Wrist Fracture
- Article Author:
- Hunter Hsu
- Article Author:
- Matthew Fahrenkopf
- Article Editor:
- Shivajee Nallamothu
- Updated:
- 8/10/2020 9:32:12 PM
- For CME on this topic:
- Wrist Fracture CME
- PubMed Link:
- Wrist Fracture
Introduction
A distal radius fracture, commonly known as a wrist fracture, is defined by the involvement of the metaphysis of the distal radius. The fracture may or may not involve the radiocarpal joint, distal radioulnar joint, and/or the distal ulna.[1] This injury is commonly associated with high-energy mechanisms in younger patients and lower energy mechanisms or falls in older patients.[2] The fracture results in acute wrist pain and swelling, and if left untreated, it can result in significant morbidity. Treatment can involve both non-operative and operative management and ultimately depends on multiple factors.[3]
Etiology
The mechanism of injury in a distal radius fracture is an axial force across the wrist with the pattern of injury determined by bone density, the position of the wrist, and the magnitude and direction of the force. Most distal radius fractures result from falls with the wrist extended and pronated.[1] This action places a dorsal bending moment across the distal radius. This type of injury is often referred to as a "fall onto an outstretched hand" or FOOSH. The relatively weaker, thinner dorsal bone collapses under compression; whereas, the stronger volar bone fails under tension resulting in a characteristic “triangle” of bone comminution with the apex volar and greater comminution dorsal. Cancellous impaction of the metaphysis compromises dorsal stability, and shearing forces impact the injury pattern, which often involves the articular surface.[4] High-energy injuries may result in significantly displaced or highly comminuted unstable fractures to the distal radius.
Common mechanisms in younger individuals
- Falls from height
- Motor vehicle accident
- Injuries sustained during athletic participation
Common mechanisms in elderly individuals
- Simple falls from standing height
Epidemiology
A distal radius fracture is the most common fracture of the upper extremity.[1] These fractures happen in all patient populations and are the most common orthopedic injury with a bimodal distribution. More than 450,000 fractures occur annually in the United States, and that number continues to rise. Fractures of the distal radius represent approximately one-sixth of all fractures treated in emergency departments. Younger patients tend to be involved in higher energy trauma mechanisms, whereas older patients tend to be involved with lower energy falls. The incidence in the elderly population correlates with osteopenia and rises in incidence with increasing age which corresponds to the increased incidence of hip fractures.[5]
Risk factors in the elderly
- Decreased bone mineral density
- Female gender
- White race
- Family history
- Early menopause
Pathophysiology
Wrist fractures are common in patients with osteoporosis. Almost any type of fall on the hand is associated with a risk of wrist fracture.
History and Physical
Patients will typically present with variable wrist deformity and displacement of the hand relative to the wrist. The wrist usually swells, with ecchymosis, tenderness, and painful range of motion. The mechanism of injury should be investigated to assist in assessing the energy and level of destruction. It is essential to establish the patient’s functional status before the injury as well as occupational demands as these may aid in determining treatment direction. Document co-existing medical conditions that may affect healing such as osteoporosis, diabetes, and/or tobacco use.
