Anatomy, Head and Neck, Tongue
- Article Author:
- Ary Dotiwala
- Article Editor:
- Navdeep Samra
- Updated:
- 8/22/2020 9:36:24 PM
- For CME on this topic:
- Anatomy, Head and Neck, Tongue CME
- PubMed Link:
- Anatomy, Head and Neck, Tongue
Introduction
The tongue is the muscular organ found in the vertebrate mouth. It is attached via muscles to the hyoid bone, mandible, styloid process, palate, and pharynx and divided into two parts by the V-shaped sulcus terminalis. These two parts, an anterior two thirds and a posterior one third, are structurally and developmentally distinct. The foramen cecum at the apex of the sulcus terminalis indicates the site of embryonic origin of the thyroglossal duct.[1][2][3]
The following papillae cover the tongue and are used for taste perception:
- Vallate papillae are arranged in a V-shape anterior to the sulcus terminalis and studded with numerous taste buds. Innervation is by the glossopharyngeal nerve (CN IX).
- Fungiform papillae are mushroom-shaped papillae with erythematous domes, located on the lateral aspects and at the apex of the tongue.
- Filiform papillae are slim, cone-shaped projections organized in rows parallel to the sulcus terminalis.
- Foliate papillae are rarely found in humans (vestigial).
Another important part of the tongue is the lingual tonsil, a collection of nodular lymphatic tissue towards the posterior one-third of the dorsum of the tongue.
Structure and Function
The functions of the tongue include taste, speech, and food manipulation in the oral cavity.
Taste Functions
Chemicals that interact with the taste buds in the tongue are referred to as "tastants." Taste buds themselves are found within the various papillae of the tongue. Tastants interact with gustatory cell receptors in the taste buds, resulting in transduction of a taste sensation. The five broad categories of taste receptors are (1) sweet, (2) salty, (3) sour, (4) bitter, and (5) umami. The lingual papillae are divided into the vallate (or circumvallate), fungiform, filiform, and foliate papillae. More than half of the taste buds are located on the vallate papillae at the junction of the oral and oropharyngeal tongue or tongue base.
Speech Functions
Speech is produced in part by manipulation of the tongue in the mouth against the teeth and palate within the oral cavity. The intrinsic muscles of the tongue are involved primarily in shaping the tongue for speech.
Food Manipulation Functions
The tongue moves food around the mouth within the oral cavity by pressing it against the hard palate and out to the sides to enable mastication. It enables the formation of the food bolus in the oral preparatory phase of swallowing. It also takes part in the oral phase of swallowing by elevating and sweeping posteriorly to propel the food bolus past the anterior tonsillar pillar, triggering the swallowing reflex.
Embryology
Tongue development begins in the embryo at approximately four weeks' gestation. Initially, two lateral lingual swellings and one medial swelling, called the tuberculum impar, form from the first pharyngeal arch. A second median swelling, known as the copula or hypobranchial eminence, develops from the mesoderm of the second, third, and fourth pharyngeal arches. A final third median swelling forms from the posterior portion of the fourth arch and develops into the epiglottis. Directly posterior to this swelling is the laryngeal orifice, which is accompanied on either side by the arytenoid swellings.
The lateral lingual swellings increase in size, eventually merging and overlapping the tuberculum impar. The merger of these two swellings forms the anterior two-thirds of the tongue. The mucosa overlying this part of the tongue originates from the first arch; thus, the sensory innervation to this area is from the mandibular branch of the trigeminal nerve (CN V3). Meanwhile, the second, third, and fourth portions of the pharyngeal arch, which make up the copula, develop into the posterior one-third of the tongue. The mucosa overlying this part of the tongue has sensory innervation from the glossopharyngeal nerve (CN XI), which is a sign that the third arch overlaps that of the second. The third arch derivatives typically are associated with glossopharyngeal sensory innervation.
The epiglottis and epiglottic region of the tongue develop from the third median swelling, which arises from the posterior fourth pharyngeal arch. Innervation of this region is by the superior laryngeal nerve, which reflects its development from the fourth pharyngeal arch.
The muscles of the tongue predominantly derive from myoblasts that originate in occipital somites and thus are innervated by the hypoglossal nerve (CN XII).
