Xanthochromia
- Article Author:
- Carla Dugas
- Article Author:
- Zohaib Jamal
- Article Editor:
- Pradeep Bollu
- Updated:
- 8/13/2020 7:05:34 PM
- For CME on this topic:
- Xanthochromia CME
- PubMed Link:
- Xanthochromia
Introduction
Xanthochromia was originally a broad term used to describe the pigmentation of cerebrospinal fluid (CSF) as pink or yellow.[1] This color change is attributed to varying concentrations of pigmented compounds such as oxyhemoglobin, bilirubin, and methemoglobin that are typically the byproducts of red blood cell degradation.[2] The term now is more widely accepted to represent the yellow color created by the presence of bilirubin in the CSF. The presence of bilirubin resulting in yellow discoloration of the CSF is the contemporary definition of xanthochromia.[3][4][5]
Etiology
Bilirubin is the byproduct of the degradation of oxyhemoglobin by the enzyme oxygenase. There are many causes of xanthochromia such as acute intracerebral hemorrhage, brain tumors, infection, increased protein, and severe systemic jaundice. The finding of xanthochromia in the CSF is most commonly used in the diagnosis of subarachnoid hemorrhage (SAH) in the presence of a normal head computed tomography. [6]
Epidemiology
The rupture of an intracerebral aneurysm most commonly causes subarachnoid hemorrhage. The incidence of SAH is anywhere from 9 to 15 people per 100,000 in the United States with rates that vary by geography. Risk factors include hypertension, cigarette smoking, alcohol use, some sympathomimetic drugs, and some genetic causes that increase the risk of a cerebral aneurysm. [7]
Pathophysiology
Once a cerebral aneurysm has ruptured or started to leak, blood may be found in the CSF in varying quantities. Over time this blood is degraded by macrophages and broken down into its byproducts containing bilirubin. The process of conversion from heme to bilirubin in the CSF takes 6 to 12 hours and can only happen in vivo. Therefore, xanthochromia is best identified 6 to 12 hours after the onset of a bleed. Even though CT scan in the investigative modality of choice for subarachnoid hemorrhage, nearly 5% of cases will have no CT evidence of hemorrhage during the first 24 hours. This percentage increases to 50% by the first week and is about 30% at 2 weeks. On the other hand, xanthochromic is seen in all patients for up to 14 days and can be present in 75% of patients for at least 21 days.
Histopathology
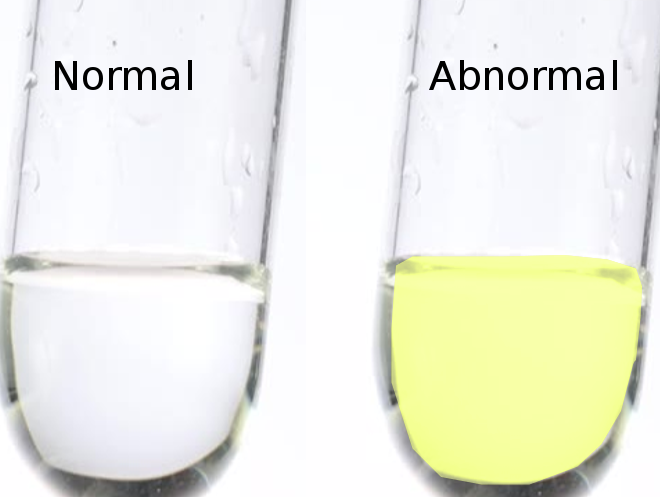
There are currently 2 different methods to identify xanthochromia in the CSF. In the United States, visual detection is still the method of choice. A CSF sample is spun down in a centrifuge, and the supernatant is visually inspected with the naked eye for yellow color. This is accomplished by holding a vial of water next to a vial of supernatant against a white backdrop.
The second and perhaps a more reliable way to test for xanthochromia is the use of spectrophotometry.[8] A spectrophotometer measures the absorption of light of the material and identifies that material based on the wavelength of light it absorbs. Bilirubin itself has a narrow window of detection with a wavelength of 440 to 460 nm. Multiple studies show the superiority of spectrophotometry when compared to visual inspection.[9] There are several factors that can interfere with the appearance of xanthochromia on visual inspection alone. For instance, the presence of proteins or pigments such as carotenoids can obscure the color change associated with the presence of xanthochromia. The presence of oxyhemoglobin with an acute bleed or traumatic lumbar puncture appears pink or orange and can hide the yellow discoloration of xanthochromia leading to a false-negative result. Furthermore, unlike spectrophotometry, a visual inspection cannot detect low concentrations of bilirubin and cannot distinguish bilirubin from oxyhemoglobin. [3]
History and Physical
Subarachnoid hemorrhage is a rare but significant disease that can lead to sudden death and disability if not diagnosed and treated properly. Patients often present complaining of the worst headache of their life.[5] A sudden onset at a maximal intensity or within the first hour of onset often characterizes headaches. There can be associated with meningismus, nausea, vomiting, photophobia, and/or phonophobia but rarely with acute neurologic deficits.[10] It can be difficult to distinguish between a non-traumatic headache associated with SAH or another less serious cause.
