Neuroanatomy, Vestibular Pathways
- Article Author:
- Hannah Yoo
- Article Editor:
- Dana Mihaila
- Updated:
- 10/28/2020 1:03:02 AM
- For CME on this topic:
- Neuroanatomy, Vestibular Pathways CME
- PubMed Link:
- Neuroanatomy, Vestibular Pathways
Introduction
The vestibular system is an essential function of the body that helps humans to maintain postural balance and spatial orientation in response to changes in the environment. Starting from the inner ear, a complex interplay among constituents in the vestibular pathway allows sensory information to reach multiple destinations in the body and make simultaneous outputs. Any disruption along the pathway leads to various symptoms, including imbalance and uncoordinated eye movements. This review discusses the anatomy of the vestibular system and its clinically significant pathological conditions, such as vestibular schwannoma, oscillopsia, and Wallenberg syndrome, to help readers make the right diagnosis based on specific signs and symptoms pertaining to each vestibular lesion.
Structure and Function
Labyrinths
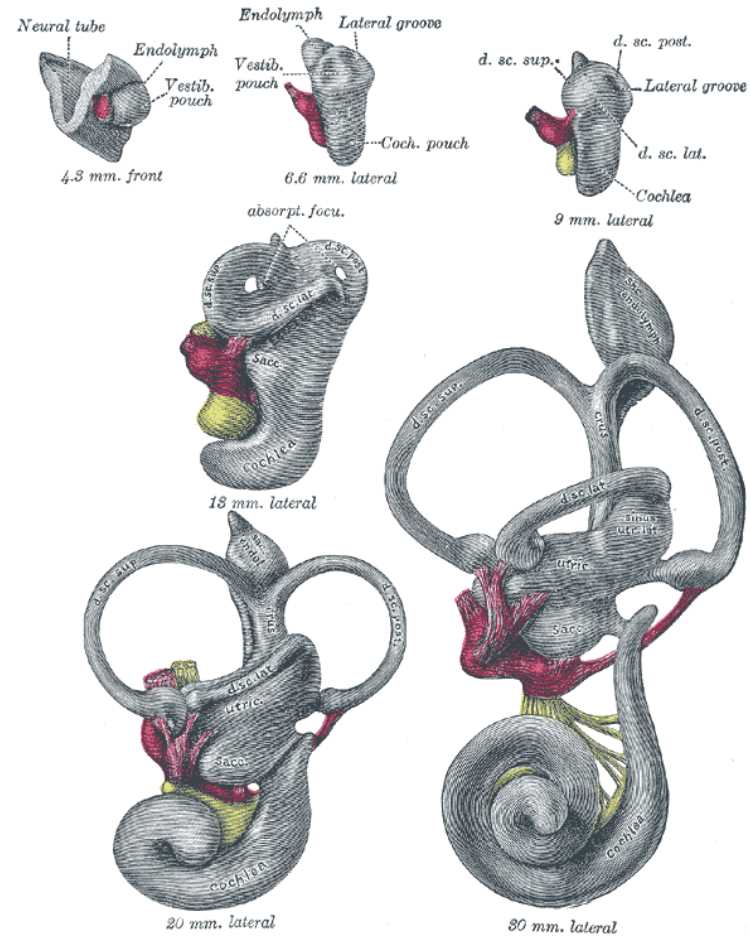
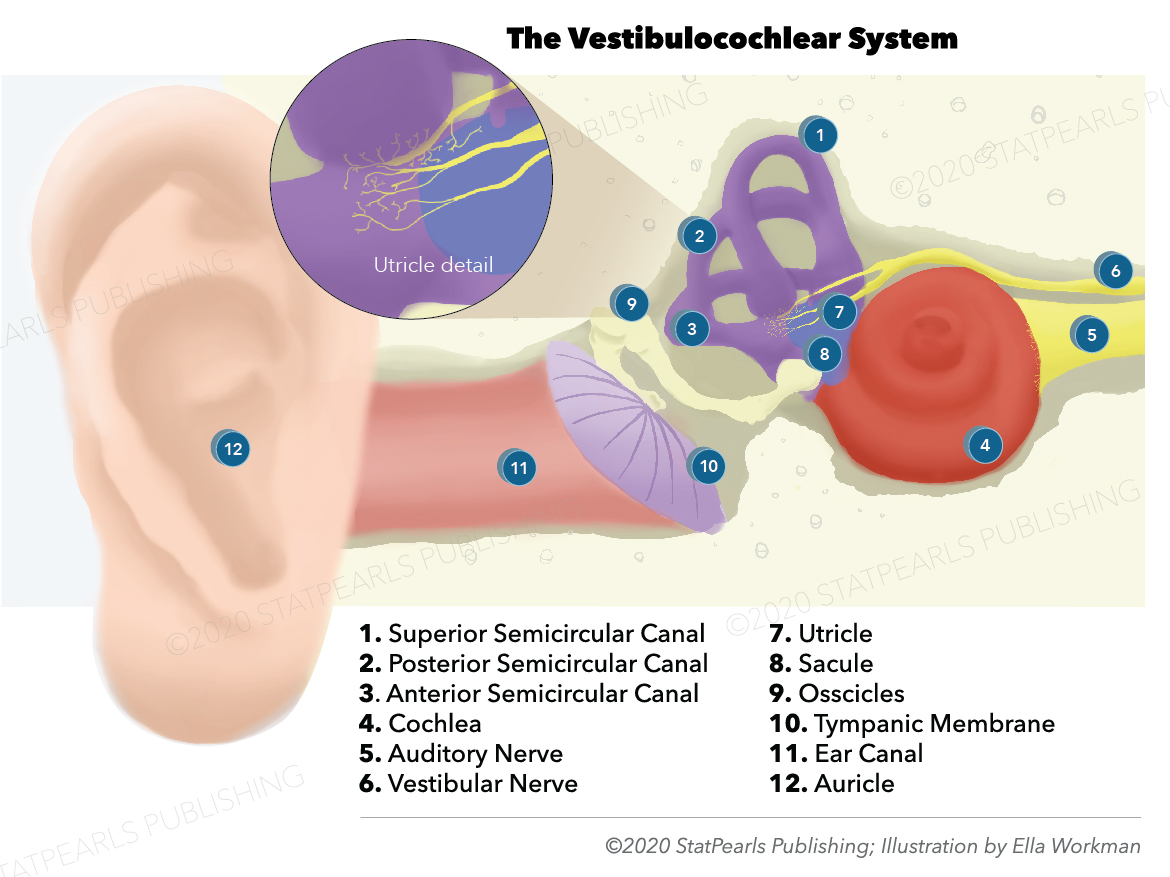
The inner ear located within the petrous temporal bone comprises the bony and membranous labyrinths. The bony labyrinth in each ear is composed of the vestibule, three semicircular canals, and the cochlea that are filled with perilymph. The three canals are superior, lateral, and posterior semicircular canals that are located posterior and superior to the vestibule. Within the bony labyrinth, the membranous labyrinth filled with endolymph is observable. The membranous labyrinth comprises the utricle and saccule, three semicircular ducts, and the cochlear duct. The utricle and saccule are also known as the otolith organs.