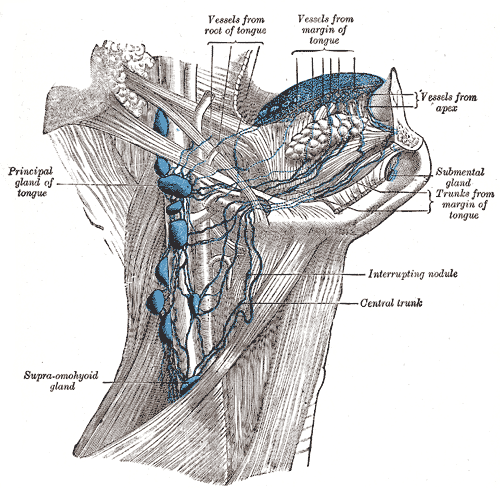
Blood Supply and Lymphatics
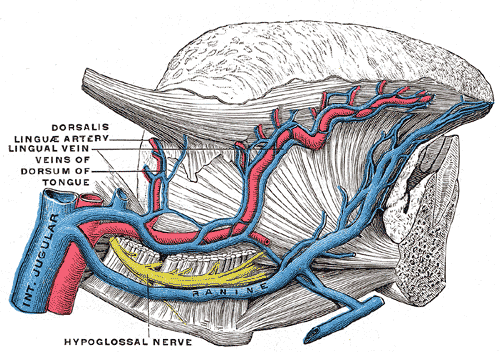
Blood supply to the tongue is predominantly from the lingual artery, a branch of the external carotid artery between the superior thyroid artery and the facial artery, which departs at the level of the greater horn of the hyoid bone within the carotid triangle. After branching from the external carotid artery, the lingual artery passes deep to the hyoglossus muscle and superficial to the middle pharyngeal constrictor muscle. It then gives rise to the following four arteries:
- The suprahyoid artery supplies the omohyoid, sternothyroid, and thyrohyoid muscles. They anastomose with the corresponding vessels from the opposite side.
- The dorsal lingual arteries arise beneath the hyoglossus muscle and pass to the posterior part of the dorsum of the tongue. They supply the mucous membrane of this region as well as the glossopalatine arch, lingual tonsils, soft palate, and epiglottis. They anastomose with their corresponding vessels on the opposite side.
- The sublingual artery branches at the anterior border of the hyoglossus muscle before passing between the genioglossus muscle and mylohyoid muscle to the sublingual gland. It supplies the sublingual gland before giving branches to the mylohyoid muscle. One branch from the sublingual artery passes posterior to the alveolar process of the mandible and anastomoses with the corresponding artery from the other side. A second branch of the sublingual artery pierces the mylohyoid muscle and anastomoses with the submental branch of the facial artery.
- The deep lingual artery, which is the termination of the lingual artery, passes between the genioglossus muscle and inferior longitudinal muscle.
Nerves
The hypoglossal nerve (CN XII) provides motor innervation to all of the intrinsic and extrinsic muscles of the tongue except for the palatoglossus muscle, which is innervated by the vagus nerve (CN X). It runs superficial to the hyoglossus muscle. Lesions of the hypoglossal nerve cause deviation of the tongue to the ipsilateral (i.e., damaged) side.
Taste to the anterior two-thirds of the tongue is achieved through innervation from the chorda tympani nerve, a branch of the facial nerve (CN VII). General sensation to the anterior two-thirds of the tongue is by innervation from the lingual nerve, a branch of the mandibular branch of the trigeminal nerve (CN V3). The lingual nerve is located deep and medial to the hyoglossus muscle and is associated with the submandibular ganglion.
On the other hand, taste to the posterior one-third of the tongue is accomplished through innervation from the glossopharyngeal nerve (CN IX), which also provides general sensation to the posterior one-third of the tongue.
Taste perception also is performed by both the epiglottis and the epiglottic region of the tongue, which receives taste and general sensation from innervation by the internal laryngeal branch of the vagus nerve (CN X). Damage to the vagus nerve (CN X) causes contralateral deviation (i.e., away from the injured side) of the uvula.
