Neuroanatomy, Cranial Nerve 5 (Trigeminal)
- Article Author:
- Trevor Huff
- Article Editor:
- Daniel Daly
- Updated:
- 7/31/2020 3:18:53 PM
- For CME on this topic:
- Neuroanatomy, Cranial Nerve 5 (Trigeminal) CME
- PubMed Link:
- Neuroanatomy, Cranial Nerve 5 (Trigeminal)
Introduction
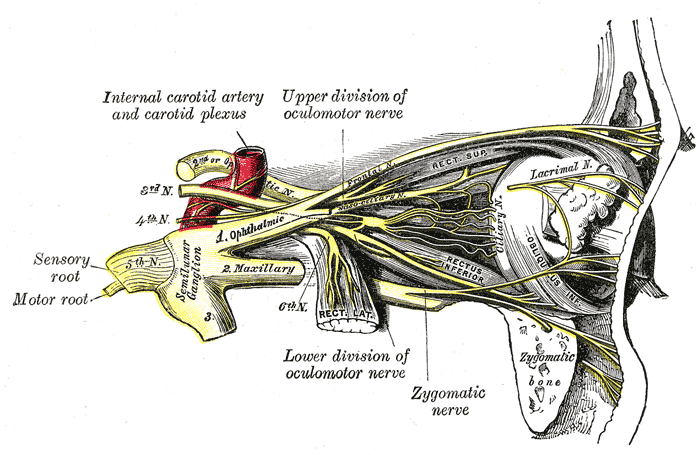
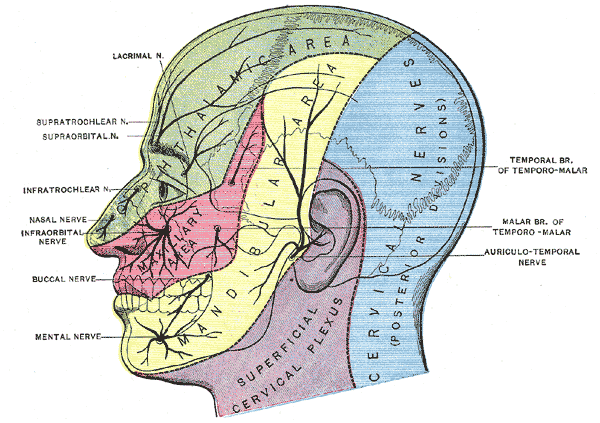
The trigeminal nerve is the fifth cranial nerve (CN V). Its primary function is to provide sensory and motor innervation to the face. The trigeminal nerve consists of three branches on either side that extend to different territories of the face. These branches join at the trigeminal ganglia which are located within the Meckel cave of the cranial cavity. The different branches are namely the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves. The ophthalmic nerve is responsible for sensory innervation of the face and skull above the palpebral fissure as well as the eye and portions of the nasal cavity. The maxillary nerve is also a sensory branch and innervates portions of the nasal cavity, sinuses, maxillary teeth, palate, and the middle portion of the face and skull above the mouth and below the forehead. The mandibular nerve is unique in that it contains both sensory and motor fibers. It provides sensory innervation of the buccal mucosa, mandibular teeth, and the skin below the mouth. The motor portion of V3 innervates all the muscles of mastication. Additionally, V3 provides sensory information from the anterior two-thirds of the tongue; this is differentiated from taste which is produced by CN VII.[1][2]
Structure and Function
As stated previously, the trigeminal nerve provides both sensory and motor innervation to the face. More specifically, the sensory information conducted by this nerve includes touch, pain, and temperature. This sensory information is relayed through the main trigeminal nucleus and nuclei of the thalamus before it travels to the cerebral cortex and synapses in the post-central gyrus. As with all other sensory information of the body, the sensory information from the face crosses over (decussates) to the contralateral brain hemisphere.