Many afferent nerve signals originate in these peripheral vestibular organs and travel to the vestibular centers located in the brain. The utricle and saccule contain sensory receptors for static equilibrium, which maintains the head position in response to linear acceleration of the body (i.e., starting to walk or stopping). The hair cells of the utricle and saccule have stereocilia that are embedded in the otolithic membrane. The semicircular ducts are positioned on three perpendicular planes and correspond to three directions of the head movement. The semicircular ducts contain sensory receptors for dynamic equilibrium, which maintains the head position in response to the rotational acceleration of the body (i.e., turning). Their hair cells are located in the crista ampullaris, a cone-shaped neuroepithelial structure in the semicircular ducts. Upon either linear or rotational acceleration, a corresponding deflection of the hair cell bundle leads to a depolarization of the hair cell membrane potential and initiates a relay of sensory information through the vestibular pathways.[1][2][3][4]
Vestibular Pathways
Hair cells of the peripheral vestibular structures receive their innervation from peripheral processes of bipolar neurons of the vestibular ganglion (also known as Scarpa’s ganglion), which is located inside the internal auditory meatus of the petrous temporal bone. As the vestibular portion of the cranial nerve VIII (CN VIII), the central processes of these bipolar neurons enter the brainstem at the pontomedullary junction and project to the vestibular nuclei or the flocculonodular lobes of the cerebellum via the inferior cerebellar peduncle.[5]
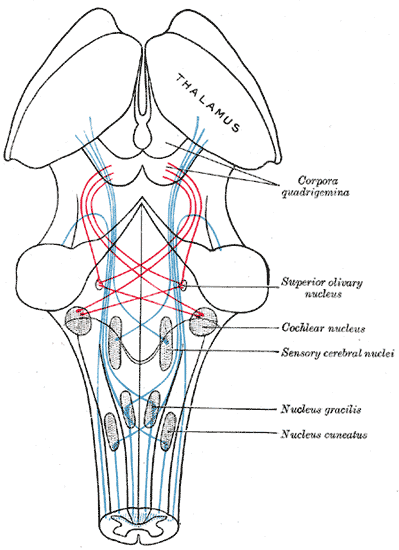
Four vestibular nuclei are lateral to the sulcus limitans and medial to the inferior cerebellar peduncle. They are observable near the level of the fourth ventricle in the medulla and pons. The vestibular nuclei receive vestibular information from the CN VIII and send projections to the spinal cord, extraocular motor nuclei, thalamus, or cerebellum. Lesions to these nuclei may lead to nystagmus, vertigo, and unsteadiness. Because the spinal tract and nucleus of CN V are located close to the vestibular nuclei at the rostral medulla, a lesion of the vestibular nuclei at the level of rostral medulla may also involve these structures leading to facial numbness and tingling.
Spinal Cord
The lateral and inferior vestibular nuclei project motor neuron fibers which descend ipsilaterally through the lateral vestibulospinal tract. The lateral vestibulospinal tract travels along the ventral regions of the white matter of the entire spinal cord. Collateral nerves arise from the lateral vestibulospinal tract and synapse with the medial motoneuron, which innervates proximal muscles of the limb, in the ventral gray horn. This lateral pathway facilitates the contraction of forelimb and hindlimb muscles to maintain balance and upright posture.
The neurons that travel down the medial vestibulospinal tract originate in the medial vestibular nucleus. They project bilaterally through the medial longitudinal fasciculus (MLF) and synapse with the medial ventral horn of the cervical cord. These neurons are responsible for the contraction of neck muscles and stabilization of head position when they receive information from the semicircular canals. The sternocleidomastoid muscle (SCM) is one of the main muscles innervated by the medial vestibulospinal tract, and a patient with the lesion tract cannot turn his or her head to the contralateral side.[6][7]
Extraocular Motor Nuclei
The connection between the vestibular system and extraocular muscles allows the eyes to maintain stability by fixating on a target point during head movements. Via the vestibulo-ocular reflex, the eyes move in the opposite direction of the head motion and stabilize the image on the retina. The vestibulo-ocular reflex initiates when the head turns and activates the semicircular canals. Then the vestibular information travels through the CN 8 to reach the superior and medial vestibular nuclei, which project fibers rostrally through the MLF to synapse with the abducens nucleus (CN 6), trochlear nucleus (CN 4), and oculomotor nucleus (CN 3). The superior and medial vestibular nuclei send signals to the ipsilateral CN 3 and contralateral CN 6, thus coordinating horizontal eye movements. The trochlear nuclei are located in the medial midbrain and give off motoneurons which project dorsally around the periaqueductal gray matter and decussate before exiting the dorsal aspect of the brainstem. The nerves then innervate the contralateral superior oblique muscle.[8][5][9][10]
