
Varicose Veins
- Article Author:
- Meghal Antani
- Article Editor:
- Jeffery Dattilo
- Updated:
- 8/23/2020 9:45:24 PM
- For CME on this topic:
- Varicose Veins CME
- PubMed Link:
- Varicose Veins
Introduction
Venous reflux disease or venous reflux, which may also be referred to as chronic venous insufficiency, is a common condition. Venous reflux is usually the underlying cause of varicose veins, reticular veins, and telangiectasias (spider veins). In the lower extremities, venous reflux is categorized as superficial or deep. Superficial venous reflux involves the great and small saphenous veins and their tributaries, which are located between fascia and skin, and is treatable by a number of modalities including endovenous ablation, stripping, or avulsion. Deep venous reflux involves the femoral and other deep veins, which are located below the fascia, and is not readily treated by endovascular methods.
Mild cases of varicose veins just produce leg discomfort or maybe aesthetically unsightly but severe disease can lead to leg swelling and eventually ulcer formation.
This activity will focus on superficial venous reflux.[1][2][3]
Etiology
Venous reflux originates from the failure of the venous valves in the saphenous veins, which results in retrograde flow and stasis, or pooling, of venous blood in the branches of the saphenous veins. The normal ambulatory venous pressure in the extremity is regulated by the function of the valves. If the valves no longer function this can translate into elevated ambulatory venous pressure and can produce symptoms. The associated symptoms, including dilated visible veins at the skin surface (varicose veins, reticular veins, and telangiectasias), swelling, aching, heaviness, skin discoloration, and potential ulcer formation. A poor calf pump mechanism may worsen venous reflux.[4][5]
Risk Factors:
- Family history
- Female sex
- Increased age
- Multiple pregnancies
- Standing for long periods
- Obesity
- History of DVT
Ambulatory venous pressure with ambulation
- Normal - 70% reduction
- Varicose veins - 30-40% reduction
The varicose veins seen in pregnancy are usually due to hormonal changes, which make the valves defective and the walls thinner.
Epidemiology
Early stages of venous reflux may occur in as many as 25% of women and 15% of men. Later stages of venous reflux, such as venous ulceration, may occur in 5% of the population (Rabe 2016).
Varicose veins are seen globally and influenced by activity and lifestyle. Overall, varicose veins are more common in women than men.
Pathophysiology
There is a myriad of intrinsic and extrinsic faccotrs that contribute to the formation of varicose veins including, age gender, pregnancy, obesity, height, race, diet, occupation, hightory of DVT, and genetics. The primary pathologies related to varicose veins are 1) elevated venous pressure in the extremities and 2) defective or destruction of the valves resulting in a reflux and thus elevated venous pressure in the extremity.
History and Physical
The CEAP classification system of venous reflux is used to assess the clinical severity of symptoms:
- C0 no visible or palpable signs of venous disease
- C1 telangiectasies or reticular veins
- C2 varicose veins
- C3 edema
- C4a pigmentation and eczema
- C4b lipodermatosclerosis and atrophie blanche
- C5 healed venous ulcer
- C6 active venous ulcer
Initial diagnosis is by clinical evaluation of swelling, discoloration, and skin ulcerations.
Symptoms associated with varicose veins include:
- Leg heaviness
- Itching
- Cramps
- Mild tenderness
- Skin discoloration
- Exercise intolerance
- Leg fatigue
The physical exam may reveal visibly distended veins from the thigh to the ankle. The discoloration is usually most prominent around the ankle and calf. The Trendelenburg test is often used to assess the competency of the deep venous valves. The leg is elevated until all the superficial veins have collapsed. With the hand, the groin area is compressed to occlude the saphenofemoral junction and the patient is asked to stand up. If the deep valves are incompetent, then the leg superficial veins will start to fill up. If distal varicosity remains empty then the point of the entry is most likely at the saphenofemoral junction. This patient can benefit from ligation of the saphenous vein at this junction.
Evaluation
If venous reflux is suspected based on symptomatology and clinical evaluation the practitioner should obtain color duplex venous ultrasound exam. This study is an objective assessment of the anatomy of the veins as well as valvular function. During the ultrasound, evaluation for deep vein thrombosis should also be performed to confirm that DVT/obstruction is not contributing to the clinical scenario.[6][7]
Contrast venography is rarely done today.
Treatment / Management
Conservative Treatments
Most patients obtain adequate symptom relief by using long-term graduated compression stockings, and through leg elevation and oral pain medications. For compression rates the recommended graduation is 20-30 mmHg and in more severe cases can be elevated to 30-40 mmHg. [8][9][10] Stockings when worn daily are the ideal treatment for patients who do not want surgery. They do work but the heat and hot weather can reduce compliance.
Surgical Treatment
Traditional surgical treatment consisted of ligation and stripping of the greater saphenous vein with avulsion of tributary veins.
Endovascular Treatment
In the United States, surgical vein ligation and stripping has largely been replaced by catheter-based endovenous thermal ablation (EVTL). EVTL is performed with either laser or radiofrequency as the source of the heat energy. The EVTL procedure is typically performed under ultrasound guidance and with a local anesthetic. If a patient is anxious, an oral anxiolytic may be of benefit. Intravenous sedation is rarely required. During the EVTL procedure, a catheter is advanced (usually in an antegrade direction) into the incompetent saphenous vein, to within a few centimeters of the saphenofemoral (or saphenopopliteal junction). Tumescent anesthesia is administered to the entire length of the catheter. The catheter is connected to an external generator, and as the catheter is retracted out of the vein, the heat energy that is released by the catheter essentially cauterizes the saphenous vein in which the catheter is located. By doing so, the source of the reflux is eliminated. The venous blood return redirects via other "healthy" veins to the deep circulation.