CN V is classified into three different branches that have distinct territories of innervation. These branches are namely the ophthalmic, the maxillary, and the mandibular nerves.[3][4][5][6][5]
Ophthalmic Nerve (V1)
The ophthalmic nerve is primarily responsible for the sensory innervation of the face and scalp above the orbits. It also contains sympathetic nerve fibers responsible for pupil dilation and supplies the ciliary body, iris, lacrimal gland, conjunctiva, and cornea. In addition to these superficial sensory functions, the ophthalmic nerve also supplies the superior portion of the nasal cavity, the frontal sinus, and even deeper structures including the dura mater and portions of the anterior cranial fossa.
Maxillary Nerve (V2)
The maxillary nerve is also a sensory branch, and it supplies the territory just below the orbits and above the mouth. This includes the inferior portion of the nasal cavity, the maxillary teeth, and maxillary sinus.
Mandibular Nerve (V3)
The mandibular nerve is the only branch of the trigeminal nerve that has both sensory and motor components. The motor component innervates all of the muscles of mastication (enumerated below). The sensory portion is responsible for pain and temperature information from the mandibular teeth, buccal mucosa, temporomandibular joint, the anterior two-thirds of the tongue, and the face below the territory of the maxillary nerve.
Muscles
The only branch of the trigeminal nerve that has a motor component in the mandibular nerve (V3). This branch supplies motor innervation to the facial muscles involved in mastication which include the masseter, temporalis muscle, and the lateral and medial pterygoids. Additionally, V3 gives off branches that innervate the tensor veli palatini, the mylohyoid, the tensor tympani, and the anterior portion of the digastric muscle.
Surgical Considerations
One of the most common surgical procedures related to the trigeminal nerve is surgical therapy for trigeminal neuralgia (discussed later). Even though surgery can offer the patient significant pain relief, it also has a considerable risk of permanent damage to the trigeminal nerve which could result in facial numbness. For this reason, surgical intervention is often recommended only after several pharmaceutical therapies have been attempted. The surgical interventions that are done for trigeminal neuralgia are split into two categories: non-destructive and destructive. The goal of non-destructive surgery is to alleviate nerve compression by removing any structure that may be impinging on the nerve and maintaining the nerve intact. Destructive procedures aim to disrupt the trigeminal nerve completely so that pain is no longer transmitted by the nerve. The result of a destructive procedure is the irreversible loss of sensation of the affected side of the face.[7][8][9]
Clinical Significance
Trigeminal Neuralgia
Trigeminal neuralgia is a clinical condition characterized by neuropathic pain within the sensory territory of the trigeminal nerve. This pain is often described as burning or shock-like, can have a sudden onset, and can last for several minutes. The causes of trigeminal neuralgia vary widely, but most commonly it is caused by nerve compression. Mechanical compression of the trigeminal nerve can be caused by things such as an aneurysm, arteriovenous malformation, tumor, and trauma. Diagnosis is typically made based on the clinical presentation alone once other possible causes such as postherpetic neuralgia or dental issues are ruled out. Treatment of trigeminal neuralgia depends on the cause. In cases where there is a structure compressing the nerve, surgical resection is a possibility. However, because surgery has many associated risks, many cases are treated pharmaceutically before any invasive intervention is attempted. The first-line treatment is carbamazepine, and second-line medications include lamotrigine, oxcarbazepine, phenytoin, gabapentin, pregabalin, and baclofen.[9]
Cluster Headache
Cluster headaches have a very similar presentation as trigeminal neuralgia, and therefore the two are often considered on the same differential. Cluster headaches most often present as a severe headache on one side of the head that affects the territory of the trigeminal nerve. These headaches can be accompanied by other symptoms such as nasal congestion, swelling, and lacrimation on the affected side. While the cause of cluster headaches is currently unknown, there is often an external stimulus that serves as a trigger for the onset of symptoms. Prophylactic treatment usually includes a combination of trigger avoidance and pharmacotherapy. Acute attacks can be remediated with fast-acting triptans and oxygen.
Wallenberg Syndrome (Lateral Medullary Syndrome)
Wallenberg syndrome is a condition that occurs when the lateral portion of the medulla in the brainstem becomes damaged, typically due to stroke. A lesion in this region of the brain stem results in an ipsilateral sensory loss in the territory of the trigeminal nerve and contralateral sensory loss in the rest of the body. Wallenberg syndrome is often recognized in the clinical setting to localize brainstem lesions.[10]
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)