases, they form concentric arches and are arranged in a completely irregular manner. The vascular network consists of small and medium-caliber arteries, each of which is accompanied by one or two satellite veins extensively anastomosed to each other. Based on the characteristics of the capillaries, 3 types of microvascular units can be distinguished. In one type, the capillary travels a long distance with a direction parallel to the longitudinal axis of the tendon, then becomes recurrent, describes a loop and flows into a venule; generally, a single arteriole gives rise to several capillary loops that run in different planes in the context of the tendon. Another type of microvascular unit, less specialized than the previous one, presents capillaries with an irregular course. Another type is characterized by very short capillaries with a straight course that acts as arterio-venous shunts. The presence of multiple microvascular units would facilitate the diffusion of gases and metabolites within individual tendon bundles.
Lymphatic drainage affects the connective tissue sheath of the tendon, forming a network. The lymphatic contents will go towards the tendon veins or to other neighboring venous structures
When the tendon is subjected to mechanical stress, the flow of blood that reaches the tendon tissue increases. Lymphatic drainage under stress does not increase.
Nerves
Tendons are innervated by nerve branches coming from both the muscular belly and from the sensitive branches that are distributed to the skin. The innervation is localized in the paratenon, endotenon, and epitenon.
In the context of the tendon, the nervous branches, which are relatively scarce, form trunks with a course parallel to the major axis of the tendon itself, anastomosed from branches with a transverse and oblique course. The nerve endings of these branches are of various types: some end in muscle-tendinous organs of the Golgi, in corpuscles of Pacini, or Ruffini; others are resolved in free arborizations. The blood branches accompany the nerve branches.
The sympathetic innervation of the tendon is found in the vicinity of the perivascular areas. At the peritendinous level, sensory nerve fibers can be found, similar to parasympathetic fibers. Generally, in a healthy tendon, the orthosympathetic fibers stimulate the vasoconstriction, the parasympathetic fibers allow vasodilation. Finally, there are small-diameter sensory fibers, which can stimulate vasodilation.
Muscles
The tendon adapts to the morphology of the muscle. A flat muscle will have a flattened tendon or aponeurosis, while a muscle with a larger diameter will have a cordiform tendon. Tendon health allows the muscle to function properly and to better adapt to the functions that compete with it. Moreover, a healthy tendon allows an optimal mechanotransduction mechanism to the contractile fibers, with a better performance.
Physiologic Variants
Literature shows many anatomical variations of the tendon. For example, the tendon of the long head of the biceps may vary its shape, its origin, or be absent with a 1.9% to 7.4% match rate in the population. The popliteal muscle tendon can have a bifurcation of 0.4%, thus creating 2 muscular bellies. The tendon of the flexor-longus hallux muscle has a lease and shape variability of approximately 9.8%. The patellar tendon, a passive patella stabilizer, may present as 2 distinct tendons or be absent.
Surgical Considerations
The decision of whether or not to proceed with surgical intervention, as opposed to nonoperative management, is based on a multitude of factors. A review of specific tendon injury management is beyond the scope of this review. However, the general principles that are considered when performing a thorough clinical analysis of managing patients with various types of tendon injuries include:
- Partial versus complete injuries or rupture
- Region of the body affected
- Capacity to compensate (i.e. clinical significance and functional outcome in the setting of tendon injury)
- Age of patient, functional goals (i.e. sedentary versus active or sport-specific lifestyle)
- Patient medical comorbidities (diabetes, inflammatory arthropathies, systemic conditions)
- Hand dominance
- Cosmetic deformity (i.e. proximal biceps, "popeye" deformity)
- Chronicity of injury, tissue quality (important when determining if direct repair can be considered versus allograft or autograft tendon reconstruction)
- Available surgical alternatives (tendon transfer principles)
- Social factors (patient compliance, smoking status, history of IV drug abuse)
- Current medications (chronic steroid use, certain antibiotics, such as fluroquinolones)
Clinical Significance
Tendinopathy results in vascular changes and adaptations to the macroscopic and microscopic environment of the muscle and tendon. One of the causes of increased vascularization (hypertrophy and hyperplasia) is the presence of an angiogenic cytokine (vascular endothelial growth factor [VEGF]), which increases in inflammatory environments. The increase in blood flow decreases the strength of the tendon with a reduction in the sliding capacity of the different connective layers. The same increase in nerve fibers occurs superficially in the tendon, and toward the inside; nociceptive fibers also increase, causing pain.[7][8][9][10]
There is an increase in sympathetic nerve fibers near the blood vessels. It is hypothesized that altered tenocytes can synthesize nociceptive neurotransmitters, which will then be recorded by the sympathetic system, with the onset of pain.
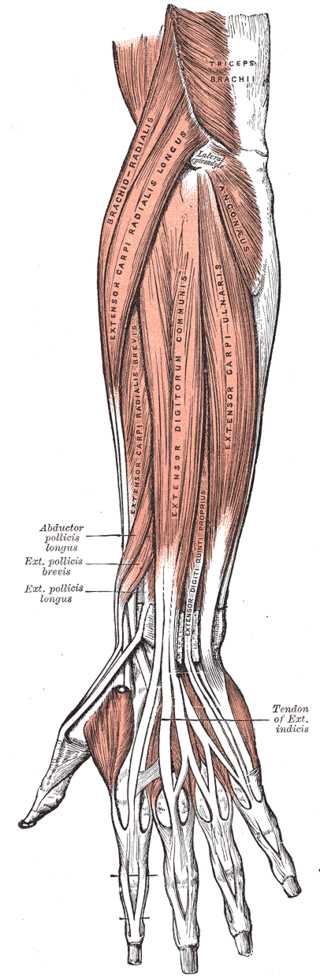
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)

Ligaments of the sole of the foot, Plantar Intermetatarsal Ligament, Plantar Calcaneocuboid Ligament, Tendon Peroneus Longus, Long Plantar Ligament, Tendon Peroneus Longus, Plantar Tarsometatarsal Ligament, Tendon Tibialis Anticus, Plantar Cuneonavicular Ligament, Plantar Calcaneonavicular Ligament, Tendon Tibialis Posticus,
Contributed by Gray's Anatomy Plates