Thalamus
Thalamus is a relay center that receives fibers from the bilateral vestibular nuclei and projects them to the cerebral cortex. The ventral posterior (VP) nucleus of the thalamus is composed of the ventral posterolateral (VPL), ventral posteromedial (VPM), and ventral posteroinferior (VPI) nuclei. The VP receives vestibular information from the bilateral superior vestibular nuclei and the contralateral medial vestibular nucleus via the MLF. The efferent fibers of the VP nucleus travel through the posterior limb of the internal capsule and to the primary somatosensory cortex. From the primary somatosensory cortex, the signals relay to the primary motor cortex and the posterior parietal cortex, which plays a role in the spatial orientation of the body. Lesions of the thalamus lead to a tilted perception of visual vertical and unsteady stance and gait.[11]
Cerebellum
The flocculonodular lobe, which is also known as the vestibulocerebellum, is the most caudal portion of the cerebellum that plays a role in balance and eye movements. It receives afferent fibers from the ipsilateral vestibular ganglion and vestibular nuclei, as well as from the visual cortex and the pretectum of the midbrain. The CN 8 signals reach the cerebellum via the inferior cerebellar peduncle. The efferent fibers project from the flocculonodular lobe via the inferior cerebellar peduncle and terminate in the vestibular nuclei, from which the nerve fibers project and innervate the CN 3, 4, and 6 nuclei to regulate eye movements. The medial portion of the flocculonodular lobe, known as the nodule, contributes to maintaining balance, while the lateral portion known as the flocculus regulates the smooth pursuit eye movements (eyes following a slow-moving target). The flocculus is also involved in the control of reflexive eye movements. Damage to the cerebellum leads to impairments in the quality of movements but does not result in a total loss of function. Vestibulocerebellar lesions cause various eye movement disorders, including nystagmus.[12][9][13]
Cerebral Cortex
The nerve fibers of the thalamus proceed to the cerebral cortex, which is the final destination of information concerning spatial orientation and motion. The signals relayed to the cortex join with other proprioceptive information to initiate a response for maintaining balance. The vestibular cortex is composed of a network of multiple temporoparietal areas which also receive somatosensory and visual information. The parietoinsular vestibular cortex (PIVC) is the primary cortical region in the posterior insula that is responsible for the vestibular function. Lesion of the posterior insula may lead to subjective visual vertical tilt. One-sided activation of the vestibular system leads to the ipsilateral activation of the vestibular cortex.[14]
Embryology
Similar to the auditory organs, the vestibular organs are the constituents of the inner ear that derive from the otic vesicle, which is a sac-like epithelial tissue that arises from the otic placode. The otic placode, a thickening ectodermal layer of an embryo, is the first visible indication of inner ear development. Once the otic vesicle arises from the otic placode, neuroblasts delaminate from the otic vesicle and coalesce to form the statoacoustic ganglion (SAG). The SAG supplies the sensory innervations to the inner ear. As its development progresses, the otic vesicle modifies its shape to form a fluid-filled labyrinth with auditory and vestibular sensory organs.[15][16][17]
Blood Supply and Lymphatics
Anterior inferior cerebellar arteries (AICA) and posterior inferior cerebellar arteries (PICA) are the major arteries that are involved in the vestibular system vascularization. The labyrinthine artery most commonly branches from the AICA, while it occasionally branches from the basilar artery and supplies the CN VIII (vestibulocochlear) and CN VII (facial) nerves. As the labyrinthine artery travels with the CN VIII and CN VII through an opening called the internal auditory meatus to enter the inner ear, it divides into the anterior vestibular, cochlear, and vestibulocochlear arteries. The anterior vestibular artery supplies most of the utricle, the vestibular nerve, and part of the semicircular canals. The cochlear artery is the main vasculature of the cochlea. The vestibulocochlear artery supplies the saccule and a portion of the cochlea and semicircular canals. The AICA supplies the flocculus of the cerebellum. An AICA infarction may result in multiple symptoms such as vertigo, hearing loss, facial weakness and sensory loss, Horner syndrome, and gait and limb ataxia.[18][19][20]