The physical examination should include careful attention to the following:
- Condition of the surrounding skin and soft tissue
- Quality of vascular perfusion and pulses
- The integrity of nerve function
- Sensory 2-point discrimination
- Motor function of intrinsic, thenar, and hypothenar muscles of the hand
- Careful attention to median nerve function as acute carpal tunnel syndrome can occur up to 20% of the time[6]
- The integrity of the median nerve requires assessment and documentation
Associated injuries include:
- Ipsilateral elbow
- Ipsilateral shoulder
- Distal radial ulnar joint
- Radial styloid fracture
- Triangular fibrocartilage complex
- Scapholunate ligament
- Lunotriquetral ligament
Evaluation
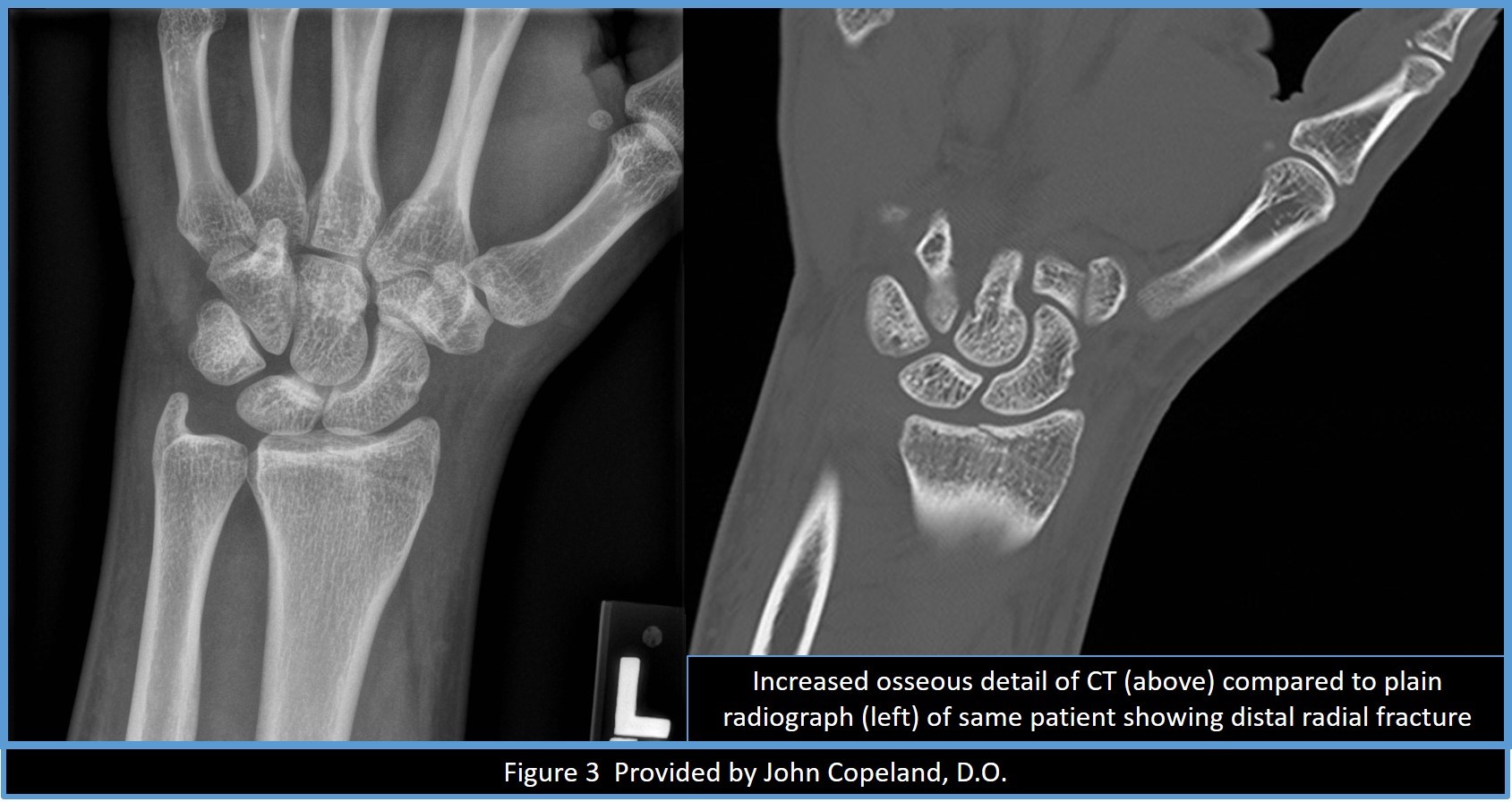
Imaging confirms fracture severity, determines stability, and guides the treatment approach. Plain radiographs should be obtained before and after reduction, if necessary. The standard radiographs include posteroanterior and lateral views of the wrist, as well as oblique views for further fracture definition. Oblique views are useful to help evaluate articular involvement, particularly the lunate fossa fragment. Contralateral wrist views may evaluate the patient’s normal ulnar variance and scapholunate angle. Computed tomography scan may demonstrate the extent of intraarticular involvement. It is important to know normal radiographic measurements of the distal radius because it is useful in identifying distal radius fractures. These measurements are also useful in determining treatment.