Evaluation
Non-contrast computed tomography of the head (NCHCT) is still the initial test of choice in the diagnosis of subarachnoid hemorrhage.[11] The sensitivity of this test is greatest within the first 6 hours of the onset of symptoms.[5] The current standard of care is to obtain an NCHCT followed by a lumbar puncture to evaluate for xanthochromia if the NCHCT is negative. The finding of xanthochromia in the CSF is helpful in that it is 93% sensitive and 95% specific with a positive predictive value of 72% and a negative predictive value of 99%.[12] Xanthochromia is typically present in the CSF within 6 to 12 hours after the onset of symptoms. Unlike CT, xanthochromia is present in the CSF in all patients up to 2 weeks post ictus and is still present in 70% of patients Up to three weeks later.[13] Furthermore, sensitivity for detecting a bleed by CT decreases from up to 95% on day 1 to less than 10% in 3 weeks, with the sensitivity of CSF analysis remaining constant near 100% over this time.[9] Because the production of bilirubin is a process that happens only in vivo, the presence of xanthochromia in the CSF is the only way to differentiate between a true hemorrhage and a traumatic tap as both can contain large amounts of red blood cells (RBCs).[14]
Treatment / Management
Once the patient is diagnosed with a SAH based on the findings of xanthochromia in the CSF, they may be sent for magnetic resonance imaging (MRI), CT angiography, or taken directly for treatment. The next step in management is to find the location of an aneurysm and thus the cause of the SAH.[15]
Differential Diagnosis
- Aneurysmal leaks
- Pseudomonal meningitis
- Severe hyperbilirubinemia
- Subarachnoid haemorrhage
- Sentinel haemorrhage
Complications
It is very difficult to determine the pretest probability of SAH based on presentation alone. There is no one factor that could determine the need for further testing for an acute non-traumatic headache. Lumbar puncture is an invasive procedure, and often results are misleading and non-diagnostic.[16][17][16] There is a very specific subset of patients in whom a lumbar puncture with the finding of xanthochromia will correctly diagnose a SAH. The majority of patients with negative head CT will not be diagnosed with SAH. However, the overuse of CT angiography (CTA) exposes patients to unnecessary radiation and contrast.[18] Furthermore, the use of CTA leads to the finding of incidental aneurysms which may or may not be clinically significant. This, in turn, may expose the patient to even more unnecessary testing and intervention. In this case, LP has a high diagnostic yield, eliminating the need for neurosurgical consultation or intervention in the majority of cases.[19] The test is both cost-effective and time-efficient and reduces the number of patients exposed to the radiation and contrast associated with angiography.[19]
Pearls and Other Issues
- Xanthochromia is the presence of bilirubin in the CSF.
- This finding can be the only positive marker that a patient is suffering from an acute SAH.
- It is an important finding in distinguishing between traumatic tap and a SAH.
- Visual inspection of the CSF is the most common method of detection.
- Spectrophotometry has been shown to be superior when evaluating for xanthochromia.[9][3][20][9]
Enhancing Healthcare Team Outcomes
The finding of xanthochromia on a spinal tap can be the only evidence to suggest the presence of a subarachnoid hemorrhage. Traditionally, xanthochromia is detected by visualizing the supernatant CSF under incandescent light for the presence of a yellow color. Multiple studies have shown the superiority of using spectrophotometry instead of visualization. Spectrophotometry can detect the presence of xanthochromia at smaller concentrations than the naked eye and is more specific as it relies on the detection of a certain wavelength of emitted light that corresponds to xanthochromia itself. [1],[4],[20] [Level III]
Standard practice in the diagnosis of subarachnoid hemorrhage with a negative head CT still includes the use of lumbar puncture to detect the presence of xanthochromia. This test is more cost effective and may reduce the need for CT angiography with contrast in many patients.[19],[21],[22] [Level IV]