Anatomy, Anterolateral Abdominal Wall Nerves
- Article Author:
- Aurimas Kudzinskas
- Article Editor:
- Bruno Cunha
- Updated:
- 10/28/2020 1:02:43 AM
- For CME on this topic:
- Anatomy, Anterolateral Abdominal Wall Nerves CME
- PubMed Link:
- Anatomy, Anterolateral Abdominal Wall Nerves
Introduction
The anterolateral abdominal wall is the structure that extends from the thorax to the pelvis and contains the abdominal cavity with its associated organs.[1] It plays an important role in the movement of the torso, stabilization of the spine, as a physical barrier and the ability to increase and maintain intra-abdominal pressure.[2][3]
Various pathology including trauma, neoplasm, and infection can affect the anterolateral abdominal wall which can result in a reduction in quality of life. This article will focus on the course, structure, function and clinical implication of the nerves towards and within the anterolateral abdominal wall.
Structure and Function
There is no clear consensus on the boundaries of the anterolateral abdominal wall.[1][4] The anterolateral abdominal wall can be defined as the region within the subcostal (thoracoabdominal) line superiorly, the upper border of the pubis and ileum inferiorly, the posterior axillary line (a vertical line from the posterior corner formed by the latissimus dorsi muscle and the chest wall) posteriorly and continuous anteriorly.[5] It has been proposed to differentiate the lateral abdominal wall from the anterior by a line from the anterior axillary line (a vertical line from the anterior corner of the axilla formed by the pectoralis major and chest wall).[4] The anterolateral abdominal wall from superficial to deep consists of skin, subcutaneous fat (including Camper’s fascia and Scarpa's fascia), abdominal muscles (with their associated fascia and aponeurosis), transversalis fascia and parietal peritoneum.[6][7]
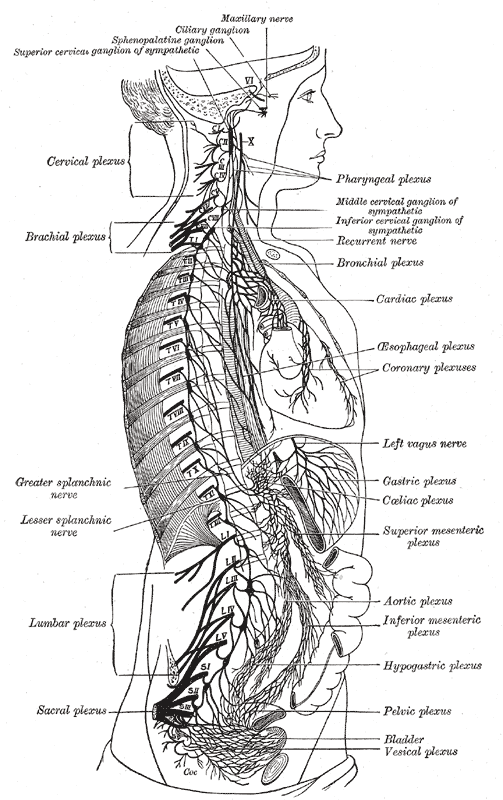
The motor and sensory nerves that are present in the anterolateral abdominal wall consist of the thoracoabdominal, iliohypogastric and ilioinguinal nerves arising from T6 to L1 spinal nerves.[6]
The thoracoabdominal nerves originate as terminal anterior ramus branches of the T7 to T12 spinal nerves.[6] Posterior ramus branches innervate the fine muscles of the spine, zygapophyseal joints and skin overlying the spine. From the T6 to T11 vertebral foramina, the anterior ramus branches of the spinal nerves travel between the pleura of the lungs and the internal intercostal membranes before traveling as the intercostal nerves between the innermost intercostal muscle and the internal intercostal muscle. The intercostal nerves travel in close relation to the inferior border of the ribs. The T12 anterior ramus branch of the thoracic spinal nerve travels as the subcostal nerve inferior to the 12 rib and deep to the costal origin of the quadratus lumborum muscle. At the mid-axillary line, the intercostal nerves and subcostal nerve give off lateral cutaneous branches with T7 and T8 predominantly supplying sensation to the inferior lateral thoracic wall and T9 to T12 predominantly supplying sensation to the lateral abdominal wall. After crossing the subcostal line the intercostal nerves and subcostal nerve enter the abdominal wall as T7 to T12 thoracoabdominal nerves. The thoracoabdominal nerves travel within a neurovascular plane between the transversus abdominis muscle and internal oblique muscle before piercing the posterior rectus sheath and traveling anteriorly through channels in the linea semilunaris to innervate the skin overlying the rectus muscle.[8] Within the abdominal wall the thoracoabdominal nerves travel at an anterior inferior angle so that T7 innervates skin just inferior to the xiphoid process of the sternum, T10 innervates the region of the umbilicus and T12 innervates suprapubic skin. This is also represented by the slightly inferior slope of the dermatomes of the abdominal wall.[1] The T7 to T12 thoracoabdominal nerves segmentally innervate the skin overlying the anterolateral abdominal wall, the intercostal muscles, rectus abdominis muscle, pyramidalis muscle, transversus abdominis muscle, internal oblique muscle, and external oblique muscle.