Muscles
The tongue's intrinsic muscles include the following:
- The superior longitudinal lingual muscle, which shortens the tongue and curls it upward.
- The inferior longitudinal lingual muscle, which shortens the tongue and curls it downward.
- The transverse lingual muscle, which elongates and narrows the tongue.
- The vertical lingual muscle, which flattens the tongue.
The tongue's extrinsic muscles include the following:
- The genioglossus muscle, which protrudes the tongue, and is innervated by the hypoglossal nerve (CN XII).
- The styloglossus muscle, which draws up the sides of the tongue to create a trough for swallowing following adequate mastication. The pair of styloglossus muscles works together on each side to retract the tongue. The styloglossus muscle is innervated by the hypoglossal nerve (CN XII).
- The hyoglossus muscle, which depresses and retracts the tongue and is innervated by the hypoglossal nerve (CN XII).
- The palatoglossus muscle, which elevates the posterior tongue, closes the oropharyngeal isthmus, aids in the initiation of swallowing, and prevents the spill of saliva from the vestibule into the oropharynx by maintaining the palatoglossal arch. It is the only extrinsic muscle of the tongue that is not innervated by the hypoglossal nerve; instead, it is innervated by the vagus nerve (CN X).
Physiologic Variants
- Ankyloglossia ("tongue-tie") occurs due to an abnormal length of the frenulum linguae which causes limited manipulation of the tongue during speech and results in a speech impediment. In the most common form of ankyloglossia, the frenulum extends to the tip of the tongue. Ankyloglossia can be corrected by surgically severing the lingual frenulum. [4][5]
- Fissured tongue ("scrotal tongue," "plicated tongue") occurs when several small furrows present on the dorsal surface of the tongue. It can be an oral manifestation of psoriasis. It is generally painless and benign, and is often associated with other syndromes (e.g., Down syndrome).[6]
- Geographic tongue ("migratory glossitis") is a benign, asymptomatic condition characterized by the presence of large red patches with a greyish-white border covering the dorsum of an otherwise normal tongue. It is caused by inflammation of the mucous membrane of the tongue, which results in loss of lingual papillae. The lesions are known to migrate over time. The name arises from the map-like appearance of the tongue in this condition.[7][8]
Surgical Considerations
Thyroglossal duct cysts can develop when there is a remnant at the point of embryologic origin of the thyroid gland, the foramen cecum. The thyroid gland begins to develop in the floor of the embryologic pharynx at the point called the foramen cecum, which is located at the dorsum of the posterior tongue. The developing gland then relocates to its ultimate destination in the anterior neck by migrating down the thyroglossal duct anterior to the hyoid cartilage and thyroid cartilage before stopping anterolateral to the superior aspect of the trachea. The thyroglossal duct ordinarily disappears, but remnants of its epithelium may remain, allowing for the potential development of a thyroglossal duct cyst in this area. These cysts generally occur in the neck, close to or inferior to the body of the hyoid bone. They form a swelling at the anterior midline of the neck that is painless, fluctuant, and moves upon swallowing. Thyroglossal ducts cysts typically are removed surgically.[9][10]
Clinical Significance
The tongue tends to fall posteriorly, thus obstructing the airway. Paralysis or total relaxation of the genioglossus muscle presents a risk of suffocation, which can occur during general anesthesia. An artificial airway is made using intubation, which prevents the tongue from falling backward and blocking the airway.
- Ludwig angina infection, once established, evolves to include the tongue. The tongue may enlarge to two or three times its usual size and tends to distend posteriorly into the hypopharynx, superiorly against the palate, and anteriorly out of the oral cavity. Any immediate posterior extension of this process will ultimately involve the epiglottis. The styloglossus muscle creates the connection between the submandibular parapharyngeal spaces, otherwise known as the buccopharyngeal gap, as it leaves the tongue and passes in between the middle and superior constrictor muscles before attaching to the styloid process. Cellulitis of the submandibular space may spread into the pharyngeal space and, from there, into the retropharyngeal space of the mediastinum.
- Dysgeusia, or a pure taste disorder, is rare and is usually associated with olfactory disorders.
(Click Image to Enlarge)
(Click Image to Enlarge)