Important normal radiographic relationships include[7][8]:
- Radial inclination: Average of 23 degrees
- Radial height: Average of 11 mm
- Volar tilt: Average of 11 degrees
Treatment / Management
Distal radius fractures may have either surgical or non-surgical treatment. Non-surgical treatment necessitates acceptable fracture displacement, angulation, and shortening. Should these criteria not be met, surgical treatment is the recommended approach.
Acceptable criteria for distal radius fractures include:
- Radial height: Less than 5 mm shortening
- Radial inclination: Less than 5-degree change
- Articular step off: Less than 2 mm
- Volar tilt: Dorsal angulation less than 5 degrees or within 20 degrees of the contralateral distal radius
Displaced fractures must undergo a closed reduction in an attempt to achieve an anatomic or acceptable reduction. Adequate anesthesia or analgesia, such as conscious sedation or hematoma block, are necessary for closed reduction.[9] Following the closed reduction, the arm should be immobilized in a long-arm, sugar-tong splint acutely, as opposed to a cast. A long-arm, sugar-tong splint prevents pronation, supination, and elbow flexion, thereby eliminating the brachioradialis as a deforming force. The splint will allow for swelling as opposed to a cast.[10] Post-reduction radiographs must be obtained to evaluate the quality of the reduction. If the fracture reduction meets the acceptable criteria, the patient may remain in the splint and follow up with an orthopedic surgeon where weekly radiographs will be obtained for the first 2 weeks. If the reduction is not maintained and is no longer acceptable, surgical intervention should be recommended. If the reduction is maintained, the splint may be converted to a cast and immobilized for a total of 6 weeks.
Non-displaced fractures are treated without surgery in a long-arm splint acutely and transitioned to a short-arm cast in the office for a total of 6 weeks with serial radiographs to monitor for fracture displacement and healing.
For fractures that do not meet acceptable alignment, surgical intervention is recommended.[3] The goal of surgical treatment is to achieve acceptable alignment and stable fixation for early motion. There are various methods of fixation, including pins, external fixators, dorsal plates, and a volar plate. Percutaneous pinning is useful in maintaining sagittal length and alignment in extra-articular fractures with a stable volar cortex. It is unacceptable when the volar cortex is comminuted, and therefore unstable, as there is not enough bony fixation to maintain reduction. Good outcomes have been reported up to 90% of the time if used appropriately. External fixation is often used in conjunction with percutaneous pin or plate fixation as it does not reliably restore the volar tilt on its own. This technique relies on ligamentotaxis to maintain fracture reduction. It is essential to limit the duration of external fixation to a maximum of 8 weeks and to perform aggressive hand therapy to maintain range of motion of the hand. Good outcomes have been reported up to 90% of the time if used appropriately. Open-reduction internal fixation with volar plating is much more common than dorsal plating. Volar plating is associated with irritation of both flexor and extensor tendons, and flexor pollicus longus tendon rupture may have occurred.[11][12] Volar plating offers support to the subchondral bone to help maintain fracture reduction. Dorsal plating is associated with extensor tendon irritation and rupture. It is typically necessary for displaced intra-articular fractures with dorsal comminution.