The iliohypogastric nerve originates from the superior branch of the anterior ramus of the L1 spinal nerve which commonly receives communicating branches from T12.[6][9] The nerve emerges from the lateral border of the psoas major muscle posteriorly and traverses laterally and deep to the quadratus lumborum muscle to pierce the transversus abdominis muscle superior to the iliac crest. Within this neurovascular plane between transversus abdominis muscle and internal oblique muscle, the iliohypogastric nerve gives off a lateral cutaneous branch at the mid-axillary line to supply the skin overlying the buttocks and ileum. As the nerve passes the anterior superior iliac spine superiorly, the nerve pierces the internal oblique muscle to travel between the internal oblique muscle and external oblique muscle continuing its course superior to the inguinal ligament. The iliohypogastric nerve then pierces the external oblique aponeurosis approximately an inch superior to the superficial inguinal ring giving terminal branches to the skin overlying the inferior rectus abdominis muscle. Along its course, the iliohypogastric nerve will innervate the skin over the buttocks, ileum, and skin overlying the inferior portion of the rectus abdominis muscle. It will also send motor branches to the inferior portions of the transversus abdominis, external oblique and internal oblique muscles.
The ilioinguinal nerve originates from the superior branch of the anterior ramus of the L1 spinal nerve.[6] The ilioinguinal nerve emerges from the lateral border of the psoas major muscle posteriorly and traverses laterally and deep to the quadratus lumborum muscle to pierce the transversus abdominis muscle at the iliac crest inferior to the iliohypogastric nerve. The nerve travels within the neurovascular plane between transversus abdominis and internal oblique muscles until it reaches the superficial inguinal ring. The ilioinguinal nerve pierces the internal oblique muscle at the superficial inguinal ring entering the inguinal canal and traveling along the spermatic cord (in males) or the round ligament (in females). The ilioinguinal nerve will innervate the skin overlying the inguinal ligament, inner thigh, mons pubis, scrotum, the root of the penis and labia majora. It will send motor branches to the inferior portions of the transversus abdominis, external oblique and internal oblique muscles.
Embryology
During embryonic development up to 39 paraxial mesoderm somites form on either side of the neural tube at Carnegie Stage (CS) 9 to CS13.[10] Nerves enter adjacent somites and follow the consequent development of the dermatome and myotome.[1][10] At CS15 separate epaxial and hypaxial myotomes are formed with individual ventral and dorsal spinal nerve branches. From CS17 and CS18 spinal nerves originating from the neural tube are seen to penetrate the correspondent myotome. Three separate muscle layers develop as the myotome elongates ventrally at CS18. The fusion of the left and right myotomes at the midline occurs at CS20 to CS23.
Blood Supply and Lymphatics
Within the intercostal space, between the innermost intercostal muscle and internal intercostal muscle, the intercostal and subcostal nerves travel with the concurrent T7 to T12 posterior intercostal arteries as neurovascular bundles.[11] The T7 to T9 posterior intercostal arteries anastomose with the anterior intercostal arteries from the musculophrenic artery. Within the abdominal wall, the T10 and T11 posterior intercostal arteries continue with the thoracoabdominal nerves travel as neurovascular bundles in the abdominal wall.[1]
The anterolateral wall receives arterial supply from inferior epigastric, superficial epigastric, superior epigastric, musculophrenic, posterior intercostal and anterior intercostal arteries.
Venous drainage consists of a large venous plexus that drains into the internal thoracic vein and lateral thoracic vein superiorly and the inferior and superficial epigastric veins inferiorly.