Equally as popular is thermal ablation of the saphenous vein uring radiofrequency energy to ultimately ablate the saphenous vein conduit (RFA - Radiofrequency ablation). Approval for this technique was granted permission in 1999 by the FDA. Many studies have been published comparing the two techniques but the general consensus states that both are equally successful but there tended to be fewer side effects with RFA.
Supplemental Procedures
In addition to treating the venous reflux within the saphenous veins, many patients will also have visible superficial veins including reticular veins (1 mm to 3 mm diameter) and telangiectasias (under 1 mm diameter). Collectively these may be referred to as "spider veins" in lay terminology. In addition to being unsightly, may also be painful to local pressure. Liquid sclerotherapy involves the injection of a dilute medication (sclerosant) into the superficial telangiectasias and reticular veins. Phlebectomy involves the removal of larger superficial varicose veins through small 2 mm to 3 mm incisions.
Laser therapy is only used to treat the spider veins and is not useful for varicose veins.
Compression Therapy
Patients with milder symptoms of venous reflux disease may obtain adequate symptomatic relief with compression stockings. Compression stockings should at the minimum reach the level of the upper calf. Thigh-high compression stockings are preferable if tolerated. After most treatments for venous reflux and its stigmata, compression stockings are recommended, although exact guidelines for duration and strength of compression are not available. A common compression strength after ablation is 20 mmHg to 30 mmHg. Recommended length of compression therapy may range from several days to 2 weeks, depending on the severity of symptoms and type of treatment (Nazarko 2017). Some patients with more severe lower extremity swelling may benefit from a longer period of compression therapy, with possible adjunctive home-based pneumatic compression (Lurie 2017).
Post-Procedure Followup
After endovenous ablation treatment, most physicians recommend duplex ultrasound examination of the treated leg within the first week, focusing on the saphenofemoral (or saphenopopliteal) junction to evaluate for deep vein thrombosis, even though the likelihood of forming DVT after endovenous ablation is minimal, under 1% (Nazarko 2017).
Differential Diagnosis
- Lymphedema
- Deep vein thrombosis
- Cellulitis
- Stasis dermatitis
Prognosis
There is no cure for varicose veins. Even after surgical removal, recurrences are common. Those who develop venous ulcers have the highest morbidity and a poor quality of life. Unlike the deep venous system, clots in superficial veins rarely embolize and hence the risk of pulmonary embolism is rare. Untreated varicose veins reflect poor aesthetics and this is the key reason why most people seek treatment.
Complications
- Venous ulcers
- Pain
- Poor cosmesis
Deterrence and Patient Education
- Graduated compression hose
- Healthy weight
- Exercise
Pearls and Other Issues
Venous reflux disease is a common condition that results in a considerable lifestyle impact due to the symptoms of leg pain and swelling, and that has the potential to cause more significant morbidity by eventual venous ulcer formation. Treatment with endovenous ablation with a period of compression therapy is usually effective in reducing the associated symptoms.
Enhancing Healthcare Team Outcomes
Varicose veins are very common in society and often lead to poor cosmesis and fatigue. However, most patients seek medical assistance because of poor cosmesis. Today, general and vascular surgeons perform several different types of procedures to treat varicose veins but recurrence is a problem. More important, varicose vein surgery is considered cosmetic and not covered by most health plans, so the patient is left to pay for the entire cost. Each year, consumers spend millions of dollars on the care of varicose veins. In view of the fact that recurrences are common and that surgical procedures also have complications, prevention is key. The primary care provider, pharmacist, and nurse are in a primary position to educate the patient on how to prevent varicose veins. By wearing compression stockings, maintaining a healthy weight, and exercise, varicose veins can be prevented at low cost in most people. In addition, the patient should be educated that if the varicose vein is untreated, it can lead to a venous ulcer which is very difficult to cure and costs the healthcare system millions of dollars each year. Finally, when evaluating a patient with a varicose vein, suspicion for a DVT should be high and the patient should be referred for a duplex ultrasound. Before referring any patient for surgery, the primary care provider, nurse, and pharmacist should advise the patient to change lifestyle, stop smoking, elevate the legs at bedtime and wear stockings- for those who comply there is no need for any type of surgery.[11][12][13] (Level V)
Evidence-based Outcomes
Every type of surgical procedure has good to excellent outcomes for varicose veins, but each one is associated with recurrence. For those who develop a venous ulcer, the morbidity is very high as there is no cure. It is also important to note that patients with varicose veins are also at high risk for deep vein thrombosis, which requires prolonged treatment with an anticoagulant which carries further morbidity from the side effects like bleeding. (Level V) Hence, an interprofessional approach to varicose veins is recommended to achieve good outcomes. [9][3][14](Level V)
(Click Image to Enlarge)
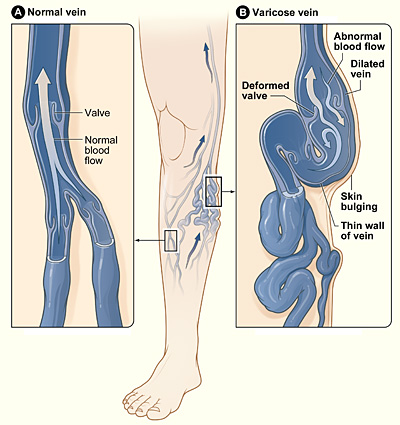
The illustration shows how a varicose vein forms in a leg. Figure A shows a normal vein with a working valve and normal blood flow. Figure B shows a varicose vein with a deformed valve, abnormal blood flow, and thin, stretched walls. The middle image shows where varicose veins might appear in a leg.
Contributed by National Heart Lung and Blood Institute