The PICA arises from the vertebral arteries and supplies the inferior cerebellar peduncle, vestibular nuclei, spinal tract and nucleus of CN V, and posterior cerebellum. The PICA also supplies the nodulus of the cerebellum. Occlusion of the PICA may result in lateral medullary syndrome, which is also known as Wallenberg syndrome. Wallenberg syndrome will be discussed more in detail under the section of clinical significance. [21][22][23]
Nerves
Vestibulocochlear Nerve
The vestibulocochlear nerves carry vestibular information from the semicircular canals, utricle, and saccule and pass through the internal acoustic meatus together with the facial nerve. The vestibular portion enters the brainstem at the pontomedullary junction and travels through the inferior cerebellar peduncle to reach the vestibular nuclei or the flocculonodular lobes of the cerebellum. Benign tumors of the Schwann cells may arise from the vestibular portion of CN VIII and result in vestibular symptoms.[5]Oculomotor, Trochlear, and Abducens Nerves
CN III, IV, and VI nerves innervate the six extraocular muscles that control eye movements in response to head movements. When the head turns to the left, vestibular information initiates its journey from the left semicircular canal via vestibular nerve fibers and proceeds to the ipsilateral medial and superior vestibular nuclei. Then, excited neurons in the left superior and medial vestibular nuclei send signals to the right CN VI nucleus. The right CN VI innervates the right lateral rectus muscle to contract and direct the gaze to the right. Another nerve fiber projects from the CN VI nucleus and ascends via the MLF toward the left CN III nucleus. When stimulated, the oculomotor nerve results in the medial rectus muscle contraction and allows the left eye to gaze to the right. Inhibitory nerve fibers also proceed from the medial vestibular nucleus to the left CN VI nucleus, rendering the left lateral rectus and right medial rectus muscles to relax. The result of these combined counteracting effects is a smooth, coordinated eye movement toward the opposite direction, and thus a steady visual field with head-turning. The trochlear nerves innervate the contralateral superior oblique muscle and stimulate the muscle to contract and make eye movements via lateral rotation, intorsion, and depression.[8][24]
Clinical Significance
Vestibular Schwannoma
Also known as acoustic neuromas, benign tumors of the Schwann cells arise from the vestibular portion of the CN 8. These growths most commonly appear at the cerebellopontine angle, the region between the cerebellum and the pons. Patients with vestibular schwannoma commonly experience progressive ipsilateral hearing loss and tinnitus as the tumor grows and compresses the cochlear portion of the CN VIII. Imbalance or rarely vertigo also accompanies hearing loss due to the damaged vestibular portion of the CN VIII. Patients will also experience nystagmus when the cerebellar flocculus becomes compressed. If untreated, large tumors may further involve other structures such as the CN VII or CN V. Due to their proximity to the CN VIII; facial nerve damage may lead to facial paralysis. CN V lesion may result in numbness and tingling sensation on the face.[25][26]
Oscillopsia
Damage of the vestibulo-ocular reflex leads to oscillopsia. The incoordination between the vestibular and ocular systems prevents the information about head and body movements from reaching the oculomotor centers. As a result, the patient has difficulty fixating on a target point while the head turns. Bilateral loss of vestibular function leads the patient to believe that the world is moving with head movements. Vertigo, dizziness, and imbalance are common symptoms of oscillopsia.[27]
Wallenberg Syndrome
Because the PICA innervates multiple organs such as the inferior cerebellar peduncle, vestibular nuclei, spinal tract and nucleus of CN V, and posterior cerebellum, its occlusion results in various symptoms. Vertigo, loss of balance, and vomiting may result due to its involvement with the vestibular nuclei. A patient with the syndrome also presents ipsilateral cerebellar signs due to its involvement with the inferior cerebellar peduncle and cerebellum. Ipsilateral ataxia can also present. Patients with the syndrome tend to fall to the ipsilateral side. Loss of ipsilateral facial pain sensation can also occur due to its association with the spinal tract and nucleus of CN V.[21]
(Click Image to Enlarge)
(Click Image to Enlarge)