Muscles
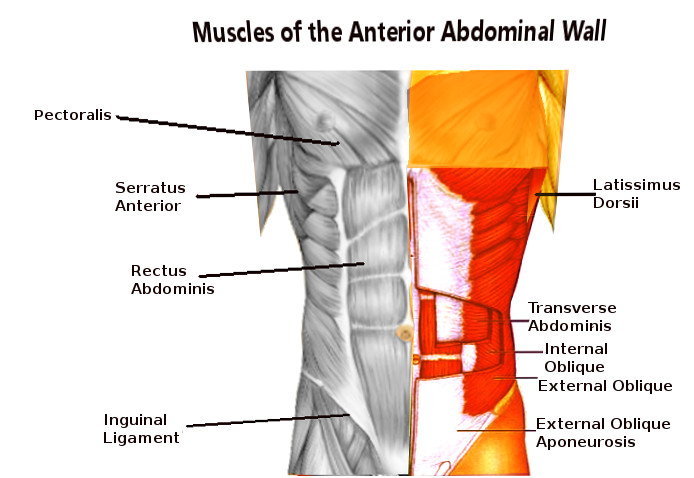
Muscles present in the anterolateral abdominal wall include the transversus abdominis, internal oblique, external oblique, pyramidalis, and rectus abdominis muscles. The rectus abdominis muscle is enclosed by the anterior and posterior rectus sheaths formed by the transversus abdominis, internal oblique, and external oblique aponeurosis. The linea alba separates the left and right rectus abdominis muscles as a combination of the anterior and posterior rectus sheaths. The linea semilunaris forms the lateral enclosure of the recuts abdominis muscles formed by the aponeurosis of the transversus abdominis, internal oblique, and external oblique muscles. The transversus abdominis, external oblique, and internal oblique muscles are layered (deep to superficial respectively) and extend from the lateral border of the rectus abdominis across the remainder of the abdominal wall. These muscles have attachments to the inguinal ligament and form the borders of the inguinal canal. The pyramidalis muscle is a physiological variant and is present in 80% of the population.[7] When present it has great variation, typically being found between the anterior border of the rectus abdominis muscle and the posterior border of the posterior rectus sheath on the lower part of the rectus abdominis muscle.[12]
Surgical Considerations
Specific nerve blocks can be used as an option to provide regional anesthesia by infiltrating local anesthetic around a nerve. Of such the transversus abdominis plane block (between the transversus abdominis and internal oblique muscles) is used to anesthetize the thoracoabdominal, iliohypogastric and ilioinguinal nerves that run in this plane.[13] Ilioinguinal and iliohypogastric nerve blocks can be performed by infiltrating local anesthetic superior to the anterior superior iliac spine.[14] These nerve blocks can be used for surgeries of the inguinal region, typically used in hernia repairs.
An indirect hernia repair can require the manipulation and visualization of the superficial inguinal ring. The ilioinguinal nerve enters the inguinal canal here and can subsequently be damaged resulting in a sensory alteration of the scrotum, root of the penis, labia majora and inner thigh.[15]
The intercostal nerves can be crushed or severed during thoracotomies. This can result in subsequent thoracoabdominal nerve dysfunction, typically causing chronic pain and rectus muscle paresis.[9][16]Thoracic drains can inadvertently damage the intercostal nerves as they travel just inferior to the ribs.[17]
Surgical incisions over the anterolateral abdominal wall pose the risk of nerve damage. Depending on the location of the incision, different nerves can be affected. Pfannenstiel incisions can damage the ilioinguinal and iliohypogastric nerves, while paramedian and subcostal incisions are more likely to damage the thoracoabdominal nerves.[18][19] Incisions running perpendicular to the course of the nerves (anterior inferior angle) will correspond to a larger sensory-motor deficit.
Clinical Significance
Dysfunction of the anterolateral abdominal nerves has the potential to result in abdominal weakness, hernia, chronic pain, movement impairment, sensory loss, and sexual dysfunction. Each of these factors can implicate and reduce the quality of life of an individual.[9][15][16]
Compression of the thoracoabdominal nerves most commonly occurs at the point where the nerves pierce the posterior rectus sheath, here they turn 90% to travel anteriorly through the linea semilunaris.[8] This can result in abdominal cutaneous nerve entrapment syndrome which is often mistreated as gynecological pain.[8][20]
(Click Image to Enlarge)