Differential Diagnosis
Radiographs confirm the diagnosis; however, the following must merit consideration:
- Associated and contributory injuries should always be in the differential
- Pathologic fracture
- Associated injuries to the carpus
Staging
Multiple Classification Systems of Distal Radius Fractures
Frykman Classification
Based on the pattern of intraarticular involvement
- Extraarticular distal radius fracture
- 1 + distal ulna fracture
- Intraarticular distal radius fracture involving radiocarpal joint
- 3 + distal ulna fracture
- Intraarticular distal radius fracture involving distal radioulnar joint
- 5 + distal ulnar fracture
- Intraarticular distal radius fracture involving radiocarpal and distal radioulnar joint
- 7 + distal ulna fracture
Fernandez Classification
Based on the mechanism of injury
- Metaphyseal bending fracture with the inherent problems of loss of volar tilt and radial shortening relative to the ulna
- Shearing fracture requiring reduction and often buttressing of the articular segment
- Compression of the articular surface without the characteristic fragmentation; also the potential for significant interosseous ligament injury
- Avulsion fracture or radiocarpal fracture-dislocation
- Combined injury with significant soft tissue involvement owing to high-energy injury
Common Eponyms for Distal Radius Fractures
Colles fracture
- Low energy, intraarticular and extraarticular distal radius fracture demonstrating dorsal angulation, dorsal displacement, and radial shortening
- Clinically, described as a “dinner fork” deformity
Smith fracture
- Low energy, extraarticular distal radius fracture demonstrating volar angulation
Barton fracture
- Fracture-dislocation or subluxation of the wrist. The dorsal or volar rim of the distal radius gets displaced with the hand and carpus
- Volar involvement is more common
Chauffeur’s fracture
- Avulsion fracture of the radial styloid
Die-punch fracture
- A depressed fracture of the lunate fossa of the articular surface of the distal radius
Prognosis
Overall good to excellent results can be expected in over 80% of patients regarding a range of motion, strength, and outcomes scoring with open-reduction internal fixation and volar plating. Studies comparing volar fixation to other forms of fixation have revealed similar if not superior results. Results appear to be superior in the early recovery period with the outcome yielding equivalent results among all fixation groups. Some studies suggest better maintenance with volar plating in overall reduction compared to other forms of fixation.[1]
Complications
Median Nerve Neuropathy (Carpal Tunnel Syndrome)[6]
- Most frequent neurologic complication
- One percent to 12% of low-energy fractures and up to 30% of high-energy fractures
- Treat with acute carpal tunnel release in progressive paresthesias, weakness in thumb opposition if symptoms do not respond to closed reduction, and if they last greater than 24 to 48 hours
Extensor Pollicus Longus Tendon Rupture[11][12]
- Nondisplaced distal radius fractures have a higher rate of spontaneous rupture of the extensor pollicus longus tendon
Radiocarpal Arthrosis
- The reported incidence of up to 30%
- Ninety percent of young adults will develop symptomatic arthrosis if articular step-off is greater than 1 to 2 mm
- May also be asymptomatic
- Malunion and nonunion
Compartment Syndrome
Complex Regional Pain Syndrome
Postoperative and Rehabilitation Care
Postoperative care for open-reduction internal fixation with volar plating includes immediate volar splinting following surgery. The patient is instructed to perform active range of motion exercises for the digits and elevate their wrist above heart level to prevent stiffness and aid in edema control. The splint is removed 1 to 2 weeks after surgery for a wound check. A removable splint should be fabricated by a hand therapist to help with edema and worn at all times to protect fracture fixation. The patient should remain non-weight bearing of the upper extremity but may begin active range of motion exercises of the wrist after the first post-operative visit. At 4 to 6 weeks putty and grip exercises may be added. At 6 to 8 weeks, the splint is discontinued, and progressive strengthening exercises are advanced. The patient will typically be discharged to activities as tolerated at the 10 to 12-week mark.
Enhancing Healthcare Team Outcomes
Wrist fractures are complex because of the number of anatomical structures that may be involved. The majority of these patients have their initial encounter with the nurse practitioner or emergency department physician. Once the diagnosis of wrist fracture is made, an orthopedic or hand surgery consult is usually the next step. Poorly managed wrist fractures demonstrate enormous morbidity and often lead to limited use of the hand. Asides from pain control and stabilization, these patients should receive a referral to a hand or orthopedic surgeon. Mild fractures may undergo management with closed reduction, but severely displaced fractures may require ORIF.
Once the wrist fracture is managed, the primary care clinicians should follow the patient for pain management, which can be significant. Before recommending the patient back to work, the orthopedic surgeon should re-examine the patient. Long term monitoring is necessary because even surgery has its complications, and not everyone obtains the desired result. Communication between the team members should be open to ensure that the patient receives the optimal level of care. Nursing will play a pivotal role in either surgical or conservative management, but monitoring on followup visits, checking progress and coordinating with any physical or occupational therapy. This type of interprofessional coordination is necessary to achieve optimal outcomes and minimize morbidity.
The outlook for most patients is fair, but a significant number do have chronic pain and limited range of motion after treatment. Physical therapy is a must to regain muscle function and strength.[13][14]